If you're self-employed, you'll likely need to file Form 124A B with your taxes. This form is used to report income and expenses for a business that's been set up as a sole proprietorship. Knowing how to complete this form accurately is essential for ensuring that you pay the correct amount of taxes on your business income. In this article, we'll walk you through every step of completing Form 124A B. We'll also provide tips for minimizing your tax liability. Let's get started!
| Question | Answer |
|---|---|
| Form Name | Da 124A B Form |
| Form Length | 2 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 30 sec |
| Other names | da 124 ab form, da 124, missouri da124ab, da 124c |
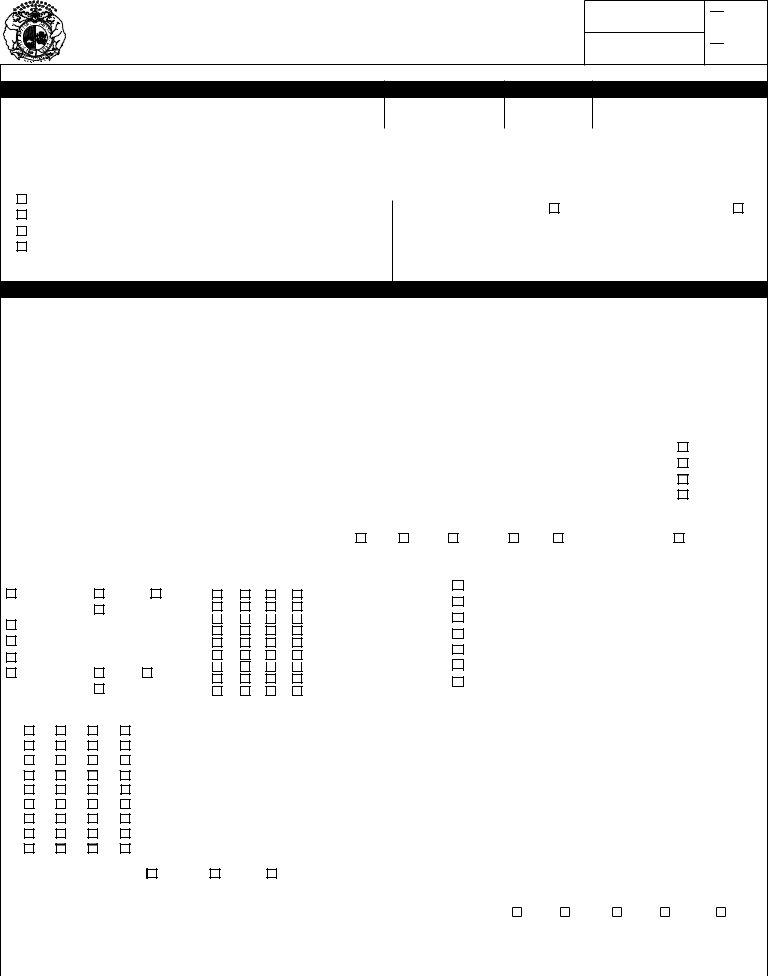
MISSOURI DEPARTMENT OF HEALTH AND SENIOR SERVICES
DIVISION OF REGULATION AND LICENSURE
INITIAL ASSESSMENT - SOCIAL AND MEDICAL
FSD CO. NO.
LOAD NO.
CASH
XIX
All questions on this form must be answered – write N/A if not applicable. Blank areas will result in return of document and delay in payment.
A. SOCIAL ASSESSMENT
1. PERSON'S NAME (LAST, FIRST, MI)
2. DCN
3. DOB
4. SOCIAL SECURITY NUMBER
5. SEX |
|
|
9. CURRENT LOCATION (ADDRESS) |
|
|
|
|
|
|||
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
6. |
RACE |
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
10. NAME OF PROPOSED NURSING FACILITY PLACEMENT, PHONE # |
|
|
|
|
|
7. |
EDUCATION LEVEL |
|
|
|
|
||||||
|
|
|
|
|
|
||||||
7. |
|
|
GRADE SCHOOL |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
||||
11. DATE ADMITTED TO NF |
12. PERSON'S LEGAL GUARDIAN |
|
OR DESIGNATED CONTACT PERSON |
|
|
||||||
7. |
|
|
HIGH SCHOOL |
|
|
|
|||||
|
|
|
|
|
|||||||
|
|
||||||||||
|
|
|
NAME _________________________________________________________________ |
||||||||
7. |
|
|
COLLEGE |
|
|||||||
|
|
|
|||||||||
|
|
|
STREET ADDRESS ______________________________________________________ |
||||||||
7. |
|
|
OTHER |
|
|||||||
|
|
|
|||||||||
|
|
|
CITY __________________________________ STATE ___________ ZIP ___________ |
||||||||
|
|
|
|||||||||
|
|
|
|
|
|
|
|||||
8. OCCUPATION |
|
||||||||||
|
PHONE ________________________________________________________________ |
||||||||||
|
|
|
|
|
|
|
|||||
B. MEDICAL ASSESSMENT
Attach additional sheets of information if necessary.
1. |
HEIGHT |
2. WEIGHT |
|
|
6. RECENT MEDICAL INCIDENTS (i.e., CVA, SURGERY, FRACTURE, HEAD INJURY, ETC., AND GIVE DATE) |
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3. |
B/P |
4. PULSE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
5. DATE OF LAST MEDICAL EXAM |
|
|
RESIDUAL EFFECTS: |
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||
7. SPECIAL LAB TESTS AND |
|
8. PRESCRIPTION DRUGS (DOSAGE AND FREQUENCY, INCLUDING PRNS; SHOULD CORRELATE WITH DIAGNOSES) |
|
|||||||||||||||
7. |
FREQUENCY |
|
|
1. ____________________________________ |
4. __________________________________ |
7. _________________________________ |
|
|||||||||||
|
|
|
|
|
2. ____________________________________ |
5. __________________________________ |
8. _________________________________ |
|
||||||||||
|
|
|
|
|
||||||||||||||
|
|
|
|
|
3. ____________________________________ |
6. __________________________________ |
9. _________________________________ |
|
||||||||||
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||
9. LIST ALL DIAGNOSES (SHOULD CORRELATE WITH MEDICATIONS) (INCLUDE PSYCH DX) |
10. POTENTIAL PROBLEM AREAS AND/OR |
|
11. STABILITY |
|
||||||||||||||
1. |
_____________________________________ |
6. |
_____________________________________ |
10. ADDITIONAL COMMENTS |
|
|
|
|
1. IMPROVING |
|
||||||||
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
||||||||||||
2. _____________________________________ |
7. |
_____________________________________ |
|
|
|
|
|
|
2. STABLE |
|
||||||||
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|||||||||||||||
3. _____________________________________ |
8. |
_____________________________________ |
|
|
|
|
|
|
3. DETERIORATING |
|
||||||||
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|||||||||||||||
4. _____________________________________ |
9. |
_____________________________________ |
|
|
|
|
|
|
4. UNSTABLE |
|
||||||||
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|||||||||||||||
5. _____________________________________ |
10. |
_____________________________________ |
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
12. LEVEL OF CARE REQUESTED BY PERSON'S PHYSICIAN (CHECK ONE)
NF
RCF
ICFMR
MH
SUPPLEMENTAL NC
HOME CARE
13. MENTAL STATUS (CHECK ALL THAT |
|
14. BEHAVIORAL INFORMATION (CHECK ONE BOX |
15. FUNCTIONAL IMPAIRMENT (CHECK ALL THAT APPLY AND GIVE |
|||||||||||||||||||||||||||||||||
12. APPLY) |
|
|
|
|
|
|
|
|
|
|
FOR EACH) |
|
|
RATIONALE) |
|
|
|
|
|
|||||||||||||||||
ORIENTED TO: |
|
|
person, |
|
|
|
place, |
|
NONE MIN MOD MAX |
|
|
|
VISION __________________________________________________ |
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CONFUSED |
|
|
|
HEARING ________________________________________________ |
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
|
|
time |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
WITHDRAWN |
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SPEECH ________________________________________________ |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
HYPERACTIVE |
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
THINKS CLEARLY |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
WANDERS |
|
|
|
AMBULATION ____________________________________________ |
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
LETHARGIC |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SUSPICIOUS |
|
|
|
MANUAL DEXTERITY ______________________________________ |
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
ALERT |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
COMBATIVE |
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TOILETING________________________________________________ |
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SUPERVISED FOR SAFETY |
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
MEMORY: |
|
|
good, |
|
|
|
fair, |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CAUSES MGT. PROBLEMS |
|
|
PATH TO SAFETY |
________________________________________ |
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
poor |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CONTROLLED WITH MEDICATION(S) |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
16. ASSESSED NEEDS (CHECK APPROPRIATE BOX FOR EACH; GIVE RATIONALE PLUS AMOUNT OF STAFF ASSISTANCE NEEDED. (YOU MUST USE GUIDE #1 ON BACK.) |
||||||||||||||||||||||||||||||||||||
NONE MIN MOD |
MAX |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
1. |
MOBILITY __________________________________________________________________________________________________________ |
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
2. |
DIETARY |
__________________________________________________________________________________________________________ |
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
3. |
RESTORATIVE SERVICES ____________________________________________________________________________________________ |
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
4. |
MONITORING ______________________________________________________________________________________________________ |
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
5. |
MEDICATION ______________________________________________________________________________________________________ |
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
6. |
BEHAVIOR/MENTAL COND. __________________________________________________________________________________________ |
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
7. |
TREATMENTS _____________________________________________________________________________________________________ |
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
8. |
PERSONAL CARE __________________________________________________________________________________________________ |
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
9. |
REHAB. SERVICES __________________________________________________________________________________________________ |
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
17. POTENTIAL FOR REHAB |
|
|
|
GOOD |
|
|
|
|
|
FAIR |
|
POOR |
|
|
|
|
CENTRAL OFFICE USE ONLY |
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
LEVEL OF CARE DETERMINATION BY DIVISION HSL CENTRAL |
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
OFFICE |
|
|
|
|
|
18. PATIENT REFERRED BY |
|
|
|
|
|
|
|
|
|
|
|
|
19. FORM COMPLETED BY |
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NAME OF INDIVIDUAL OR AGENCY |
|
|
|
|
|
|
|
|
|
|
|
|
SIGNATURE OF INDIVIDUAL |
|
|
|
|
1 NF |
2 IMR |
3 MH |
4 SNC |
5 NONE |
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
� |
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
ADDRESS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TELEPHONE NUMBER |
|
|
|
|
NEXT EVALUATION DATE |
|
SIGNATURE DATE |
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
TELEPHONE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FAX NUMBER |
DATE |
|
|
STATE PHYSICAN'S CONSULTANT |
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
� |
|
|
|
|
|
MO |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
GUIDE #1 - ASSESSED NEEDS:
1.MOBILITY - individual's ability to move from place to place. Do they require assistive device, physical assist with transfer, mobile only with physical assist or unable to ambulate and/or totally dependent?
2.DIETARY - individual's nutritional requirements and need for assist and/or supervision with meals. Do they have a special diet, require tray set up, cueing, feeding or on tube feedings or IV fluids?
3.RESTORATIVE - specialized services provided to help individual obtain/maintain optimal function potential. Is individual receiving ROM, B & B program, RO, frequency, and amount of assistance required?
4.MONITORING - Observation and assessment of individual's physical and mental condition. This may include routine lab work, I & O, clinitest, acetest, weights and other routine procedures.
5.MEDICATION - A drug regimen of all physician ordered legend and
6.BEHAVIORAL - individual's social or mental activities. Does individual require supervision/guidance or assist due to their behavior? Are they alert, oriented, disoriented, uncooperative, abusive or incapable of
7.TREATMENTS - a systematized course of nursing procedures ordered by the attending physician. What is the treatment and how often is it ordered? Is the treatment
8.PERSONAL CARE - activities of dailing living, including hygiene, personal grooming (dressing, bathing, oral hygiene, hair and nail care, shaving), and bowel anad bladder funcitons. Does daily care require supervision, close supervision or total care?
9.REHABILITATION - restoration of former or normal state of health through medically ordered therapeutic services either directly
provided by or under the supervision of a qualified professional, which may include PT, OT, ST and audiology. What type of rehab is individual receiving and how often do they receive it?
NOTE: Refer to State of Missouri
GUIDE #2 - INSTRUCTIONS (for
A.NURSING FACILITY ADMISSIONS FROM HOSPITALS–
1.If the person is hospitalized and will or MAY seek placement in a Medicaid certified bed within a skilled or intermediate nursing facility upon discharge, the hospital completes the Level One (I) Screening
2.In Missouri, Federal & State regulations require that Level II Screenings be completed PRIOR to nursing facility placement EXCEPT when a person qualifies for a SPECIAL ADMISSION CATEGORY (follow directions on
B.NURSING FACILITY ADMISSIONS FROM HOME OR RCF–
1.Skilled/intermediate nursing facilities receiving persons directly from home should assist families in completing the Level I Screening
2.EMERGENCY ADMISSIONS FROM HOME OR
3.All Medicaid certified beds, including swing beds, within skilled/intermediate nursing facilities MUST have a completed
C.NURSING FACILITY TRANSFERS–
1.When persons transfer from one skilled/intermediate nursing facility to another, the sending facility furnishes a copy of their DA- 124A/B & C forms to the receiving facility. The receiving facility then notifies their local FSD office of the transfer.
2.When persons transfer from one skilled/intermediate nursing facility to another and application for Medicaid is not indicated, the ORIGINAL
D.TRANSFERS FROM A FACILITY TO A HOSPITAL TO ANOTHER FACILITY–
1.When the person transfers from one skilled/intermediate facility to a hospital, then to another skilled/intermediate facility, hospitals must consider the following prior to placement:
a.If the person did not need a Level II Screening prior to placement at the sending facility, no new forms are indicated if this hospital stay does not exceed 60 days (unless a current Level I Screening indicates the need for a Level II Screening).
b.If the person had a Level II Screening prior to placement at the sending facility, but is being hospitalized for acute medical treatment, no new forms are necessary if the hospital stay does not exceed 60 days.
c.If the person had a Level II Screening prior to placement at the sending facility, and this hospitalization involves a change in the person's mental status, the hospital completes a new
skilled/intermediate nursing facility (if the person stays less than 60 days). That nursing facility sends the new form to COMRU, as in section A, #1. NOTE: If the person stays more than 60 days, the HOSPITAL completes new set of
E.PERSON IS DISCHARGED HOME BUT UNABLE TO STAY–
1.If person is out of facility less than 60 days, no new forms are required. Notify local FSD office of person's readmission.
MO