If you want to fill out 1915i pdf louisiana, you won't have to download and install any applications - just give a try to our online tool. FormsPal is dedicated to providing you with the absolute best experience with our editor by continuously introducing new features and upgrades. With these updates, working with our tool becomes easier than ever! Starting is effortless! All that you should do is stick to the following easy steps below:
Step 1: Simply press the "Get Form Button" above on this webpage to start up our form editor. There you will find everything that is necessary to fill out your document.
Step 2: This tool enables you to change PDF forms in many different ways. Change it by including personalized text, correct original content, and place in a signature - all when it's needed!
Filling out this form typically requires thoroughness. Ensure every single blank field is filled in accurately.
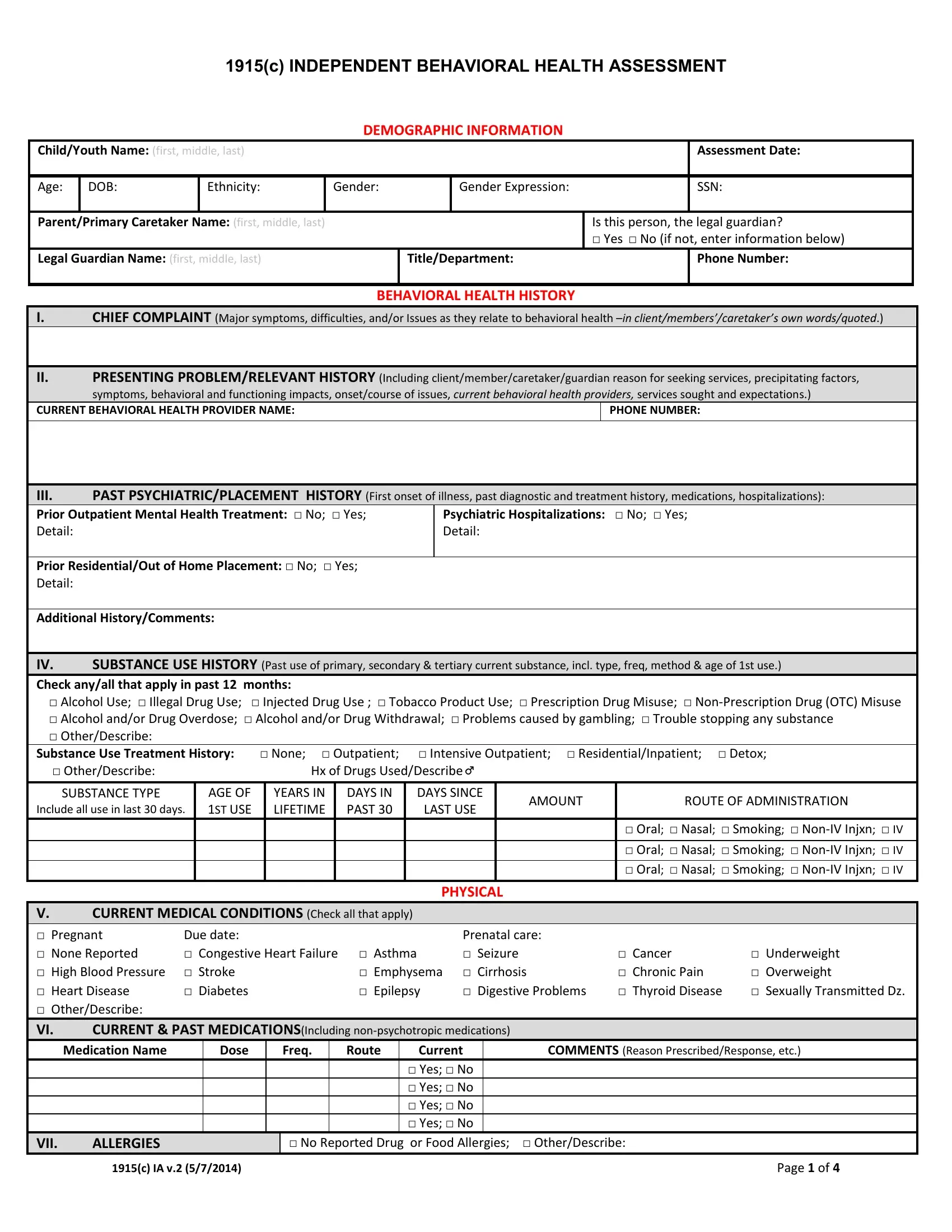
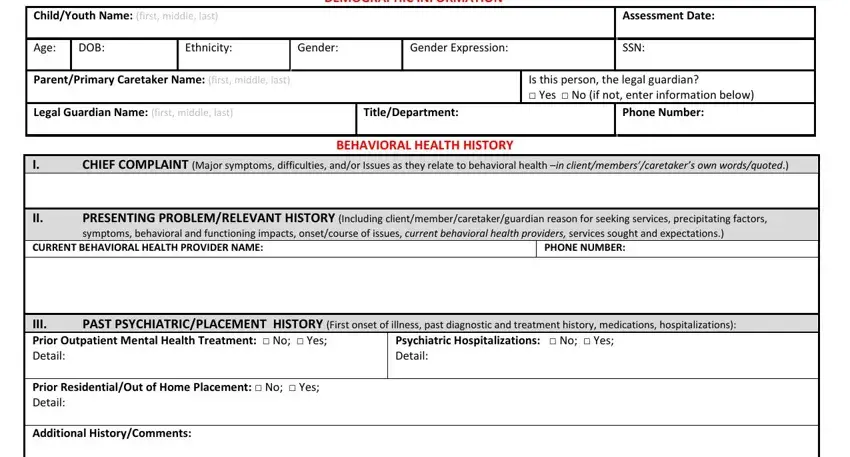
1. To get started, once completing the 1915i pdf louisiana, beging with the form section that features the subsequent blanks:
2. The third step is to submit the next few fields: IV Check anyall that apply in past, SUBSTANCE TYPE, Include all use in last days, AGE OF ST USE, YEARS IN LIFETIME, DAYS IN PAST , DAYS SINCE LAST USE, PHYSICAL, AMOUNT, ROUTE OF ADMINISTRATION, Oral Nasal Smoking NonIV Injxn, CURRENT MEDICAL CONDITIONS Check, Due date Congestive Heart Failure, Prenatal care Asthma Seizure , and Digestive Problems.
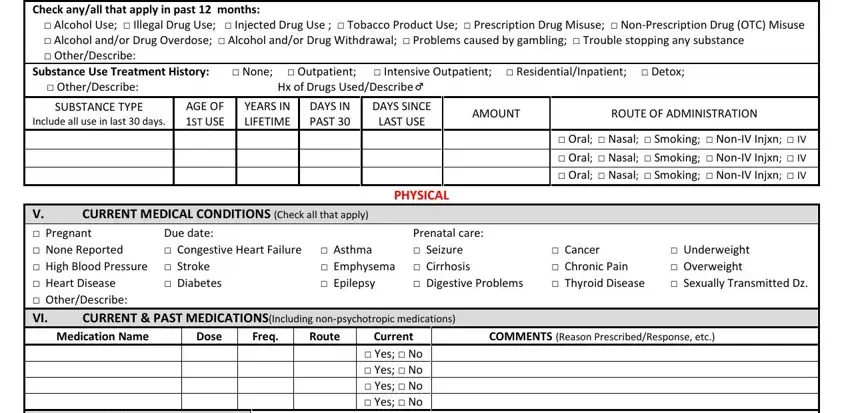
3. This next part focuses on VII, ALLERGIES, No Reported Drug or Food, c IA v , and Page of - type in all of these fields.
It's easy to make an error while completing your No Reported Drug or Food, hence you'll want to take a second look before you decide to submit it.
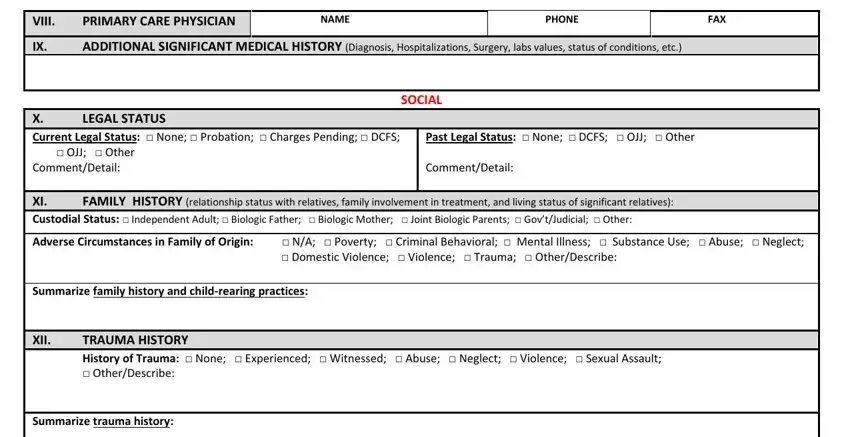
4. This next section requires some additional information. Ensure you complete all the necessary fields - VIII, PRIMARY CARE PHYSICIAN, NAME, PHONE, FAX, ADDITIONAL SIGNIFICANT MEDICAL, SOCIAL, LEGAL STATUS, X Current Legal Status None , OJJ Other, Past Legal Status None DCFS OJJ, CommentDetail XI Custodial Status , FAMILY HISTORY relationship status, CommentDetail, and Domestic Violence Violence - to proceed further in your process!
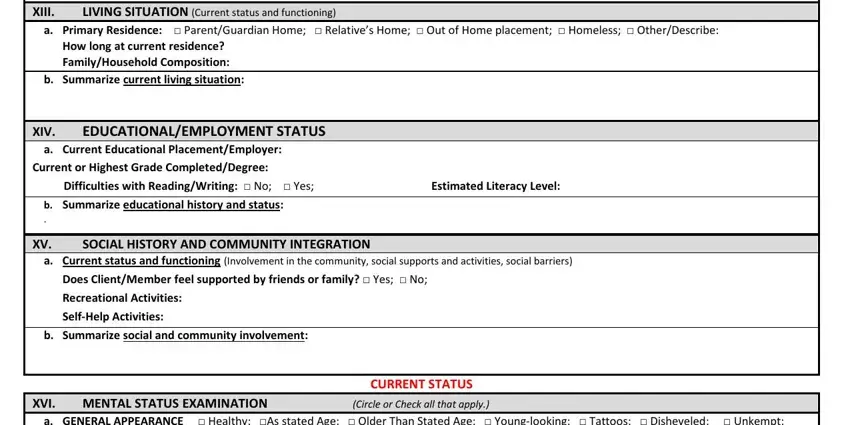
5. The final section to conclude this PDF form is integral. Make certain to fill out the displayed blank fields, consisting of Summarize trauma history XIII, LIVING SITUATION Current status, a Primary Residence , How long at current residence, b Summarize current living, XIV, EDUCATIONALEMPLOYMENT STATUS, a Current Educational, Current or Highest Grade, Estimated Literacy Level, b Summarize educational history, SOCIAL HISTORY AND COMMUNITY, a Current status and functioning, Does ClientMember feel supported, and SelfHelp Activities, before finalizing. Failing to do so may generate an unfinished and potentially incorrect form!
Step 3: Prior to finalizing this document, make certain that form fields are filled in the right way. The moment you determine that it is fine, click on “Done." Join FormsPal right now and immediately gain access to 1915i pdf louisiana, prepared for downloading. All adjustments made by you are kept , helping you to change the document at a later time when necessary. When using FormsPal, you'll be able to fill out forms without having to worry about personal information breaches or records being distributed. Our secure platform helps to ensure that your personal data is kept safely.