Our top rated computer programmers worked hard to design the PDF editor we are happy to present to you. The app makes it possible to shortly create form 8584 get and will save you valuable time. You just have to stick to this particular guide.
Step 1: The initial step would be to select the orange "Get Form Now" button.
Step 2: Right now, it is possible to modify your form 8584 get. The multifunctional toolbar makes it possible to include, eliminate, adapt, highlight, and also perform several other commands to the content and areas inside the form.
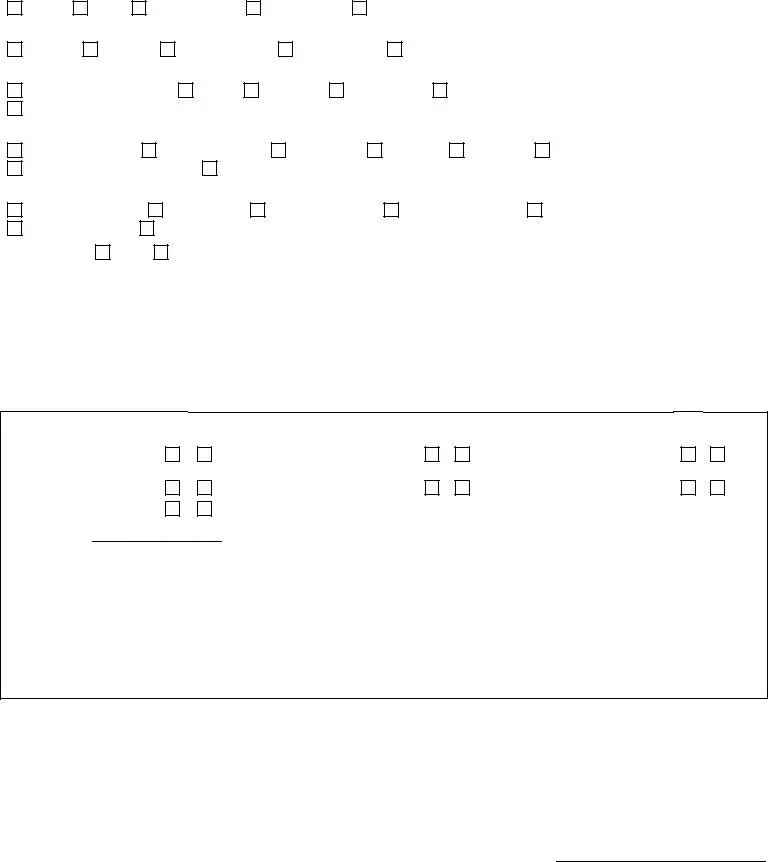
The next parts are what you are going to fill out to get your finished PDF form.
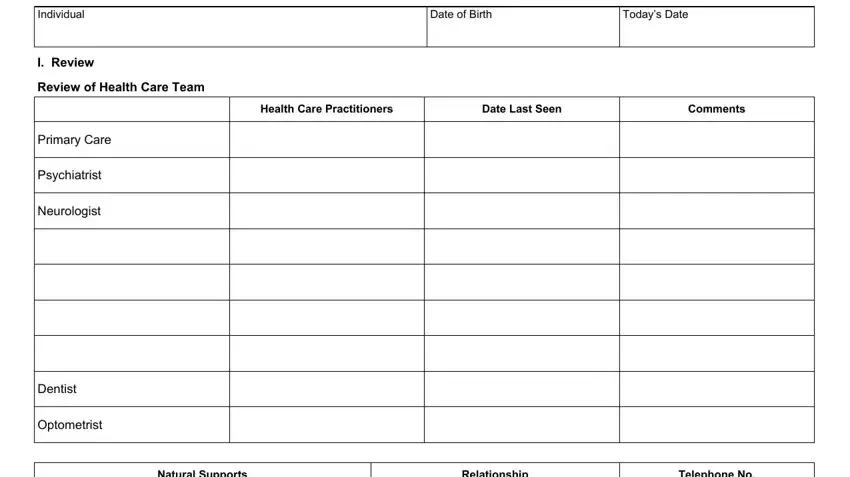
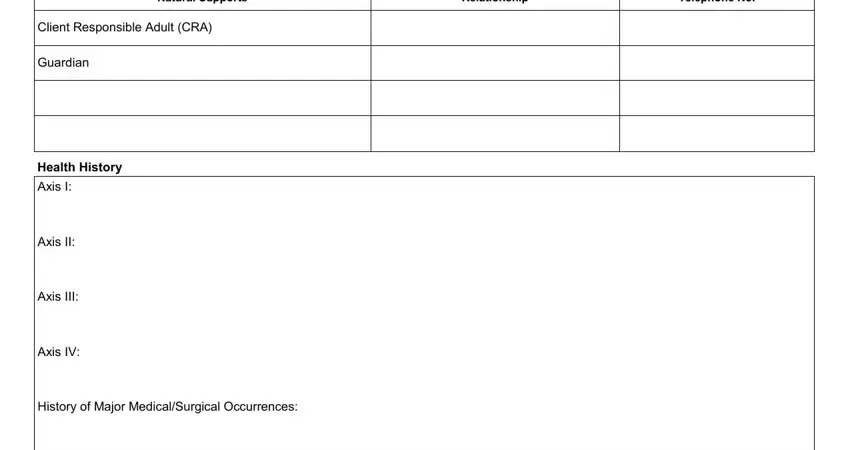
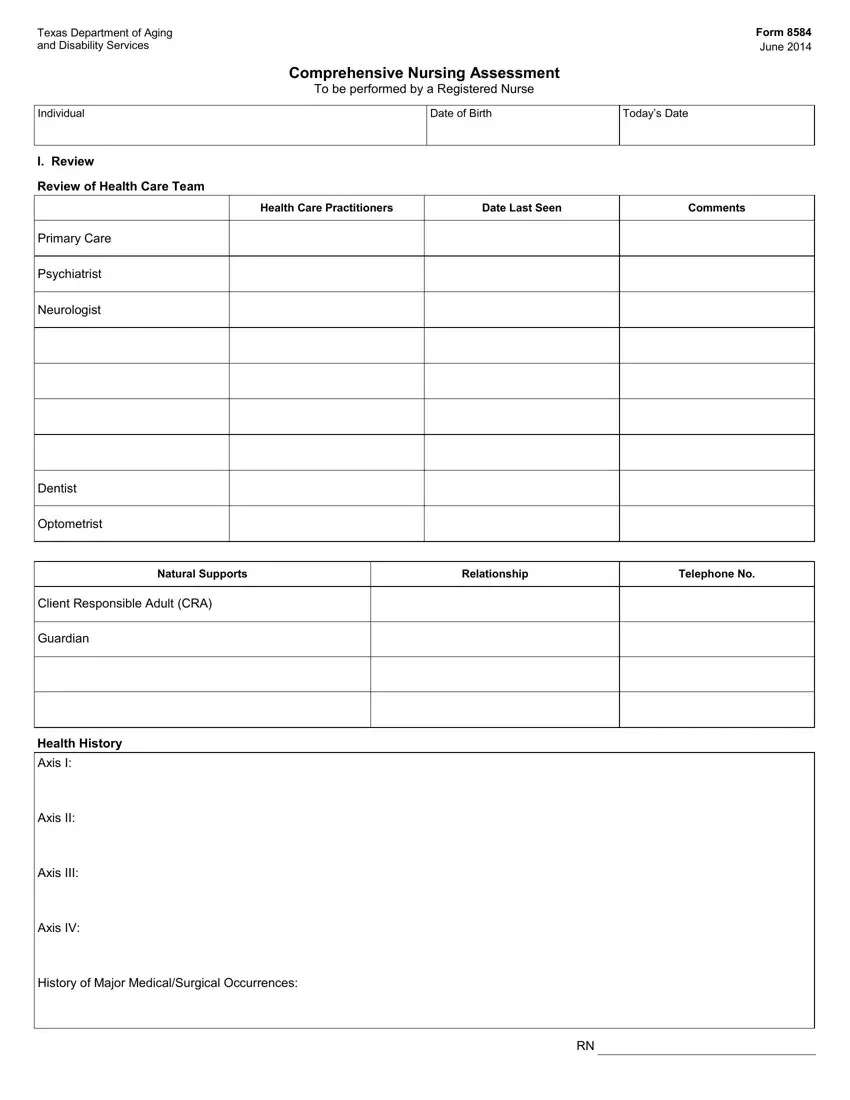
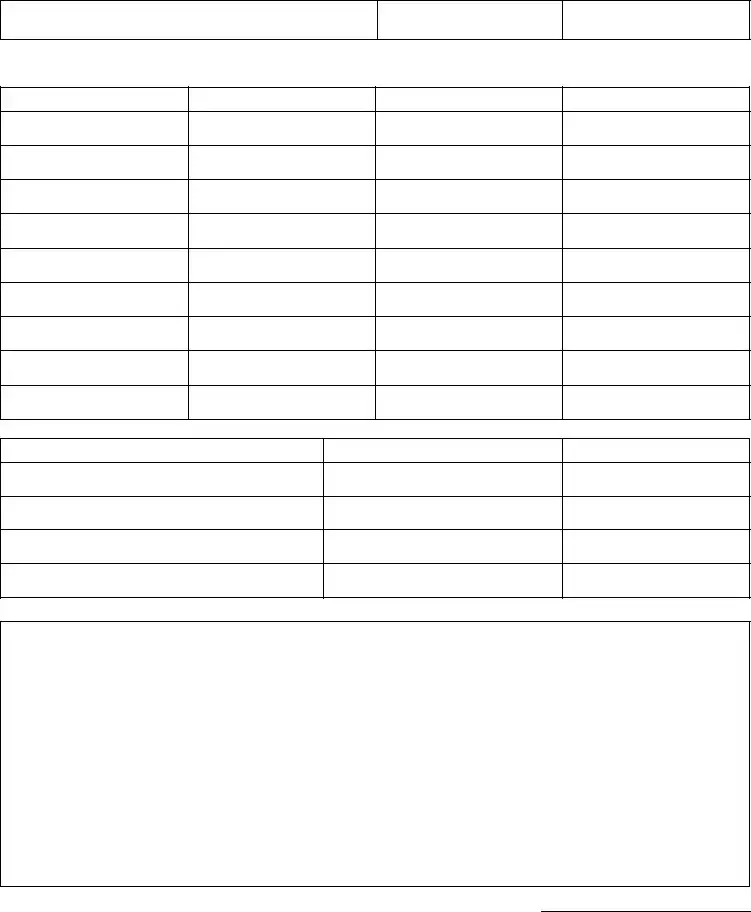
Write the essential data in the Natural Supports, Relationship, Telephone No, Client Responsible Adult CRA, Guardian, Health History, Axis I, Axis II, Axis III, Axis IV, and History of Major MedicalSurgical part.
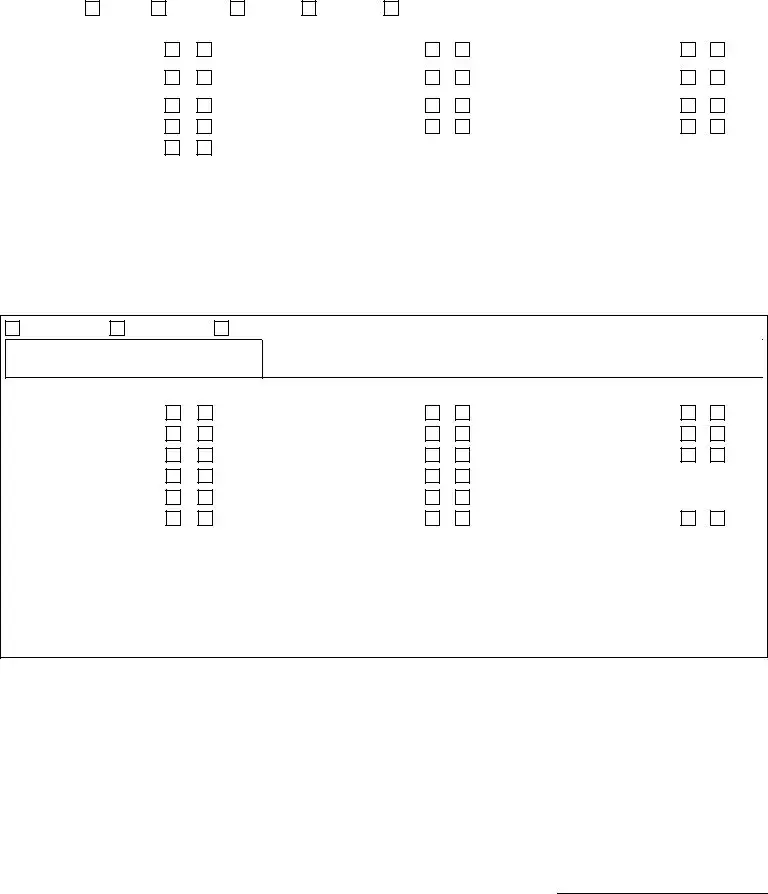
In the part, identify the valuable particulars.
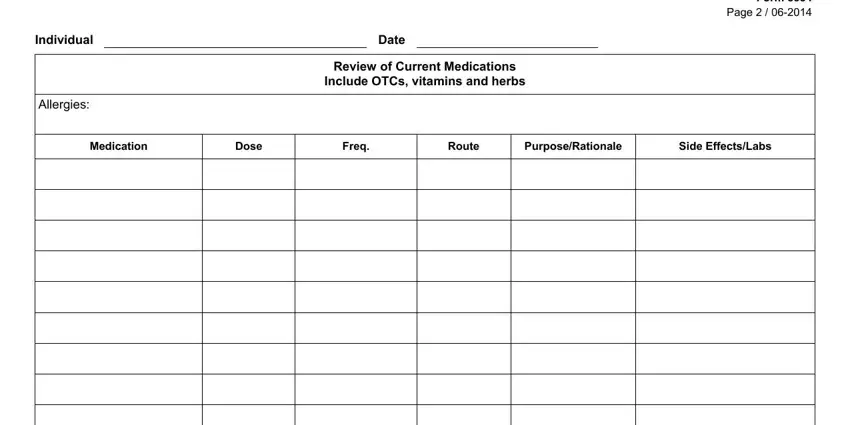
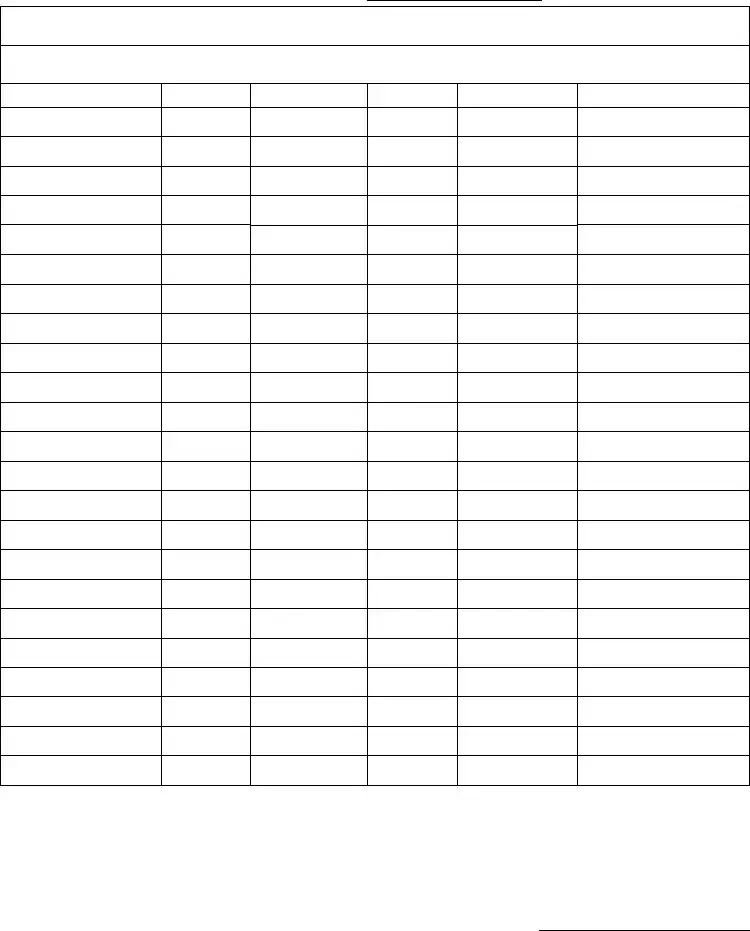
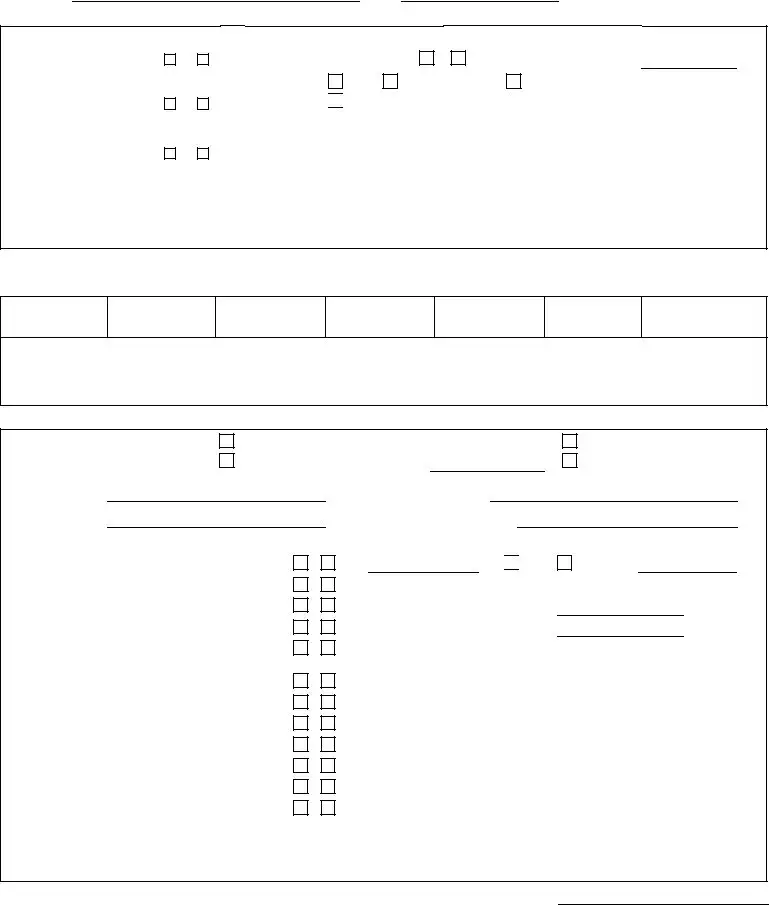
You'll have to spell out the rights and obligations of both parties in paragraph Individual, Date, Review of Current Medications, Allergies, Medication, Dose, Freq, Route, PurposeRationale, Side EffectsLabs, and Form Page.
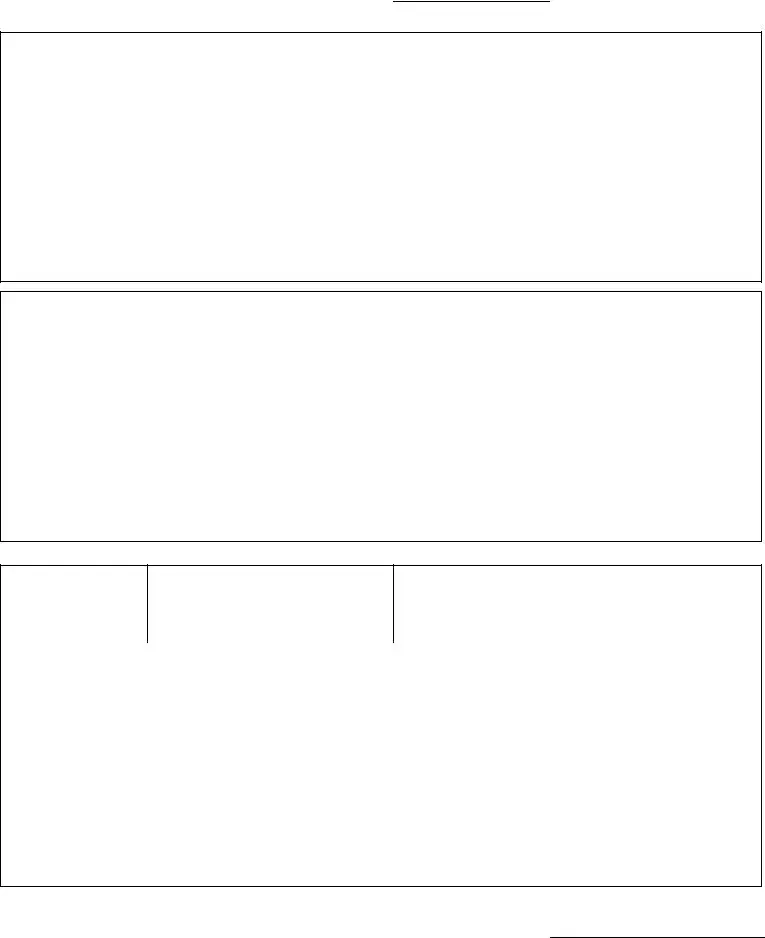
Finish by looking at the following areas and filling them out accordingly: .
Step 3: Choose the button "Done". The PDF form may be transferred. You can easily upload it to your device or email it.
Step 4: It may be better to keep duplicates of the document. There is no doubt that we won't disclose or check out your details.
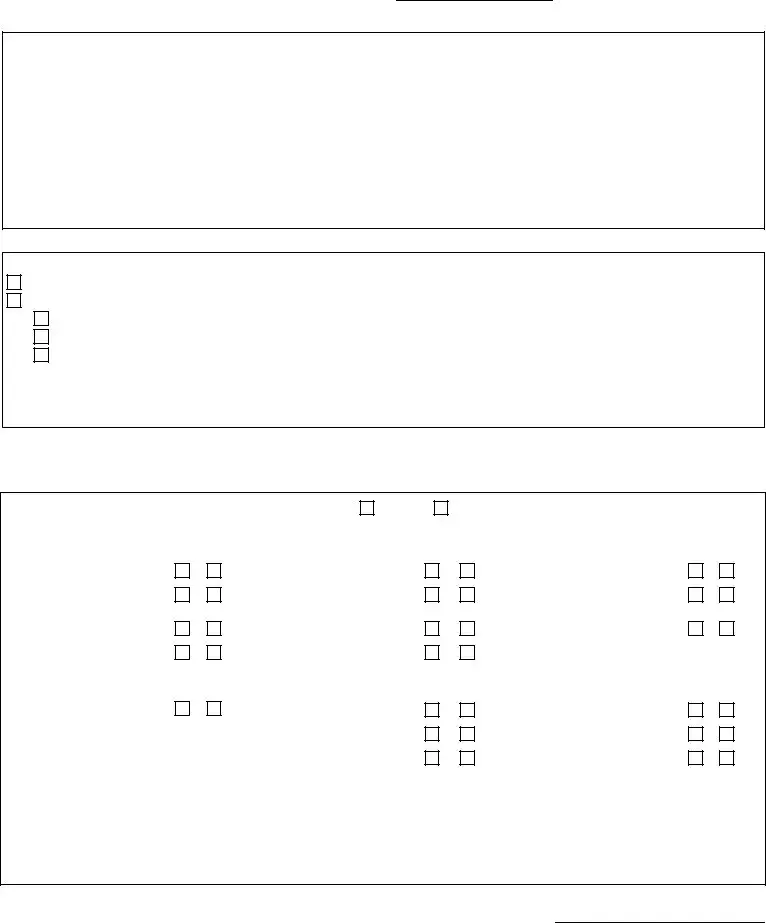
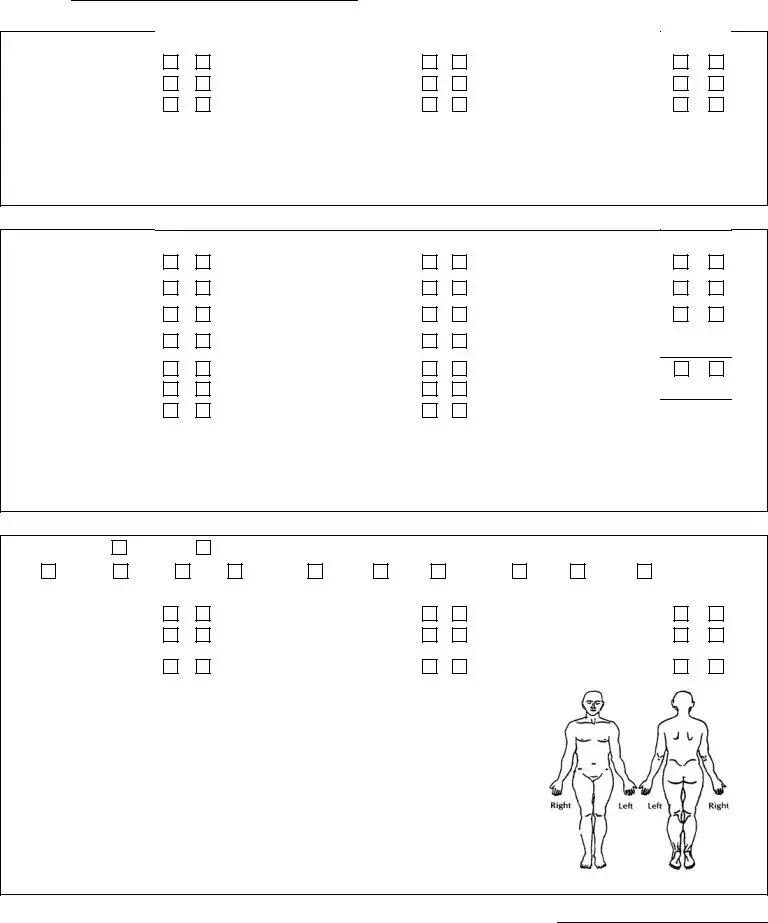

 Other injectable medication to manage diabetes Desired blood sugar range:
Other injectable medication to manage diabetes Desired blood sugar range:
 gain
gain