Understanding the intricacies of health benefits post-employment or after major life changes can be quite daunting. The Pers Hbd 85 form, also known as the Public Employees' Retirement System (PERS) COBRA Continuation Coverage application, plays a pivotal role in this arena by offering a crucial bridge for individuals navigating the complexities of maintaining health coverage during transitional periods. Designed under the auspices of the Consolidated Omnibus Budget Reconciliation Act (COBRA), this document facilitates the extension of health benefits previously provided by public employers to employees, retirees, and their dependents in California. In essence, the form allows eligible individuals to continue their health insurance coverage when it would otherwise be lost due to specific qualifying events such as employment separation, divorce, or the death of the employee/retiree. Detailing essential information such as enrollee details, event dates, and coverage information, the form also outlines procedural guidelines for applying, including the necessary steps for electing COBRA coverage, the payment to carriers, and the implications of non-compliance. The form is not just a piece of paperwork but a crucial lifeline that ensures continuity of care for those in a state of transition, emphasizing the importance of timely and accurate submission to avoid any interruption in coverage.
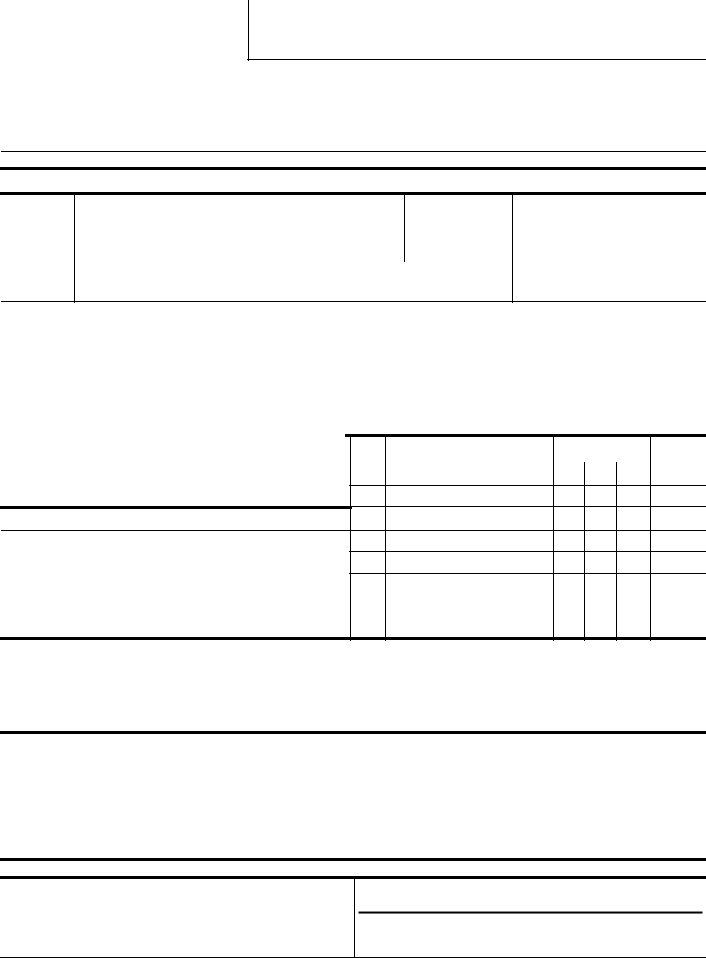
| Question | Answer |
|---|---|
| Form Name | Form Pers Hbd 85 |
| Form Length | 2 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 30 sec |
| Other names | TIMEBASE, PERS-HBD-85, pers hbd 85, 1977 |
C
GROUP CONTINUATION COVERAGE
CONSOLIDATED OMNIBUS BUDGET RECONCILIATION ACT “COBRA”
PERS USE ONLY – DOCUMENT REFERENCE NUMBER
PUBLIC EMPLOYEES’ RETIREMENT SYSTEM
Office of Employer and Member Health Services
P.O. Box 942714
Sacramento, CA
(888) CalPERS
TDD - (916)
INSTRUCTIONS FOR COMPLETING THIS FORM ARE ON THE REVERSE SIDE. PLEASE TYPE
PART A: ORIGINAL QUALIFYING EVENT AND DATES
1.Type of Action
1NEW
1Change
2. QUALIFYING EVENT
1EMPLOYMENT SEPARATION/TIMEBASE REDUCTION
1DIVORCE/LEGAL SEPARATION
1CHILD CEASES TO BE A DEPENDENT
1DEATH OF AN EMPLOYEE/RETIREE
1DEPENDENT CONTINUATION – ORIGINAL ENROLLEE ELIGIBLE
3. EVENT DATE |
4. COBRA ENROLLMENT PERIOD |
|
|
|
FROM |
|
01 |
|
FOR MEDICARE |
TO |
|
|
|
||
|
|
|
|
|
|
|
PART B: ENROLLEE INFORMATION
5. COBRA ENROLLEE (MAY BE DIFFERENT THAN SUBSCRIBER) |
6. SUBSCRIBER (EMPLOYEE/RETIREE) |
|
|
|||
SOCIAL SECURITY NUMBER |
— |
— |
SOCIAL SECURITY NUMBER |
|
— |
— |
|
|
|
||||
NAME |
|
|
NAME |
|
|
|
|
|
|
|
|
|
|
ADDRESS |
|
|
|
|
|
|
|
|
|
|
|
|
|
CITY, STATE, ZIP
Day Phone |
|
Married 1Yes |
1 No |
|
( |
) |
|
|
|
|
|
|
|
|
BIRTHDATE |
|
SEX 1 MALE |
1 FEMALE |
|
|
|
|
|
|
PART C: CARRIER INFORMATION
7. NAME AND ADDRESS OF HEALTH PLAN
PART D: DEPENDENT INFORMATION
A |
|
|
|
DATE OF BIRTH |
FAMILY |
|
C C |
LIST ALL PERSONS (including self) |
|||||
RELATION |
||||||
T O |
TO BE ENROLLED IN: |
|
|
|||
|
|
|
||||
I D |
|
|
|
|
SHIP |
|
O E |
(FIRST) |
(MI) |
(LAST) MO. DAY YR |
|
||
N |
|
|||||
|
|
|
|
|
SELF |
|
PLAN CODE:______________ |
PREMIUM: $____________ |
|
|
PHONE: |
|
PART E: ENROLLMENT CHANGES
9. NAME OF PRIOR HEALTH PLAN |
11. PERMITTING EVENT |
12. PERMITTING EVENT |
13. EFFECTIVE DATE OF |
||||||
|
CODE |
DATE |
CHANGE |
||||||
|
|
|
|
|
|
|
|
01 |
|
10. PRIOR PLAN CODE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PART F: ELECTION CERTIFICATION
14.I AGREE TO PAY THE PREMIUM FOR THE COVERAGE DIRECTLY TO THE CARRIER LISTED ABOVE. I UNDERSTAND THAT I AM REQUIRED TO SEND THE INITIAL PAYMENT PRIOR TO EFFECTIVE DATE OF ENROLLMENT AND AGREE TO MAKE FUTURE PAYMENTS IN A TIMELY MANNER AS REQUIRED BY THE CARRIER. I UNDERSTAND THAT FAILURE TO PAY THE PREMIUM WILL RESULT IN AUTOMATIC TERMINATION OF COVERAGE. I CERTIFY THAT THE INFORMATION PROVIDED BY ME IS TRUE AND CORRECT TO THE BEST OF MY KNOWLEDGE AND ABILITY.
______________________________________________________________________ |
__________________________ |
SIGNATURE OF COBRA ENROLLEE (SEE REVERSE FOR PRIVACY INFORMATION) |
DATE SIGNED |
PART G: AGENCY INFORMATION
15.
AGENCY NAME ________________________________________
AGENCY CODE _________________ UNIT CODE __________
16. HEALTH BENEFITS OFFICER’S SIGNATURE
PHONE ( ) __________________ DATE RECEIVED __________
PRIVACY INFORMATION
Submission of the requested information is mandatory. The information requested is collected pursuant to the Government Code Sections (20000. et seq.) and will be used for administration of the Board’s duties under the Retirement Law, the Social Security Act, and the Public Employees’ Medical and Hospital Care Act, as the case may be. Portions of this information may be transferred to another governmental agency (such as your employer) but only in strict accordance with current statutes regarding confidentiality. Failure to supply the information may result in the System being unable to perform its functions regarding your status.
You have the right to review your membership files maintained by the System. For questions concerning your rights under the Information Practices Act of 1977, please contact the Information Practices Act Coordinator, CalPERS, P.O. Box 942702, Sacramento, CA
INSTRUCTIONS FOR THE COMPLETION OF FORM
Part A: 1. Type of Action. Check “new” if this is a new enrollment.
Check “change” if family member is added, deleted, or for plan changes.
2.Check applicable original qualifying event.
3.Provide original event date (separation, date of divorce, etc.).
4.Original COBRA enrollment period. Examples:
|
Separation from employment |
|
|
Child attains age 23 on |
FROM |
Part B. 5. |
Please provide all requested information. |
|
6. |
If the COBRA enrollee is a former dependent, the employee/retiree must be identified in Box 6. |
|
Part C. 7. Please identify the carrier. The COBRA enrollee must continue the same coverage which he or she had as an employee or as a dependent. Carrier changes are only allowed during the open enrollment period of if the enrollee moves into or out of a carrier’s geographic service area. The carrier’s name, address, phone number, plan code, and premium can be found in the annual “Health Plan Decision Guide” which is available in all employing agencies. The monthly premium may not exceed 102% of the group rate.
Part D. 8. List all family members to be enrolled, including self.
Action Code: Use “A” to indicate which person is being added (or newly enrolled).
Use “D” to indicate individual is being deleted from an existing COBRA enrollment An Action Code is not required when changing carriers.
IMPORTANT: The addition or deletion of family members is regulated by time limits which are identical to those for active enrollees (subscribers).
Part E.
Part F. 14. Signature of COBRA enrollee and date signed.
Part G.
IMPORTANT: It is the responsibility of the COBRA enrollee to report enrollment changes in a timely manner. Enrollment change requests must be submitted in accordance with existing regulations, laws, and the time limits applicable to the Public Employees’ Medical and Hospital Care Act. All change requests are directed through the agency listed in Part G.