Using our PDF editor to complete a clinical incident report provides a convenient and efficient way to manage documentation for patient care issues.
If you work in healthcare or an administrative role, ensuring this document is accurately completed is critical for compliance, quality control, and ongoing training needs.
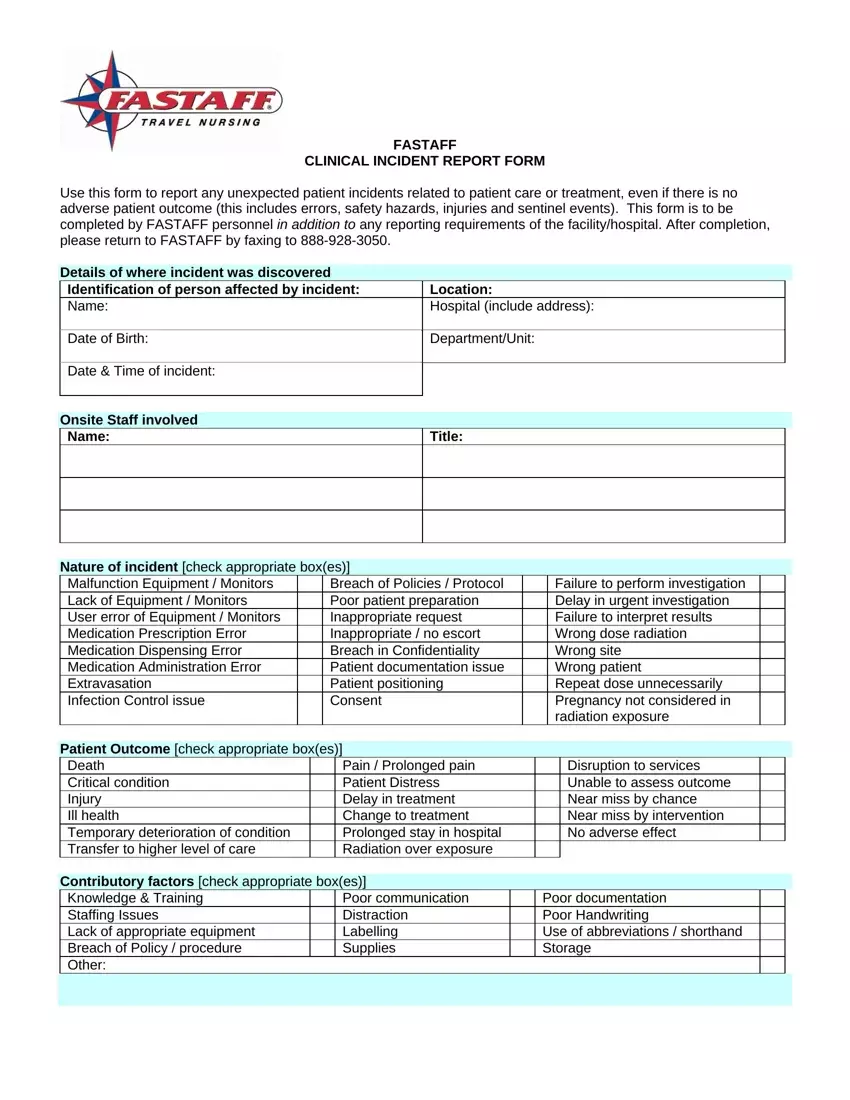
1. Enter Patient Identification Details
Input the patient's name, location within the hospital, date of birth, and any other identifying details requested in the form.
2. Document the Incident Specifics
Record the department or unit where the incident occurred and the precise date and time. Accurate timing can be crucial for subsequent reviews or legal considerations.
3. Describe the Nature of the Incident
Check the appropriate boxes that describe the nature of the incident. The form includes options such as equipment malfunctions, medication errors, and breaches of confidentiality.
4. Note Onsite Staff and Witnesses
List the names and titles of any staff members involved in or witnesses to the incident. This information is essential for follow-up interviews and determining the incident's scope.
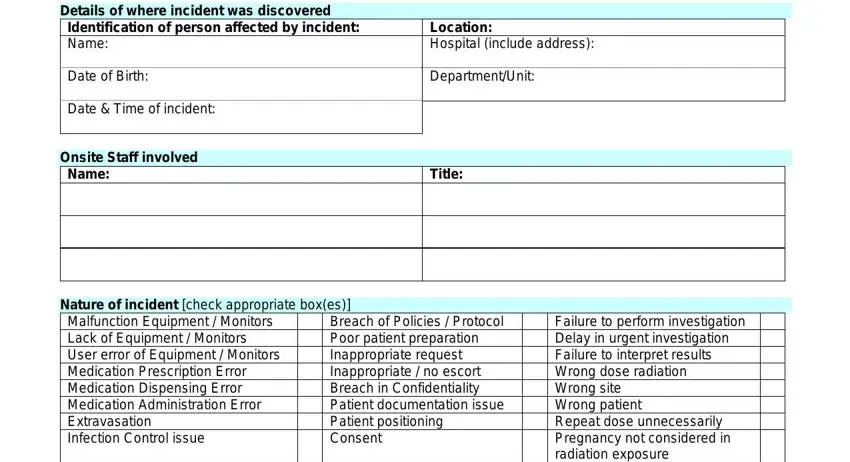
5. Indicate the Patient Outcome
Specify the outcome for the patient using the checkboxes provided, such as injury, critical condition, or no adverse effect. Understanding the immediate impact on safety for the patient helps assess the incident's severity.
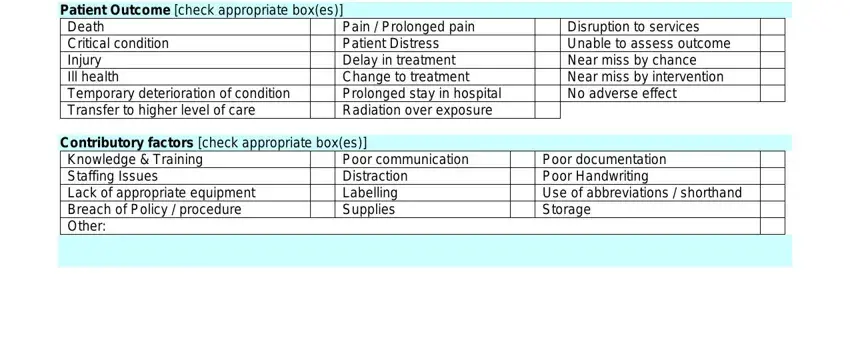
6. Identify Contributory Factors
Identify and check off all events leading to the incident, like staffing issues or equipment lack. Recognizing these factors helps to implement preventive measures.
7. Provide a Summary of the Incident
Provide a clear and factual summary of what happened during the incident. Attach additional sheets if necessary to ensure a comprehensive written account.
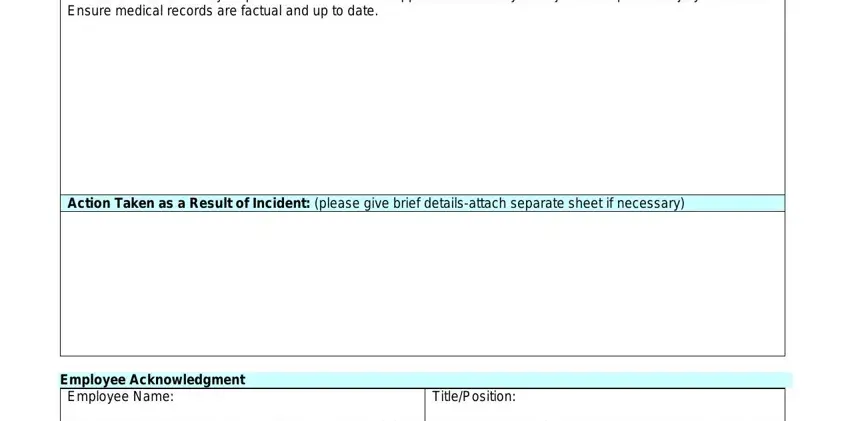
8. Detail Actions Taken
Document any immediate actions taken in response to the incident to address and mitigate its effects. It could include medical treatments provided, additional supervision, or other corrective actions.
9. Employee Acknowledgment
As the reporting individual, fill in your name and position and sign off on the report to acknowledge that the information recorded is accurate.
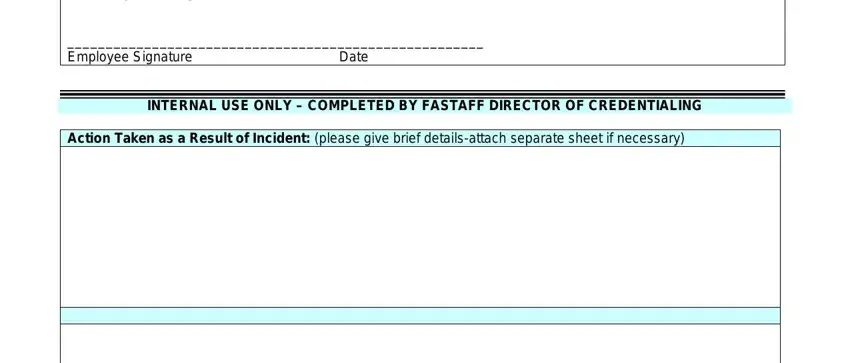
10. Submit the Report
Once completed, the form should be submitted according to your healthcare facility's protocol, including faxing or uploading through a secure incident reporting system.