In case you desire to fill out PICC, you don't have to download and install any applications - just make use of our online tool. Our editor is consistently evolving to deliver the very best user experience possible, and that's due to our resolve for continual improvement and listening closely to comments from users. It merely requires just a few basic steps:
Step 1: Click the "Get Form" button above on this page to open our editor.
Step 2: With the help of our state-of-the-art PDF tool, you'll be able to do more than simply fill in blanks. Edit away and make your documents seem perfect with customized text incorporated, or tweak the file's original content to excellence - all that comes with an ability to insert almost any photos and sign the PDF off.
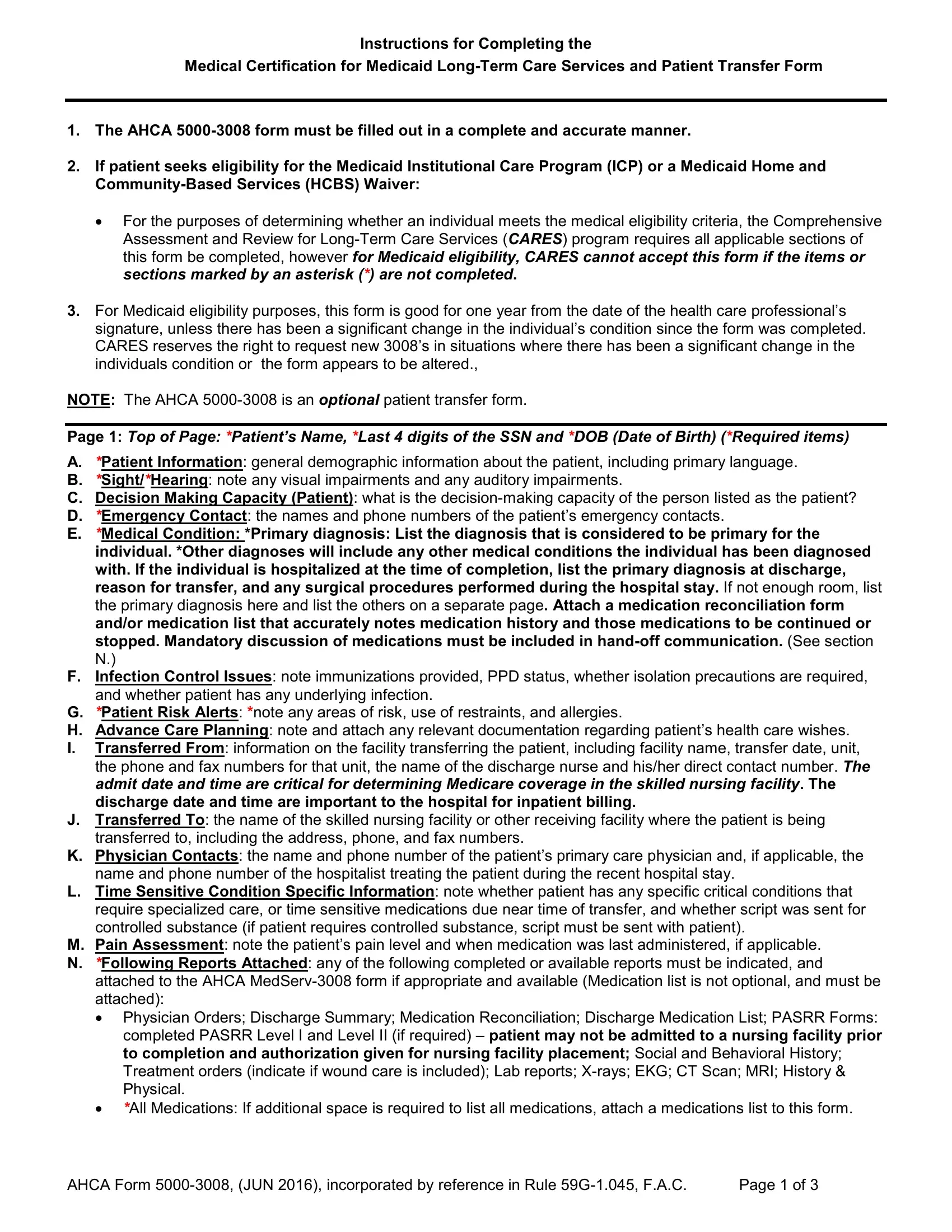
So as to complete this PDF document, be certain to enter the right information in each field:
1. While completing the PICC, make certain to include all essential blank fields within its associated section. It will help to expedite the work, making it possible for your details to be processed swiftly and appropriately.
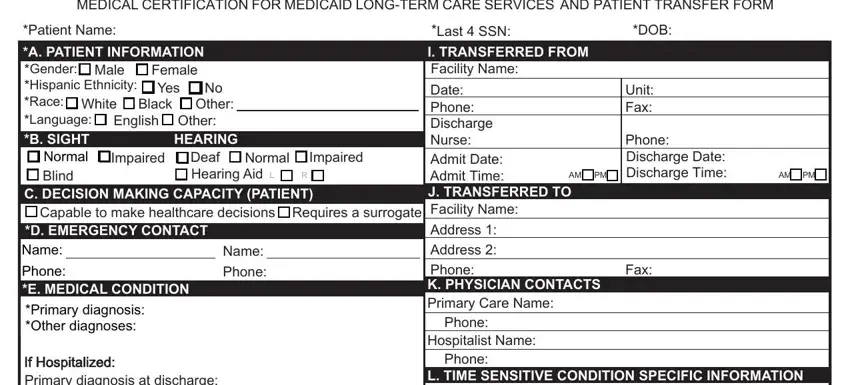
2. Once your current task is complete, take the next step – fill out all of these fields - L TIME SENSITIVE CONDITION, AnticoagulantsDate Antibiotics, Time Time Time Time, Has CHF diagnosis If yes, Yes, Yes, Last echocardiogram Date, LVEF, On a proton pump inhibitor If yes, Yes, Inhospital prophylaxis and can be, IfHospitalized, Negative, Not known, and MRSA VRE ESBL MDRO CDiff Other with their corresponding information. Make sure to double check that everything has been entered correctly before continuing!
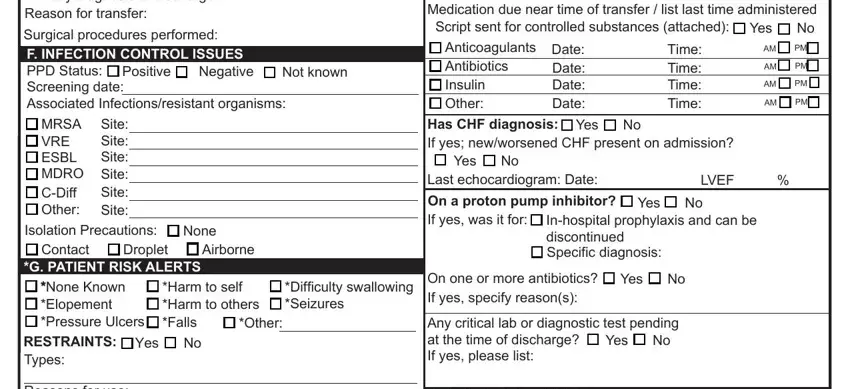
3. Completing Reasons for use, ALLERGIES, None Known, Yes List below, Latex Allergy, Yes, Dye AllergyReaction, Yes, H ADVANCE CARE PLANNING Please, Advance Directive Living Will DO, Yes Yes Yes Yes Yes Yes Yes, No No No No No No No, M PAIN ASSESSMENT Pain Level, Time, and AM PM is essential for the next step, make sure to fill them out in their entirety. Don't miss any details!
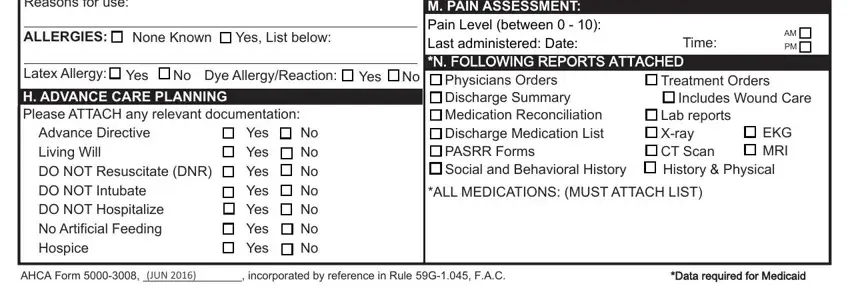
4. This next section requires some additional information. Ensure you complete all the necessary fields - MEDICAL CERTIFICATION FOR MEDICAID, Patient Name O VITAL SIGNS Date, Time Taken, HT Temp, FEET, INCHES, HR P PATIENT HEALTH STATUS Bladder, Catheter Type, Continent, Incontinent, Sp, dateinserted, LastSSN T SKIN CARE STAGE , DOB, and Pressure Ulcers Indicate stage and - to proceed further in your process!
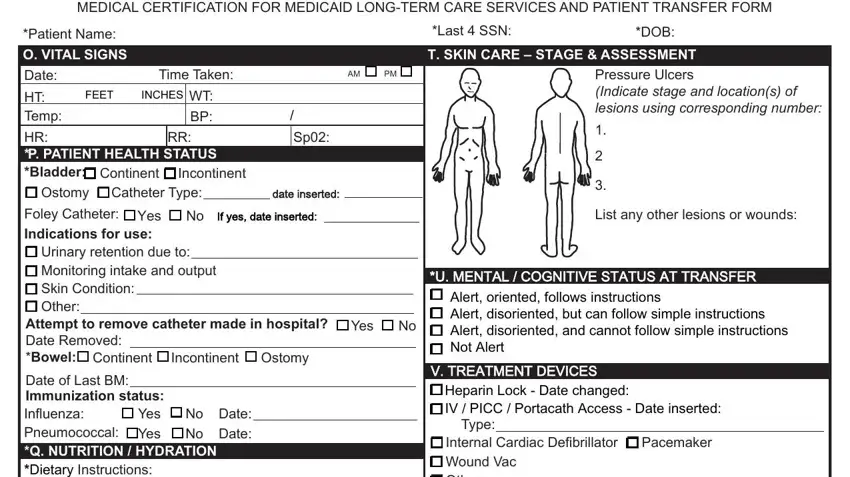
When it comes to FEET and Incontinent, be certain that you don't make any mistakes in this section. Both of these are the key fields in this PDF.
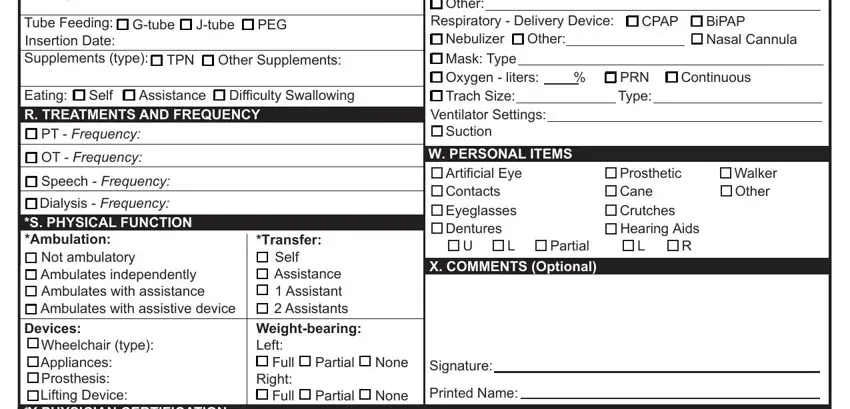
5. To conclude your document, the particular area features a number of extra blank fields. Entering Attempt to remove catheter made in, Internal Cardiac Defibrillator, Gtube, Jtube, PEG, Respiratory Delivery Device, CPAP, BiPAP Nasal Cannula, Tube Feeding Insertion Date, TPN, Other Supplements, Eating R TREATMENTS AND FREQUENCY, Assistance, Self, and Difficulty Swallowing will certainly finalize everything and you can be done in a tick!
Step 3: Prior to finalizing this form, ensure that all blanks were filled out correctly. When you think it's all fine, click on “Done." Make a free trial subscription with us and gain direct access to PICC - download or edit inside your personal account. When you use FormsPal, it is simple to complete documents without stressing about information leaks or entries being shared. Our protected system makes sure that your personal information is kept safe.


 Capable to make healthcare decisions
Capable to make healthcare decisions Requires a surrogate
Requires a surrogate Positive
Positive Negative
Negative  Not known Screening date:
Not known Screening date:




 None Known
None Known 
 Yes, List below:
Yes, List below:
 Yes
Yes 
 No
No



