The Molina Healthcare Resolution Request form represents a critical tool for healthcare providers seeking to address and resolve disputes or disagreements with Molina Healthcare, specifically regarding claims processing, payment issues, or policy interpretations. By submitting this form, providers essentially agree not to bill the patient for the disputed service, thereby safeguarding patients from financial responsibility amid provider-insurer disputes. Required fields marked with an asterisk must be meticulously filled out, including provider details, claim information, and a clear description of the dispute alongside the expected outcome. This process underscores the importance of submitting comprehensive supporting information to bolster the dispute's description. The guideline stipulates the form’s submission exclusively via mail to Molina Healthcare of California, highlighting the formality and specificity of the dispute resolution process. It is also made clear that this form is not intended for routine follow-up inquiries, for which a separate Provider Tracking Form is recommended. The inclusion of various provider types and the distinction between single and multiple claims underscore the form's versatility in addressing diverse provider needs. By facilitating a structured process for dispute resolution, the form plays a pivotal role in the broader framework of provider-insurer relations, aiming to streamline the resolution of conflicts through standardized procedures.
| Question | Answer |
|---|---|
| Form Name | Molina Healthcare Resolution Request Form |
| Form Length | 1 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 15 sec |
| Other names | molina dispute form florida pdf, molina appeal form, molina dispute resolution request form, molina provider dispute resolution request |
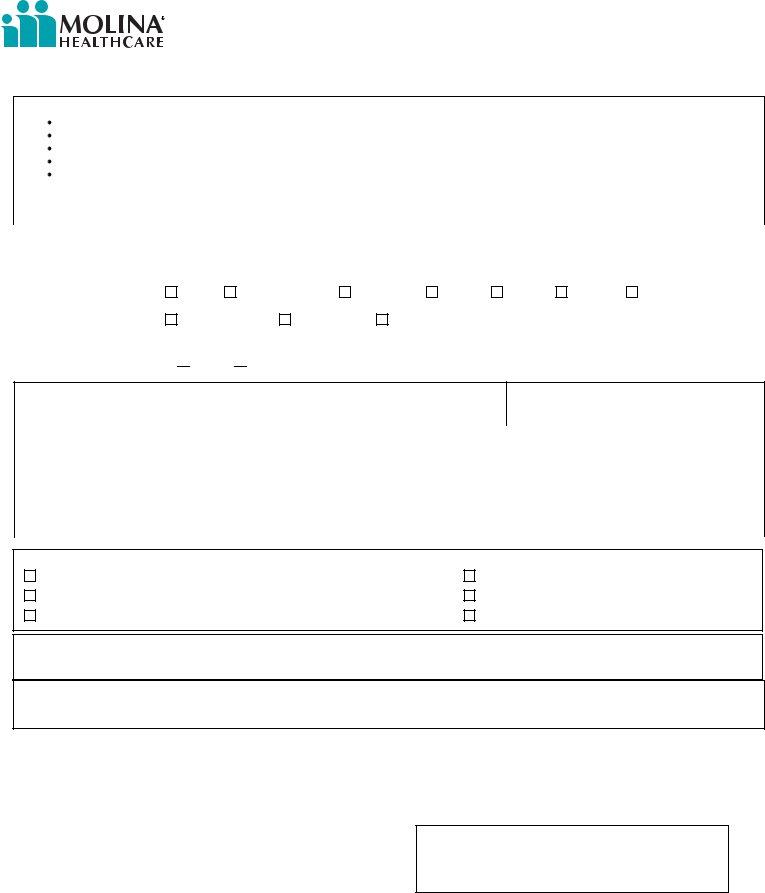
PROVIDER DISPUTE RESOLUTION REQUEST
NOTE: SUBMISSION OF THIS FORM CONSTITUTES AGREEMENT NOT TO BILL THE PATIENT
INSTRUCTIONS
Please complete the below form. Fields with an asterisk ( * ) are required.
Be specific when completing the DESCRIPTION OF DISPUTE and EXPECTED OUTCOME.
Provide additional information to support the description of the dispute..
For routine
Mail the completed form to: |
Molina Healthcare of California |
|
|
P.O. Box 22722 |
|
|
Long Beach, CA 90801 |
|
|
ATTN: Provider Dispute Resolution |
|
|
|
|
*PROVIDER NAME: |
|
*PROVIDER TAX ID # / Medicare ID #: |
PROVIDER ADDRESS: |
|
|
|
|
|
PROVIDER TYPE
* CLAIM INFORMATION
MD |
Mental Health |
Hospital |
ASC |
SNF |
DME |
Rehab |
|
Home Health |
Ambulance |
Other |
|
|
|
|
|
(please specify type of “other”)
Single Multiple “LIKE” Claims (complete attached spreadsheet) NUMBER OF CLAIMS:___
* Patient Name:
Date of Birth:
* Health Plan ID Number: |
Patient Account Number: |
Original Claim ID Number: (If multiple claims, |
||
|
|
|
use attached spreadsheet) |
|
|
|
|
|
|
Service “From/To” Date: ( * Required for Claim, Billing, and |
Original Claim Amount Billed: |
Original Claim Amount Paid: |
||
Reimbursement Of Overpayment Disputes) |
|
|
|
|
|
|
|
|
|
DISPUTE TYPE
Claim
Appeal of Medical Necessity / Utilization Management Decision
Request For Reimbursement Of Overpayment
Seeking Resolution Of A Billing Determination Contract Dispute
Other:
*DESCRIPTION OF DISPUTE:
EXPECTED OUTCOME:
|
|
|
( |
) |
|
Contact Name (please print) |
|
Title |
|
Phone Number |
|
|
|
|
( |
) |
|
Signature |
|
Date |
|
Fax Number |
|
For Health Plan Use Only
TRACKING NUMBER
PROVIDER ID#
[] CHECK HERE IF ADDITIONAL INFORMATION IS ATTACHED (Please do not staple additional information)
Revise:08/2010