In the Commonwealth of Pennsylvania, ensuring that students of school age undergo a comprehensive physical examination is crucial for their well-being and educational success. The H511 336 form, devised by the Pennsylvania Department of Health, serves as the standardized document for private physicians to report these essential physical examinations. This form encompasses a wide variety of information starting with basic identification details of the student, including name, date of birth, and address. Importantly, it delves into the student's medical history, immunizations, and tests received by detailing the type and date of each vaccine administered, alongside booster shots. The form thoughtfully includes sections for medical and religious exemptions, particularly for cases where immunization might pose a risk to the child's health or conflict with familial beliefs. Furthermore, it requires details on significant medical conditions, covering a broad spectrum from allergies to neuromuscular disorders, aiming to highlight any special medical concerns that might necessitate restricted activity, medication, or could impact the student's education process. The form culminates with the physician's report of the physical examination, offering a concise overview of the pupil's health across various physiological parameters. Through this detailed reporting, the H511 336 form plays a pivotal role in safeguarding the health of Pennsylvania's school-aged children, ensuring they receive the proper care and considerations needed for a conducive learning environment.
| Question | Answer |
|---|---|
| Form Name | Form H511 336 |
| Form Length | 2 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 30 sec |
| Other names | DTaP, H511, pa school physical form h511 336, physical form for school pa |
H511.336 (Rev 5/02) |
COMMONWEALTH OF PENNSYLVANIA |
|
DEPARTMENT OF HEALTH |
PRIVATE PHYSICIAN’S REPORT OF
PHYSICAL EXAMINATION OF A PUPIL OF SCHOOL AGE
DATE _________________ 20_________
NAME OF SCHOOL __________________________________________________ GRADE ______ HOMEROOM ________
NAME OF CHILD
__________________________________________________________________________
Last |
First |
Middle |
DATE OF BIRTH
SEX
M F
ADDRESS
____________________________________________________________________________________________________
No. and Street City or Post Office Borough or Township County State Zip Code
MEDICAL HISTORY
IMMUNIZATIONS AND TESTS
|
Enter Month, Day, and Year each |
|
|
|
|
|
|
|
|||||||
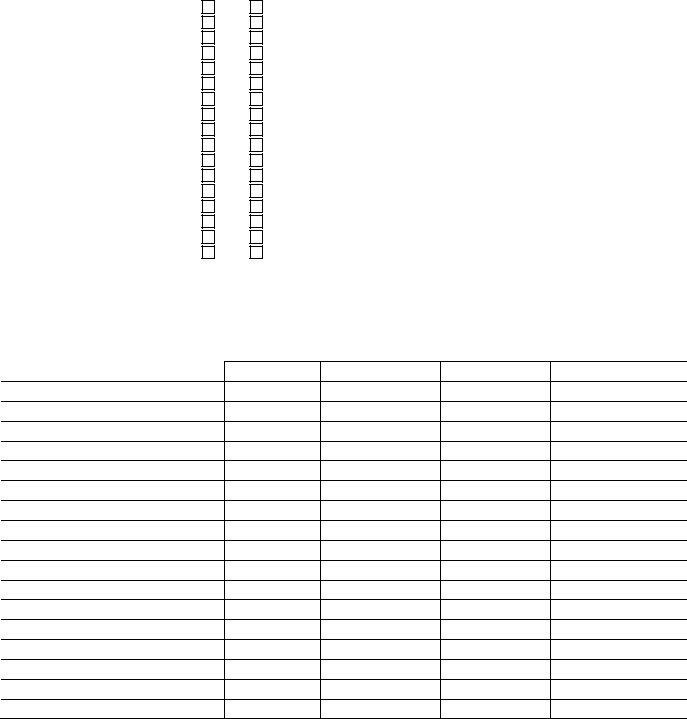
VACCINE |
immunization was given |
|
|
|
|
|
|
|
BOOSTERS & DATES |
|
|||||
|
|
|
|
|
DOSES |
|
|
|
|
|
|
|
|||
Diphtheria and Tetanus |
1 |
|
|
2 |
|
|
|
3 |
|
|
|
4 |
|
5 |
|
(Circle): DTaP, DTP, DT, TD |
|
/ |
/ |
|
/ |
/ |
|
|
/ |
/ |
|
/ |
/ |
/ |
/ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
|
2 |
|
|
|
3 |
|
|
|
4 |
|
5 |
|
Polio (Circle): OPV, IPV |
|
/ |
/ |
|
/ |
/ |
|
|
/ |
/ |
|
/ |
/ |
/ |
/ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
|
2 |
|
|
|
|
|
|
|
|
|
|
|
Measles, Mumps, Rubella |
|
/ |
/ |
|
/ |
/ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
|
|
|
|
2 |
|
|
|
|
|
3 |
|
|
Hepatitis B |
|
/ |
/ |
|
|
|
|
/ |
|
/ |
|
/ |
/ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
|
|
|
|
2 |
|
|
|
|
|
3 |
|
|
HIB |
|
/ |
/ |
|
|
|
|
/ |
|
/ |
|
/ |
/ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
1 |
|
|
|
|
|
2 |
|
|
|
|
|
Varicella Disease or Lab |
||
Varicella |
|
/ |
/ |
|
|
|
|
/ |
|
/ |
|
Evidence |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Date: __________________ |
||
Other: ___________________ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MEDICAL EXEMPTION The physical condition of the above named child is such that immunization would endanger life or health RELIGIOUS EXEMPTION (Includes a strong moral or ethical conviction similar to a religious belief and requires a written
statement from the parent/guardian)
If Applicable:
Tuberculin Tests |
|
|
|
|
|
Date Applied |
Arm |
Device |
Antigen |
Manufacturer |
Signature |
|
|
|
|
|
|
Date Read |
Results (mm) |
|
Signature |
|
|
|
|
|
|
|
|
Parent/Guardian notified of significant findings on _____________________________.
Result of Diagnostic Studies: _____________________________________________________________________.
Preventive |
|
___________ |
No |
Yes |
Date |
|
Significant Medical Conditions (√) |
|
If Yes, Explain |
Yes |
No |
Allergies |
_______________________________________________________________ |
Asthma |
_______________________________________________________________ |
Cardiac |
_______________________________________________________________ |
Chemical Dependency |
_______________________________________________________________ |
Drugs |
_______________________________________________________________ |
Alcohol |
_______________________________________________________________ |
Diabetes Mellitus |
_______________________________________________________________ |
Gastrointestinal Disorder |
_______________________________________________________________ |
Hearing Disorder |
_______________________________________________________________ |
Hypertension |
_______________________________________________________________ |
Neuromuscular Disorder |
_______________________________________________________________ |
Orthopedic Condition |
_______________________________________________________________ |
Respiratory Illness |
_______________________________________________________________ |
Seizure Disorder |
_______________________________________________________________ |
Skin Disorder |
_______________________________________________________________ |
Vision Disorder |
_______________________________________________________________ |
Other (Specify) |
_______________________________________________________________ |
Are there any special medical problems or chronic diseases which require restriction of activity, medication or
which might affect his/her education? If so, specify ____________________________________________________________
Report of Physical Examination (√) |
|
|
|
Normal |
Abnormal |
Not Examined |
Comments |
Height (inches)
Weight (pounds) BMI
Pulse ( )
Blood Pressure
Hair/Scalp
Skin
Eyes/Vision
Ears/Hearing
Nose and Throat
Teeth and Gingiva
Lymph Glands
Heart – Murmur, etc
Lung – Adventitious Finding
Abdomen
Genitourinary
Neuromuscular System
Extremities
Spine (Presence of Scoliosis)
_____________________________________________________
Date of Examination
_____________________________________________________ |
______________________________________________________ |
Signature of Examiner |
PRINT Name of Examiner |
______________________________________________________ |
______________________________________________________ |
Address |
Telephone Number |