Number of tasks can be quicker than managing files taking advantage of the PDF editor. There isn't much for you to do to enhance the nurse practitioner patient physical and yealth assessment form form - just simply follow these steps in the next order:
Step 1: Hit the orange button "Get Form Here" on this web page.
Step 2: At this point, you're on the document editing page. You may add information, edit current information, highlight certain words or phrases, insert crosses or checks, insert images, sign the document, erase unnecessary fields, etc.
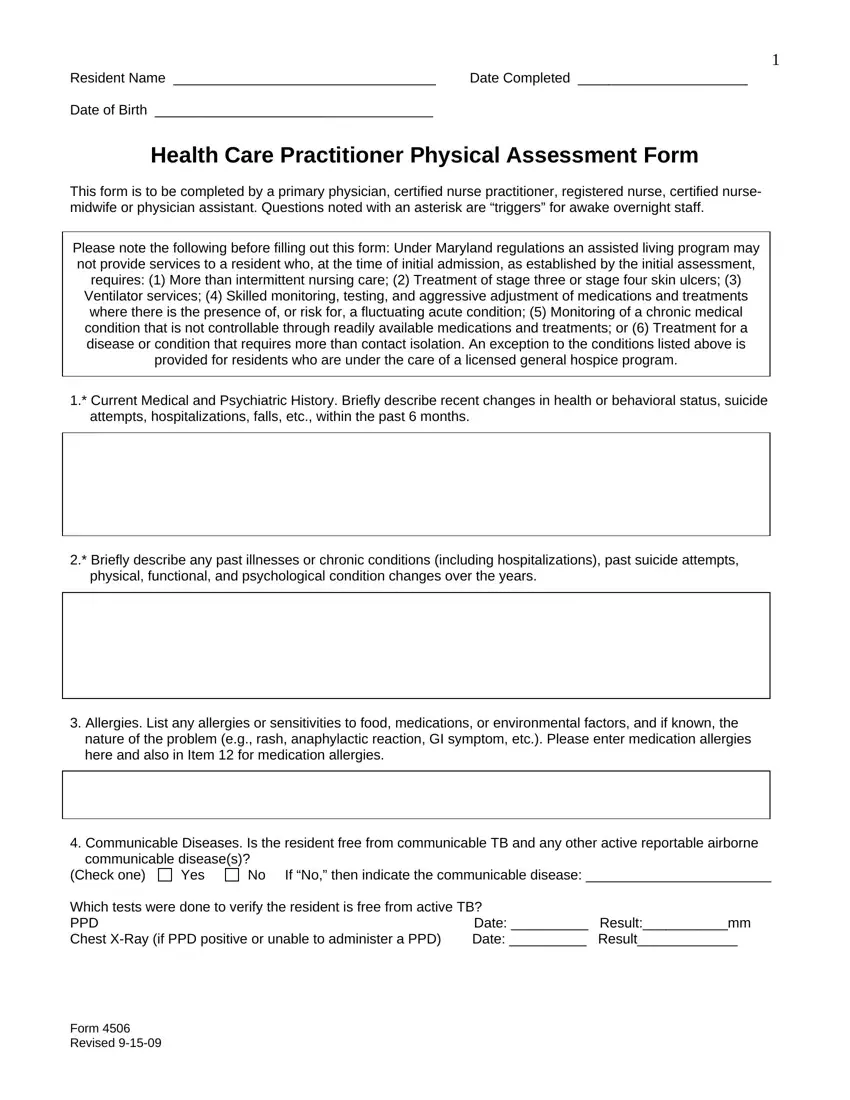
Create the nurse practitioner patient physical and yealth assessment form PDF by typing in the data meant for each part.
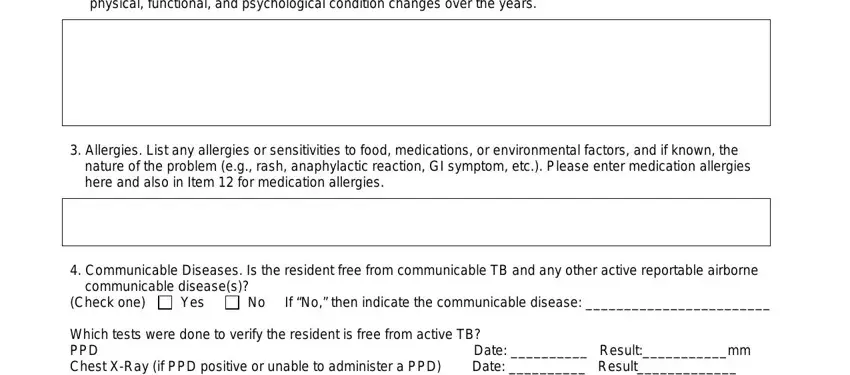
Type in the necessary information in the physical functional and, Allergies List any allergies or, nature of the problem eg rash, Communicable Diseases Is the, communicable diseases, Check one, Yes, No If No then indicate the, Which tests were done to verify, and Date Resultmm segment.
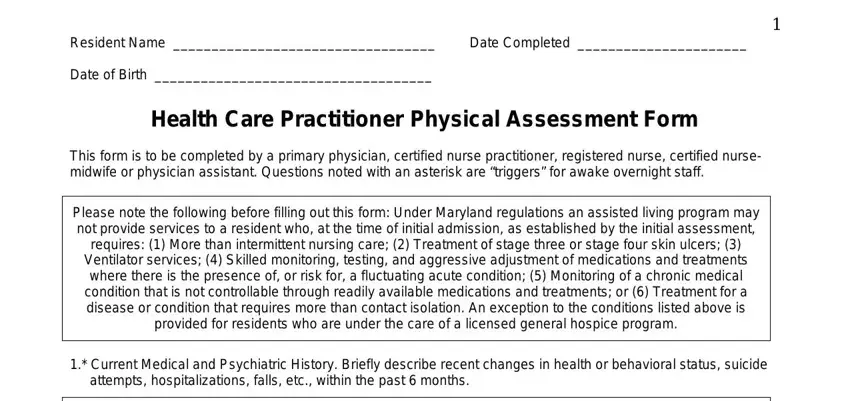
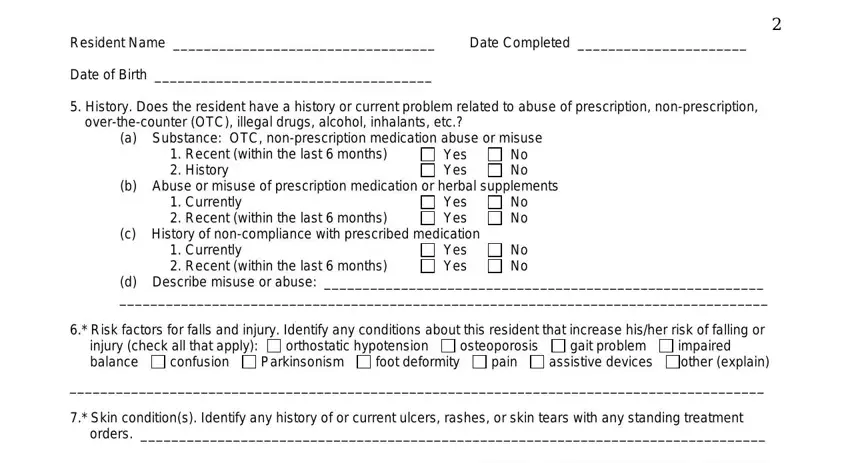
In the Resident Name, Date Completed, Date of Birth, History Does the resident have a, overthecounter OTC illegal drugs, a Substance OTC nonprescription, Recent within the last months, Yes Yes, No No, b Abuse or misuse of prescription, Currently Recent within the last, Yes Yes c History of noncompliance, Currently Recent within the last, No No, and No No segment, emphasize the essential details.
The Sensory impairments affecting, Left ear Right ear, Adequate Adequate, Poor Poor, Deaf Uses corrective aid Deaf Uses, b Vision c Temperature Sensitivity, Adequate, Poor, Uses corrective lenses, Blind check all that apply, Normal, Decreased sensation to, Heat, Cold, and Weight lbs area is the place where both sides can indicate their rights and responsibilities.
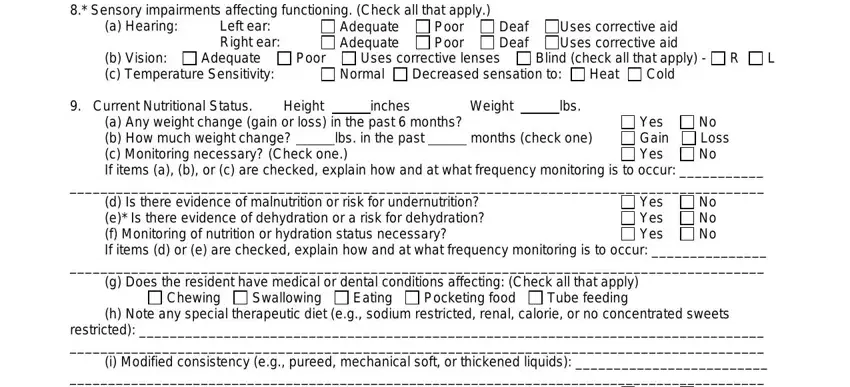
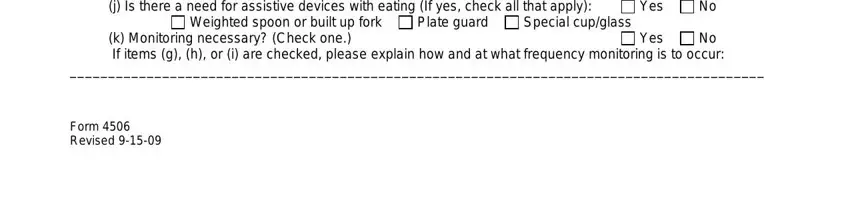
Prepare the document by looking at all these sections: h Note any special therapeutic, Yes, Weighted spoon or built up fork, Plate guard, Special cupglass, k Monitoring necessary Check one, Yes, and Form Revised.
Step 3: Press "Done". Now you may transfer the PDF document.
Step 4: To prevent potential future concerns, take the time to possess a minimum of two or more copies of each and every form.

 orthostatic hypotension
orthostatic hypotension 
 osteoporosis
osteoporosis 
 gait problem
gait problem 
 impaired
impaired confusion
confusion  Parkinsonism
Parkinsonism  foot deformity
foot deformity  pain
pain  assistive devices
assistive devices  other (explain)
other (explain) Chewing
Chewing  Swallowing
Swallowing  Eating
Eating  Pocketing food
Pocketing food  Tube feeding
Tube feeding



 Other
Other