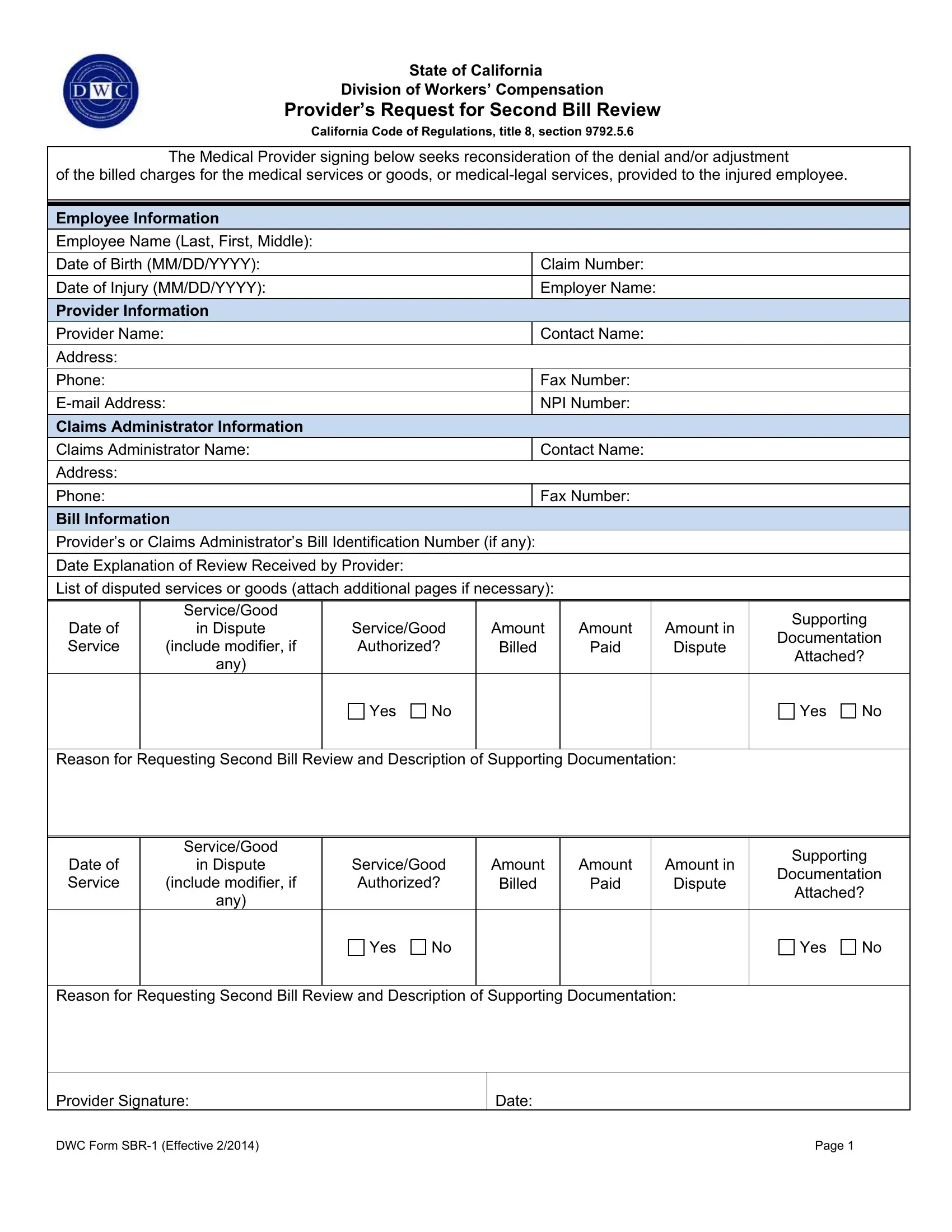
State of California
Division of Workers’ Compensation
Provider’s Request for Second Bill Review
California Code of Regulations, title 8, section 9792.5.6
The Medical Provider signing below seeks reconsideration of the denial and/or adjustment
of the billed charges for the medical services or goods, or medical-legal services, provided to the injured employee.
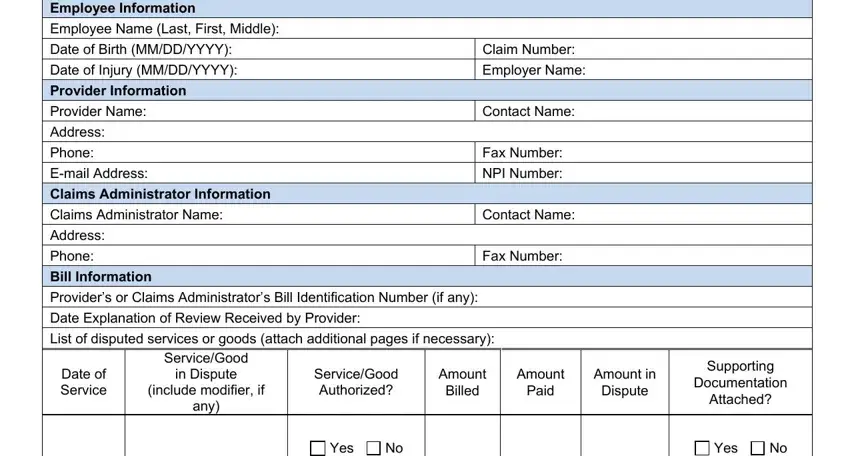
Employee Information
Employee Name (Last, First, Middle):
Date of Birth (MM/DD/YYYY): |
Claim Number: |
|
|
Date of Injury (MM/DD/YYYY): |
Employer Name: |
|
|
Provider Information |
|
Claims Administrator Information
Claims Administrator Name: |
Contact Name: |
Address:
Bill Information
Provider’s or Claims Administrator’s Bill Identification Number (if any):
Date Explanation of Review Received by Provider:
List of disputed services or goods (attach additional pages if necessary):
Service/Good
in Dispute
(include modifier, if
any)
Supporting
Documentation
Attached?
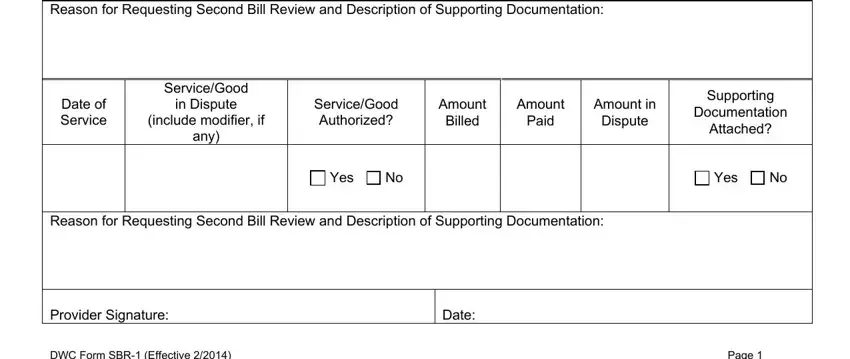
Reason for Requesting Second Bill Review and Description of Supporting Documentation:
Service/Good
in Dispute
(include modifier, if
any)
Supporting
Documentation
Attached?
Reason for Requesting Second Bill Review and Description of Supporting Documentation:
DWC Form SBR-1 (Effective 2/2014) |
Page 1 |
Instructions for Provider’s Request for Second Bill Review
Overview: The Provider’s Request for Second Bill Review (DWC Form SBR-1) is used to initiate the second bill review process required by Labor Code sections 4603.2(e), for medical treatment services and goods, and by Labor Code section 4622, for medical-legal services, to dispute the amount of payment. The Division of Workers’ Compensation’s (DWC) regulation outlining the process can be found at California Code of Regulations, title 8 (8 C.C.R.), section 9792.5.5. Under this process, a medical provider who disputes the amount paid by a claims administrator on either a bill for medical treatment services or goods, or a bill for medical-legal expenses, must request a second review of the bill from the claims administrator. The second bill review process must be completed before a provider can seek independent bill review of a billing dispute.
How to Apply: To apply for a second review of a non-electronic medical treatment bill, you can use either this form or a modified standardized bill. See 8 C.C.R. section 9792.5.5(c)(1) and the California Division of Workers’ Compensation Medical Billing and Payment Guide, version 1.2, for instructions as to how to submit a request for second review using a non-electronic standardized bill. For an electronic medical treatment bill, refer to 8 C.C.R. section 9792.5.5(c)(2) and (3) and the California Division of Workers’ Compensation Electronic Medical Billing and Payment Companion Guide, version 1.2, for instructions as to how to submit a request for second review under that format. Both guides can be found at the DWC website at http://www.dir.ca.gov/dwc/EBilling/EBilling.html. For medical-legal bills, the second review must be on this form.
When to Apply: A request for second bill review must be made within 90 days of service of the explanation of review that explained why the payment you sought in the initial bill was reduced or denied. If an issue that would preclude your right to receive compensation for the submitted bill is under consideration by the Workers’ Compensation Appeal Board (WCAB), you have 90 days from the date of the service of the WCAB order that resolves the issue to request the second bill review. If the only dispute is the amount of payment and you do not timely request a second bill review, the bill will be considered satisfied and neither the claims administrator nor the employee shall be liable to you for any further payment.
Routing Information: The Request for Second Bill Review form can either be mailed or faxed to the claims administrator. The requesting provider must complete all fields in the Employee Information, Provider Information, and Claims Administrator Information sections.
Bill Information: Complete all fields in this section for each disputed service or good, or medical-legal service. Attach additional pages if necessary.
Provide your or the claims administrator’s bill identification number, if any.
State the date when the explanation of review that either denied or reduced the amount billed was received.
State the date of service.
State the service or good for which payment is in dispute. Include the code and modifier, if any.
Indicate whether the billed service was authorized.
State the amount billed, the amount paid, and the amount in dispute.
State whether supporting documentation is attached. (For example, documents provided in response to a request by the claims administrator in the explanation of review.)
State the reason for requesting the second bill review and describe the supporting documentation.
Provider Signature: Signature/Date line is located at the bottom of the form.
A SECOND BILL REVIEW REQUEST MUST BE COMPLETED FOR A PROVIDER TO SEEK INDEPENDENT BILL REVIEW OF A BILLING DISPUTE.
DWC Form SBR-1 (Effective 2/2014) |
Page 2 |