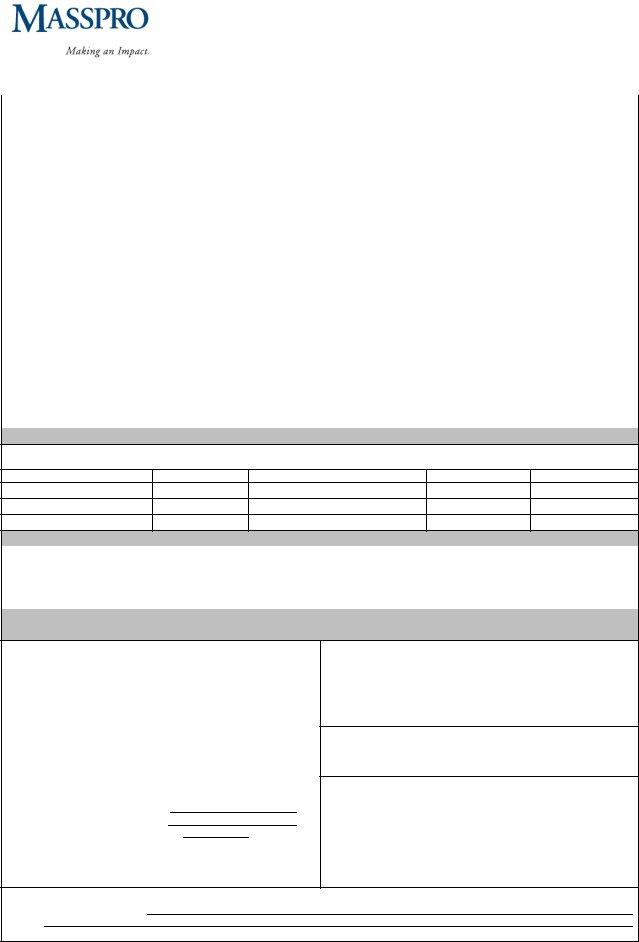
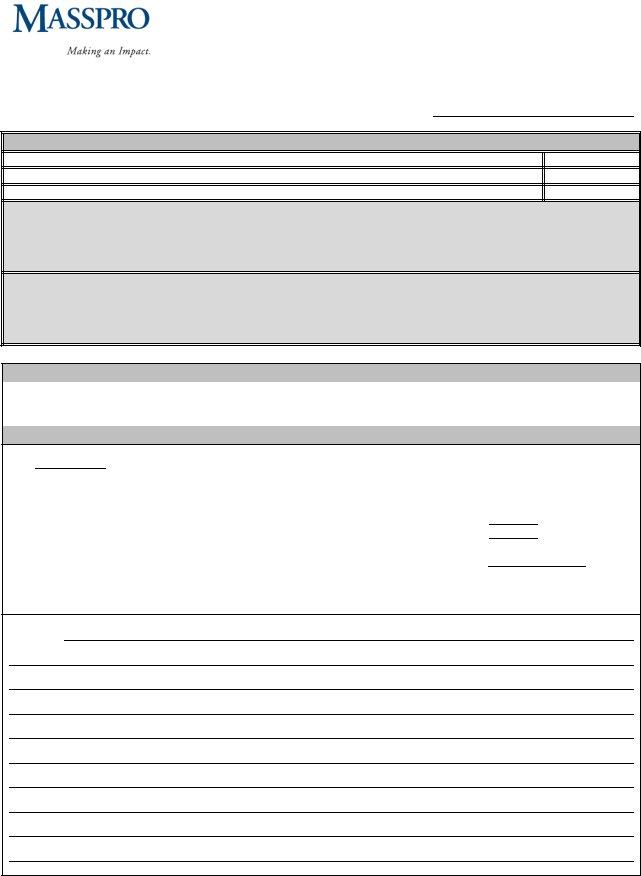
Navigating the complexities surrounding the care of individuals who require admission into nursing facilities, the Colorado Post Admission Level 1 Pre-Admission Screening and Resident Review (PASRR) form stands out as a comprehensive tool designed to ensure that the specific needs of each person are meticulously assessed and addressed. This form is integral in identifying whether individuals have major mental illnesses, mental disorders, symptoms that impact their day-to-day functioning, and any histories of psychiatric treatment, which are crucial factors in determining the level of care and services they require. It delves into the presence of dementia, outlining the necessity for corroborative testing or additional information to verify and understand the progression of such conditions. Moreover, the document gathers details on psychotropic medications, shining a light on the dosages and whether they exceed recommended limits. The form also touches upon mental retardation and developmental disabilities, seeking to understand the individual's historical context and current cognitive or behavioral impairments. Decisions regarding exemption and categorical determinations are addressed, highlighting criteria for hospital exemption, terminal illness, severity of illness, and convalescence. The PASRR form is a vital step in ensuring individuals receive the appropriate level of care in nursing facilities, tailoring interventions and services to meet their specific health needs while adhering to regulatory and compliance standards.
| Question | Answer |
|---|---|
| Form Name | Colorado Post Admission Level 1 Passr Form |
| Form Length | 3 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 45 sec |
| Other names | colorado pasrr, colorado pasrr level 1, print pasrr form, colorado pasrr form |

COLORADO LE VE L I F ORM
First Name: |
|
|
Middle Initial: |
|
|
Last Name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
Mailing Address: |
|
|
|
|
|
|
|
|
|
|
|
City: |
|
|
|
|
|
|
|
|
|
|
|
|
State: |
Zip: |
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
Phone: |
|
|
Social Security #: |
|
- |
|
|
|
|
- |
|
|
|
Date of Birth: |
/ |
|
|
/ |
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
Gender: c Male c Female Race: c Caucasian c African American c Asian c Hispanic c Other: |
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||
Current Location: c*Medical Facility c*Psychiatric Facility c *Nursing Facility c Community c Other: |
|||||||||||||||||||||||||||||||||||||||||||||
*Provide Admission Date: |
|
|
|
|
|
|
|
|
|
|
Receiving Nursing Facility: |
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||
Receiving Nursing Facility Address: |
|
|
|
|
|
|
|
|
|
|
|
|
City: |
|
|
|
State: |
|
Zip: |
|
|
|
|
|
|
||||||||||||||||||||
Payment Method: c Medicare c Private Pay c Medicaid c Medicaid Pending c Medicaid # |
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||
c Hospice c PACE c 30 Day PACE Respite |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
** Provide ULTC Scores if Medicaid or Medicaid Pending: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
Bathing |
|
Dressing |
|
|
|
Toileting |
|
|
Mobility |
|
|
|
Transfer |
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
Eating |
Supervision Behaviors |
|
Supervision Memory/Cognition |
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
Section I: MENTAL ILLNESS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
1. Does the individual have any of the |
|
2. |
Does the individual have any of the |
|
3. Does the individual have a diagnosis of |
||||||||||||||||||||||||||||||||||||||||
following Major Mental Illnesses |
|
|
following mental disorders? |
|
|
|
|
|
|
|
|
a mental disorder that is not listed in |
|||||||||||||||||||||||||||||||||
(MMI)? |
|
|
|
|
|
|
c No |
|
|
|
|
|
|
|
|
|
|
|
|
#1 or #2? (do not list dementia here) |
|||||||||||||||||||||||||
c No |
|
|
|
|
|
|
c Suspected: One or more of the |
|
|
|
c No |
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||
c Suspected: One or more of the |
|
|
|
|
following diagnosis is suspected |
|
|
|
c Yes (if yes, enter the diagnosis(es) |
||||||||||||||||||||||||||||||||||||
|
following diagnoses is suspected |
|
|
|
|
(check all that apply) |
|
|
|
|
|
|
|
|
below): |
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
(check all that apply) |
|
|
|
|
|
|
c Yes: (check all that apply) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
c Yes: (check all that apply) |
|
|
|
c Personality Disorder |
|
|
|
|
|
|
|
|
c Diagnosis 1: |
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
c Schizophrenia |
|
|
|
|
|
|
c Anxiety Disorder |
|
|
|
|
|
|
|
|
|
|
|
c Diagnosis 2: |
|
|
|
|
|
|
|
|
|
|||||||||||||||||
c Schizoaffective Disorder |
|
|
|
c Panic Disorder |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
c Major Depression |
|
|
|
|
|
|
c Depression (mild or situational) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
c Psychotic/Delusional Disorder |
|
|
|
|
(provide GDS Score: |
) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||
c Bipolar Disorder (manic depression) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
c Paranoid Disorder |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
Section II: SYMPTOMS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
4. |
|
5. Concentration/Task related |
|||||||||||||||||||||||||||||||||||||||||||
individual exhibited interpersonal symptoms or behaviors [not |
|
|
the past 6 months, has the individual exhibited any of the |
||||||||||||||||||||||||||||||||||||||||||
due to a medical condition]?: c No c Yes |
|
|
|
|
|
|
|
|
|
|
|
following symptoms or behaviors [not due to a medical |
|||||||||||||||||||||||||||||||||
c Serious difficulty interacting with others |
|
|
|
|
|
|
|
|
|
|
condition]? c No |
c Yes |
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||
c Altercations, evictions, or unstable employment |
|
|
c Serious difficulty completing tasks that she/he should be |
||||||||||||||||||||||||||||||||||||||||||
c Frequently isolated or avoided others or exhibited signs |
|
|
capable of completing |
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||
|
suggesting severe anxiety or fear of strangers |
|
|
c Required assistance with tasks for which she/he should be |
|||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
capable |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c Substantial errors with tasks in which she/he completes |
||||||||||||||||||||||||
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||
Adaptation to change |
|||||||||||||||||||||||||||||||||||||||||||||
adapting to change? c No (proceed to Section III) c Yes (complete |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||
6. c Self injurious or self |
7. c Severe appetite disturbance |
|
8. |
c Other major mental health symptoms (this may include |
|||||||||||||||||||||||||||||||||||||||||
mutilation |
c Hallucinations or delusions |
|
|
|
|
recent symptoms) that have emerged or worsened as a result |
|||||||||||||||||||||||||||||||||||||||
c Suicidal talk |
c Serious loss of interest in things |
|
|
|
|
of recent life changes as well as ongoing symptoms. |
|||||||||||||||||||||||||||||||||||||||
c History of suicide |
c Excessive tearfulness |
|
|
|
|
||||||||||||||||||||||||||||||||||||||||
|
|
|
|
Describe symptoms: |
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||
attempt or gestures |
c Excessive irritability |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
c Physical violence |
c Physical threats (no potential for |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
c Physical threats (with |
harm) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
potential for harm) |
GDS Score: |
|
|
|
(if any areas in #7 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
are marked) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Masspro s 245 Winter St. s Waltham, MA 02451 s Phone:
COLORADO LE VE L I F ORM
Patient Last Name: |
|
|
|
|
|
|
|
|
|
|
|
Patient First Name: |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
Section III: HISTORY OF PSYCHIATRIC TREATMENT |
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
9. Currently or within the past 2 years , has the individual |
|
|
10. Currently or within the past 2 years, has the individual |
|
|||||||||||||||||||||
received any of the followingmental health services? |
|
|
|
experienced significant life disruption because of mental health |
|
||||||||||||||||||||
|
c No |
|
|
|
|
|
|
|
|
|
|
symptoms? c No c Yes (check all that apply): |
|
|
|
||||||||||
|
c Yes (the individual has received the following service[s]): |
|
|
c Legal intervention due to mental health symptoms |
|
||||||||||||||||||||
|
c Inpatient psychiatric hospitalization (if yes, provide |
|
|
|
(date: |
|
|
) |
|
|
|
|
|
|
|
||||||||||
|
date: |
|
|
) |
|
|
|
|
|
|
|
c Housing change because of mental illness |
|
|
|
||||||||||
|
c Partial |
hospitalization/ day treatment (if yes, provide |
|
|
(date: |
|
|
) |
|
|
|
|
|
|
|
||||||||||
|
date: |
|
|
) |
|
|
|
|
|
|
|
c Suicide attempt or ideation (date[s]: |
|
|
) |
|
|||||||||
|
cResidential treatment (if yes, provide date: |
|
) |
|
|
c Other: |
|
|
(date: |
|
) |
|
|
||||||||||||
|
c Other: |
|
|
|
|
|
(if yes, |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
provide date: |
|
) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|||||||||||||||||
11. |
Has the individual had a recent psychiatric/behavioral evaluation? |
c No c Yes (date: |
|
|
) |
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
Section IV: DEMENTIA |
|
|
|
|
|
|
|
|
|
||||||||
12. |
Does theindividual have a diagnosis |
|
13. If yes to #12, is corroborative testing or other information available to verify the presence |
|
|||||||||||||||||||||
|
of dementia or Alzheimer’s disease? |
|
or progression of the dementia? |
|
|
|
|
|
|
|
|
|
|||||||||||||
|
c No (proceed to 15) c Yes |
|
c No c Yes (check all that apply) |
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
c Dementia work up c Comprehensive Mental Status Exam |
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
c Other (specify): |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
14.If yes to12, list currently prescribed antidepressant or antipsychotic medications listed on the Beer’s List.
|
|
|
|
|
|
Medication |
Dosage MG/Day |
Refer to Beer’s List |
|
|
|
|
|
Does dosage exceed Beer’s List? cNo cYes |
|
|
|
|
|
|
|
|
|
Does dosage exceed Beer’s List? cNo cYes |
|
|
|
|
|
|
|
|
|
Does dosage exceed Beer’s List? cNo cYes |
|
|
|
|
|
Section V: PSYCHOTROPIC MEDICATIONS
15.Has the individual been prescribed psychoactive (mental health) medications now or within the past 6 months other than those listed in question 14? c No c Yes (list below) [use separate sheet if necessary] *Do not list medications if used for a medical diagnosis.
Medication
Dosage MG/Day
Diagnosis
Started
Ended
Section VI: MENTAL RETARDATION & DEVELOPMENTAL DISABILITIES
16. |
Does the individual have a diagnosis of mental retardation |
17. |
Does the individual have any history of MR or DD? c No c Yes |
||
|
(MR) or developmental disability (DD)? c No c Yes |
|
|
|
|
|
|
|
|
||
18. |
Is there presenting evidence of a cognitive or behavioral |
19. |
Has the individual ever received services from an agency that |
||
|
impairment prior to age 22 or suspicion of MR condition that |
|
serves people affected by MR/DD? c No |
||
|
occurred prior to age 18? c No c Yes |
|
c |
||
|
|
|
|
|
|
Section VII: EXEMPTION AND CATEGORICAL DECISIONS
(MASSPRO MUST APPROVE USE OF CATEGORIES AND EXEMPTION PRIOR TO ADMISSION)
20.Does the admission meet criteria for Hospital Exemption? c No
c Yes (meets all the following andhas a known or suspected MMI or MR/DD):
∙Admission to NF directly from hospital after receiving acute medical care, and
∙Need for NF is required for the condition treated in
the hospital (specify condition: |
, ) |
|
and |
|
|
∙The attending physician has certified prior to NF admission the individual will require less than 30 calendar days of NF services and the individual’s symptoms or behaviors are stable.
Physician Name: Physician Phone: Physician License #:
22.Does the admission meet the criteria for Terminal Illness? c No
c Yes (Has a known or suspected MMI or MR/DD and MD has certified in writing that the patient has 6 months or less to live. The physician signed certification must be submitted to Masspro via facsimile within 6 business hours of submission of this form)
23.Does the admission meet the criteria for Severity of Illness?
cNo
cYes (Has a known or suspected MMI or MR/DD and is ventilator dependent or comatose unresponsive)
24.Does the admission meet criteria for 60 day Convalescence? c No
c Yes (meets all the following and has a known or suspected MMI or MR/DD): c Admission to NF directly from hospital after receiving acute medical care; and c Need for NF is required for the condition treated in the hospital, and cThe attending physician has certified prior to NF admission the individual will require less than 60 calendar days of NF services.
21. Additional Comments:
Masspro s 245 Winter St. s Waltham, MA 02451 s Phone:
COLORADO LE VE L I F ORM
Patient Last Name: |
|
Patient First Name: |
Section VIII: OUTCOME
25. Are any of the following numbers marked yes or, if applicable, suspected 1, 3, 6, 7, 8, 9, 10, 14, 15, 16, 17, 18,or 19?
26. Check yes if #2 is marked yes or suspected and any areas in
27. Check yes if #4 or 5 or (any areas in) #7 are marked affirmatively and #12 is no
28. Are any of the
cNo (if No, NO further screening is required. Proceed to Section IX)
cYes (Screening information must be submitted to Masspro via fax at
required).
Provide a copy of this form to the individual and, if applicable, guardian.
Does the individual have a legal guardian? c No legal guardian c Yes, legal guardian information is below:
Guardian Last Name: |
|
|
|
First Name: |
|
|
|
|||
Street: |
|
|
City: |
|
|
|
State: |
|
Zip: |
|
Section IX: SOURCE SIGNATURE
Print Name: |
Signature: |
Date: |
/ |
/ |
|
|
|
|
|
Agency/Facility: |
Phone: |
Fax: |
|
|
|
|
|
|
|
Section X: MASSPRO OUTCOME: MASSPRO USE ONLY
Date:
Level I Approved: |
PASRR Authorization #: |
|
|
|
|||
c No MMI/DD |
|
|
|
|
|
|
|
c |
c PACE Respite |
|
c 30 Day Exemption |
||||
c Hospice |
|
|
c Convalescent Care |
|
c Terminal |
||
c Severity of Illness |
|
|
|
|
|
|
|
c |
|
|
|
c |
|||
Level II Referred: |
|
c MI |
c MR/DD |
c Dual |
|
|
|
Comments:
Masspro s 245 Winter St. s Waltham, MA 02451 s Phone: