In an era where the expectations on healthcare professionals are continually rising, the 14th Edition of Tidy's Physiotherapy serves as an essential guide for physiotherapists striving to excel in their profession. This comprehensive form encapsulates the multifaceted nature of physiotherapy, emphasizing the responsibilities that come with the title, both ethically and practically. With insights into becoming a professional within the UK context, it covers the essence of professionalism, clinical governance, evidence-based practice, and the evolution towards autonomy within the field. The form highlights the importance of continuous professional development, national standards, and service evaluation in delivering high-quality, patient-centered care. It stresses the significance of meeting societal and governmental expectations for healthcare delivery, acknowledging the profession's privileged status while also exploring future challenges. The form acknowledges that physiotherapists enter the field with a commitment to improving lives, and it meticulously outlines how they can make this a reality amidst changing healthcare landscapes. Furthermore, it underscores the unique skills and knowledge physiotherapists bring to their practice, advocating for a patient-partnership model in clinical decision-making. As the profession navigates its evolving role within the UK's health services, Tidy's Physiotherapy 14th Edition form serves as a vital resource for professionals committed to upholding the highest standards of care.
| Question | Answer |
|---|---|
| Form Name | Tidys Physiotherapy 14Th Edition Form |
| Form Length | 19 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 4 min 45 sec |
| Other names | tidy's physiotherapy 12th edition book pdf, tidy's physiotherapy pdf download, tidy's physiotherapy pdf, tidys physiotherapy 12th edition pdf download |
Porter: Tidy's Physiotherapy, 14th Edition
1
Chapter 1
The responsibilities of being a physiotherapist
Ralph Hammond and Julie Dawn Wheeler
CHAPTER CONTENTS |
|
|
|
INTRODUCTION |
FINAL |
||||||||||
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
This chapter aims to provide the reader with an insight |
||||||||||||
|
|
|
|
|
|
|
|||||||||
Introduction |
1 |
|
|
|
|
into what it means to be a professional (in the context |
|||||||||
Characteristics of being a professional |
2 |
|
of this |
chapter, |
a physiotherapist), |
focusing on the |
|||||||||
|
responsibilities, both ethical and practical, that are |
||||||||||||||
|
|
|
|
|
|
|
|||||||||
Responsibilities of being a professional |
5 |
|
inherent in claiming to be a professional working in |
||||||||||||
Becoming an autonomous profession |
6 |
|
the UK. |
- |
NOT |
|
|
|
|||||||
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
The current status and privilege of physiotherapists |
|||||||
Clinical governance |
7 |
|
|
|
as autonomous professionals will be placed in the con- |
||||||||||
|
|
|
|
|
OF |
|
ELSEVIER |
|
|
|
|||||
|
|
text of the history of the profession, and the impact of |
|||||||||||||
|
|
autonomy on clinical practice will be explored. The |
|||||||||||||
|
|
|
|
|
|
||||||||||
Clinical effectiveness |
10 |
|
|
chapter will reflect on the implications for physiothera- |
|||||||||||
|
|
pists of the increasing expectations of both the general |
|||||||||||||
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
public and the government for health professionals to |
|||||||||
Applying national standards and guidelines |
|
||||||||||||||
locally 10 |
|
|
|
|
|
deliver |
|||||||||
Evaluating services |
12 |
|
|
|
how |
physiotherapists can |
meet |
these expectations |
|||||||
|
|
|
through clinical governance will be provided. Finally, |
||||||||||||
|
|
|
|
|
|
|
|||||||||
Continuing professional development |
13 |
|
the reader will be offered a look at the possible future |
||||||||||||
|
|
|
|
|
CONTENTof the profession in light of the changing shape of |
||||||||||
Having the right workforce (and using it |
|
health services in the UK. |
|
|
|
||||||||||
appropriately) 14 |
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
Physiotherapists come into the profession because |
||||||||||
|
|
|
|
|
|
|
|
||||||||
Monitoring clinical governance |
15 |
|
|
they have an underlying sense of |
and commitment |
||||||||||
The future |
|
15 |
|
|
|
|
to |
helping others and improving |
their quality of |
||||||
|
|
|
|
|
life. Indeed, Koehn (1994) argues that professionals |
||||||||||
|
|
|
|
|
|
|
|||||||||
Sources of critical appraisal tools |
17 |
|
|
can be |
thought |
of as being |
defined |
by a distinctive |
|||||||
PROPERTY |
|
|
commitment to |
benefit the client. |
Physiotherapists |
||||||||||
Acknowledgements |
18 |
|
|
|
want to be able to use their acquisition of knowledge, |
||||||||||
|
|
|
|
|
|
|
|||||||||
References |
|
18 |
|
|
|
|
skills |
and attributes from qualifying |
programmes to |
||||||
|
SAMPLE |
|
|
benefit people, in whatever specialty or with whichever |
|||||||||||
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
patient group they wish to work once qualified |
||||||||
|
|
|
|
|
|
|
for example, elite athletes, older people, people with |
||||||||
|
|
|
|
|
|
|
developmental or acquired conditions, people with |
||||||||
|
|
|
|
|
|
|
mental health problems. This chapter will help readers |
||||||||
|
|
|
|
|
|
|
understand how they can |
make |
benefiting patients |
||||||
|
|
|
|
|
|
|
a reality in the context of the expectations of society |
||||||||
|
|
|
|
|
|
|
for the provision of |
||||||||
|
|
|
|
|
|
|
care. |
|
|
|
|
|
|
|
|
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
2THE RESPONSIBILITIES OF BEING A PHYSIOTHERAPIST
1 |
|
While earlier editions of Tidy’s Physiotherapy may |
|
The professional body for physiotherapists, the |
||||||||||
have been popular for their prescriptive descriptions |
Chartered Society of Physiotherapy (CSP), provides a |
|||||||||||||
|
of what physiotherapists should do in particular situa- |
framework for the curriculum of physiotherapy educa- |
||||||||||||
|
tions or for specific conditions, this edition demands |
tion and approves those physiotherapy programmes |
||||||||||||
|
more from the reader. No two patients are quite the |
that meet the requirements of the framework on behalf |
||||||||||||
|
same; each requires the skills of the physiotherapist to |
of the profession. |
|
|
|
|||||||||
|
carry out a full and accurate assessment, taking account |
|
The CSP also publishes rules of professional conduct |
|||||||||||
|
of the individuality of the patient, and then to use clini- |
and standards of physiotherapy practice derived from |
||||||||||||
|
cal reasoning to |
within the profession, which are in harmony with those |
||||||||||||
|
options for treatment, on which the patient will make |
of the HPC. Anyone on the HPC physiotherapist regis- |
||||||||||||
|
a decision. A professional is required to have the matu- |
ter may call themselves a physiotherapist; only those |
||||||||||||
|
rity to take full responsibility for the privilege of auton- |
who are members of the CSP may call themselves a |
||||||||||||
|
omy. This will be by maintaining a competence to |
chartered physiotherapist. |
|
|
||||||||||
|
practise through |
|
The breadth of activity and resources that the CSP |
|||||||||||
|
undertakes and provides seek to establish a level of excel- |
|||||||||||||
|
present practice; by keeping up to date with the most |
lence for the profession. Its education and professional |
||||||||||||
|
effective interventions; and by maintaining the trust of |
activity is centred on leading and supporting members’ |
||||||||||||
|
patients by doing good. Readers should realise that |
delivery of |
||||||||||||
|
while this approach is more challenging, it will also |
|
|
|
|
|
|
|
FINAL |
|||||
|
activity emanates from its status as the professional body |
|||||||||||||
|
be more rewarding. |
|
|
|
|
for physiotherapy in the UK and therefore as the primary |
||||||||
|
|
|
|
|
|
|
holder and shaper of physiotherapy practice. The CSP |
|||||||
|
|
CHARACTERISTICS OF BEING |
|
|
|
works on behalf of the profession to protect the chartered |
||||||||
|
|
|
|
|
status of physiotherapists’ standing, which is one denot- |
|||||||||
|
|
A PROFESSIONAL |
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
NOT |
|
|||
|
|
|
|
|
|
|
ing excellence. It is worth noting that the relationship with |
|||||||
|
|
Becoming a professional requires an acceptance, often |
|
|
|
- |
|
|
|
|
||||
|
|
the HPC is one of registrant; with the CSP it is one of |
||||||||||||
|
|
implied, of certain responsibilities, in return for certain |
membership. |
|
|
|
|
|||||||
|
|
|
|
|
ELSEVIER |
|
|
|
||||||
|
|
privileges. These responsibilities require certain beha- |
|
While the principles of professionalism should be |
||||||||||
|
|
viours and attitudes of individuals in whom profes- |
aspired to by physiotherapists anywhere in the world, |
|||||||||||
|
|
sional trust is placed. Broadly, professionalism requires |
the existence and/or role of regulators and professional |
|||||||||||
|
|
these attributes: |
|
OF |
|
|
bodies and the way these characteristics are manifested |
|||||||
|
|
|
|
|
|
may vary, depending on political, social and financial |
||||||||
|
▪ a motivation to deliver service to others |
|
|
|||||||||||
|
|
|
factors. |
|
|
|
|
|
|
|||||
|
▪ adherence to a moral and ethical code of practice |
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
||||||
|
▪ striving for excellence, maintaining an awareness of |
|
Belonging to an organisation that sets |
|||||||||||
|
|
limitations and scope of practice |
|
|
|
|
||||||||
|
|
|
|
|
|
standards and ideals of behaviour |
||||||||
|
▪ the empowerment of others (Hodkinson 1995 and |
|
||||||||||||
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
CONTENT |
|
|
|
|
|
|||||
|
|
Medical Professionalism Project 2002, both cited in |
|
The Rules of Professional Conduct (the Rules) were |
||||||||||
|
|
CSP 2005b). |
|
|
|
|
|
endorsed at the very first council meeting of the CSP |
||||||
|
|
To practise in the |
profession of |
physiotherapy |
in |
|
in 1895 |
(Barclay 1994) |
|
and have been revised and |
||||
|
|
|
updated at intervals since. The Rules define the profes- |
|||||||||||
|
the UK, registration |
with the statutory regulator |
is |
|
||||||||||
|
|
sional behaviour expected of chartered physiothera- |
||||||||||||
|
required. The Health Professions Council (HPC) sets |
|
||||||||||||
|
|
pists. The current Rules set out a number of principles, |
||||||||||||
|
standards of professional training, |
performance and |
|
|||||||||||
|
|
the basis for all of which is to safeguard patients (CSP |
||||||||||||
|
conductPROPERTYfor thirteen professions, including physiother- |
|
||||||||||||
|
|
2002a). |
They include |
requirements that chartered |
||||||||||
|
apy (HPC 2006). It keeps a register of health profes- |
|
||||||||||||
|
|
physiotherapists should: |
|
|
|
|||||||||
|
sionals that meet its standards, and it takes action if |
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
||||||
|
|
SAMPLE |
|
|
▪ respect the dignity and individual sensibilities of |
|||||||||
|
registered health professionals do not meet those stan- |
|||||||||||||
|
dards. It was created by the Health Professions Order |
|
every patient |
|
|
|
|
|||||||
|
2001 (HPC 2002). Only those registered with the HPC |
▪ work safely and competently |
||||||||||||
|
may call themselves a physiotherapist/physical thera- |
▪ ensure the confidentiality of patient information |
||||||||||||
|
pist (HPC 2006). It is the duty of registrants to keep |
▪ report circumstances that might otherwise put |
||||||||||||
|
up to date with the processes and requirements decreed |
|
patients at risk |
|
|
|
||||||||
|
by the Regulator; this is particularly important currently |
▪ not exploit patients |
|
|
|
|||||||||
|
because of the changing attitudes to, and legislation of, |
▪ act in a way that reflects credit on the profession and |
||||||||||||
|
healthcare professions in recent times. |
|
|
|
does not cause offence to patients. |
|||||||||
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926

Porter: Tidy's Physiotherapy, 14th Edition
Characteristics of being a professional 3
on informed consent. This is a good example of how
the Standards and Rules complement each other. They 1 should be used together to ensure compliance with
the characteristics and actions required of members of the physiotherapy profession.
Commitment to discipline other members
As of 15 October 2006 the CSP no longer handles com- plaints concerning the professional conduct or fitness to
▪ involving patients in |
|
|
practise of its members, except those described in the |
|||||||||
▪ being fully abreast of the evidence of effectiveness |
||||||||||||
next paragraph. The HPC considers all complaints of |
||||||||||||
in order to inform patients and offer the most effec- |
||||||||||||
this nature. |
|
|
||||||||||
tive interventions |
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
The Society |
does however, handle complaints or |
|||||
▪ evaluating their practice and measuring a patient’s |
||||||||||||
consider matters of fitness to practise concerning mem- |
||||||||||||
health gain as a result of treatment. |
|
|
|
|||||||||
|
|
|
bers of the Society who are not regulated by the HPC. |
|||||||||
|
|
|
|
|
|
|
|
|
||||
This reflects the increasing expectations of the public to |
(This includes physiotherapist’s physiotherapy treat- |
|||||||||||
be active partners in their healthcare, the expectations |
ment of animals, students and the CSP’s associate |
|||||||||||
of clinical governance to provide more effective care, |
members (CSP 2006).) |
FINAL |
||||||||||
and the growing demands of funders of services, as |
|
|
||||||||||
Possessing knowledge and skills not shared |
||||||||||||
well as patients, to be able to demonstrate the benefits |
||||||||||||
by others |
|
|
||||||||||
or ‘added value’ of physiotherapy. All these will be dis- |
|
|
||||||||||
|
|
|
||||||||||
|
|
|
||||||||||
cussed later in the chapter. |
|
|
|
|
|
Any profession possesses a range of specific knowledge |
||||||
Standards of Physiotherapy Practice is written in a way |
and skills that are either unique, or more significantly |
|||||||||||
that offers a broad statement of intent (the Standard |
|
NOT |
|
|||||||||
developed than in other professions. The World Congress |
||||||||||||
statement), which is followed by a number of measur- |
- |
|
|
|||||||||
for Physical Therapy (WCPT) has described the nature of |
||||||||||||
able statements about expected performance or activity |
physiotherapy as ‘providing services to people and popu- |
|||||||||||
|
|
|
|
|
|
|
|
ELSEVIER |
|
|||
by the physiotherapist, student or assistant (known as |
lations to develop, maintain and restore maximum move- |
|||||||||||
‘criteria’). For example, Core Standard 2 states ‘Patients |
ment and functional ability throughout the lifespan’ |
|||||||||||
are given relevant information about the proposed |
(WCPT 1999). |
|
|
|||||||||
physiotherapy |
procedure, |
taking into account |
their |
It adds, in a detailed description, that physical ther- |
||||||||
|
|
|
|
|
|
OF |
|
apy is ‘concerned with identifying and maximising |
||||
age, emotional state and cognitive ability, to allow |
||||||||||||
informed consent.’ The criteria for this standard include |
movement potential, within the spheres of promotion, |
|||||||||||
the following: |
|
|
|
|
|
|
|
prevention, treatment and rehabilitation’ (ibid, p28). |
||||
▪ The patient’s consent is obtained before starting any |
WCPT identifies the interaction between ‘physical |
|||||||||||
therapist, patients or clients, families and care givers, |
||||||||||||
|
|
|
|
|
|
|
|
|
||||
examination/treatment. |
|
|
CONTENTin a process of assessing movement potential and in |
|||||||||
▪ Treatment |
options, including |
significant |
benefits, |
establishing agreed upon goals and objectives’ as cru- |
||||||||
risks and |
||||||||||||
cial and acknowledges that |
this requires knowledge |
|||||||||||
▪ The patient |
is |
given |
the |
opportunity |
to |
ask |
||||||
and skills unique to physical therapists (ibid, p28). |
||||||||||||
questions. |
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
In the UK, |
one approach |
to conceptualising phy- |
||
▪ The patient is informed of the right to decline phys- |
||||||||||||
siotherapy has been to focus on three core elements: mas- |
||||||||||||
iotherapy |
at |
any |
stage |
without that prejudicing |
||||||||
sage, exercise and electrophysical modalities (CSP 2002a). |
||||||||||||
future care. |
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
For physiotherapy, the roots of the profession can be |
|||||
PROPERTY |
|
|
|
|||||||||
▪ The patient’s consent to the treatment plan is docu- |
found in massage, the founders of the profession having |
|||||||||||
mented in the patient’s record. |
|
|
|
|
||||||||
|
|
|
|
been a group of nurses who carried out massage. The sig- |
||||||||
|
SAMPLE |
|
|
|
||||||||
|
|
|
|
nificance of therapeutic touching of patients still sets |
||||||||
These measurable criteria allow performance to be |
||||||||||||
assessed against them, through clinical audit, described |
physiotherapy aside from other professions. Physiothera- |
|||||||||||
in more detail later. |
|
|
|
|
|
|
pists continue to use massage therapeutically as well as a |
|||||
The content of this standard and accompanying |
wide range of other manual techniques such as manipu- |
|||||||||||
criteria set out the specific actions required in order to |
lation and reflex therapy. Therapeutic handling under- |
|||||||||||
conform, in this case, to an aspect of Rule 2 of Rules of |
pins many aspects of rehabilitation, requiring the |
|||||||||||
Professional Conduct: ‘Chartered physiotherapists shall |
touching of patients to facilitate movement. |
|||||||||||
respect and uphold the rights, dignity and individual |
Another description of the profession’s knowledge |
|||||||||||
sensibilities of every patient,’ which includes guidance |
and skills can be found in the Curriculum Framework |
|||||||||||
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
4THE RESPONSIBILITIES OF BEING A PHYSIOTHERAPIST
1 |
|
for Qualifying Programmes in Physiotherapy (CSP 2002b). |
the ability to think critically about practice, to learn |
||||||||
|
This sets out the underpinning knowledge and skills |
from experience and apply that learning to future sit- |
|||||||||
|
|
required of newly qualifying physiotherapists, setting |
uations. It is the relationship between the physiothera- |
||||||||
|
|
this in the context of their application in professional |
pist’s knowledge, his or her ability to collect, analyse |
||||||||
|
|
practice areas and environments. These are, in turn, |
and synthesise relevant information (cognition), and |
||||||||
|
|
underpinned by a set of professional attributes, identity |
personal awareness, |
||||||||
|
|
and relationships, such as understanding the scope of |
processes, or metacognition (Jones et al. 2000). |
|
|||||||
|
|
practice and active engagement with patient partner- |
This professional autonomy has, however, to be |
||||||||
|
|
ship. Finally, the framework sets out the outcomes that |
balanced with the autonomy patients have to make |
||||||||
|
|
graduates should be able to demonstrate: for example, |
their own decisions. |
||||||||
|
|
‘enable individual patients and groups to optimise their |
partnership between patient and professional, sharing |
||||||||
|
|
health and social |
information, with patients’ values and experience being |
||||||||
|
|
ately to changing demands’. |
|
|
|
|
|
treated as equally important as clinical knowledge |
|||
|
|
|
|
|
|
|
|
and scientific facts (Ersser and Atkins 2000). Higgs and |
|||
‘ |
|
|
|
|
|
|
|
|
|
||
|
Definition |
|
|
|
|
|
Titchen (2001) describe the notion of the professional’s |
||||
|
|
Physiotherapy is a healthcare profession concerned |
|
|
role as a ‘skilled companion’. The professional is char- |
||||||
|
|
with human function and movement and maximising |
|
|
acterised as a person with specialised knowledge which |
||||||
|
|
potential. It uses physical approaches to promote, |
|
|
can be shared with the patient in a reciprocal ‘working |
||||||
|
|
maintain and restore physical, psychological and social |
|
|
|
|
FINAL |
|
|||
|
|
|
|
with’ rather than ‘doing to’ relationship, and as someone |
|||||||
|
|
|
who ‘accompanies the patient on their journey towards |
||||||||
|
|
It is |
|
|
health, adjustment, coping or death’. This patient- |
||||||
|
|
evaluating and reviewing the evidence that underpins |
|
|
centred model facilitates the sharing of power and |
||||||
|
|
and informs its practice and delivery. The exercise of |
|
|
responsibility between professional and patient. |
|
|||||
|
|
clinical judgement and informed interpretation is at its |
|
|
|
NOT |
|
|
|||
|
|
|
|
A history of how the physiotherapy profession’s |
|||||||
|
|
core (CSP 2002b). |
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
autonomy evolved in the UK can be found later in this |
||||
|
|
|
|
|
|
|
|
chapter. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ELSEVIER |
|
|
|||
|
|
Cott et al. (1995) have proposed an overarching |
|
|
|
|
|||||
|
framework for the profession: the movement continuum |
Licensed by the state |
|
|
|||||||
|
theory of physical therapy, |
arguing that the |
way in |
|
|
|
|
||||
|
As previously mentioned, physiotherapists in the UK |
||||||||||
|
which physiotherapists conceptualise movementOFis what |
||||||||||
|
have to be registered with the HPC in order to use the |
||||||||||
|
differentiates the profession from others. They suggest |
||||||||||
|
title physiotherapist and therefore to work in any setting |
||||||||||
|
that physiotherapists conceive of movement on a contin- |
||||||||||
|
in the UK. This is a government measure to protect |
||||||||||
|
uum from a micro (molecular, cellular) to a macro (the |
||||||||||
|
patients from unqualified or inadequately skilled health- |
||||||||||
|
person in his or her environment or in society) level. |
||||||||||
|
care providers. |
|
|
|
|||||||
|
The authors argue that the theory is a unique approach |
|
|
|
|||||||
|
|
|
|
|
|||||||
|
to movement rehabilitation |
|
CONTENTIn 2006, the HPC put in place a system requiring |
||||||||
|
because it incorporates |
||||||||||
|
knowledge of pathology with a holistic view of move- |
||||||||||
|
individual’s commitment to |
Continuing Professional |
|||||||||
|
ment, which includes the influence of physical, social |
||||||||||
|
Development (CPD), whereby individuals must under- |
||||||||||
|
and psychological factors in an assessment of a person’s |
||||||||||
|
take and maintain a record of their CPD activities and, |
||||||||||
|
maximum achievable movement potential. They argue |
||||||||||
|
if required, submit evidence |
of this and of the |
out- |
||||||||
|
that the role of physiotherapy is to minimise the differ- |
||||||||||
|
comes of their CPD on their practice, service |
users |
|||||||||
|
ence between a person’s current movement capability |
||||||||||
|
and service. |
||||||||||
|
|
PROPERTY |
|
|
|
|
|||||
|
and his or her preferred movement capability. |
|
|
|
ing of public confidence in the National Health Service |
||||||
|
|
Exercising autonomySAMPLE |
|
|
|
|
|||||
|
|
|
|
|
|
(NHS) following, for example, the report into children’s |
|||||
|
|
|
|
|
|
heart surgery in Bristol (Bristol Royal Infirmary Inquiry |
|||||
|
|
Autonomy, or ‘personal freedom’ (Concise Oxford |
|||||||||
|
|
2001). Equally disturbing were the revelations about |
|||||||||
|
|
Dictionary, 7th edn) is a key characteristic of being a |
the murders of so many patients by Harold Shipman, a |
||||||||
|
|
professional. It allows independence, but is mirrored |
man who had been a previously trusted general practi- |
||||||||
|
|
by a responsibility and accountability for action. Cen- |
tioner, where health systems failed to detect an unusu- |
||||||||
|
|
tral to the practice of professional autonomy is clinical |
ally high number of deaths (Department of Health 2004). |
||||||||
|
|
reasoning, described as the ‘thinking and decision- |
This has led the government to introduce a number |
||||||||
|
|
making processes associated with clinical practice’ |
of measures, including the requirement for all health |
||||||||
|
|
(Higgs and Jones 2000). Clinical reasoning |
requires |
professionals to |
|||||||
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
|
|
|
|
|
|
Responsibilities of being a professional |
5 |
|||||
|
|
|
|
|||||||||
|
|
|
|
|
||||||||
order to be seen to be protecting the public through a |
about meeting needs. Being a professional is a |
|
|
|||||||||
|
1 |
|||||||||||
more explicit and independent process (Department |
privilege |
|
in particular the trust that is bestowed by |
|
||||||||
of Health 2002). It aims to identify poor performers |
the public |
which underpins |
the patient’s ability to |
|
|
|||||||
who may be putting the public at risk, as well as |
benefit from treatment. However, this brings with it |
|
|
|||||||||
providing an incentive for professionals to keep up to |
weighty responsibilities. |
|
|
|
|
|
||||||
date, maintaining and further developing their scope |
|
|
|
|
|
|
|
|
|
|||
of practice and competence to do their job. Disciplinary |
Doing only those things you are competent |
|
|
|||||||||
processes are in place to remove, ultimately, an indi- |
|
|
||||||||||
to do |
|
|
|
|
|
|
|
|
||||
vidual from the register (HPC 2005). The means by |
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
||||
Every physiotherapist has her or his own personal |
|
|
||||||||||
which individuals can maintain their competence are |
|
|
||||||||||
discussed later in the chapter. |
‘scope of practice’ (CSP 2002a) |
that is, a range (or |
|
|
||||||||
|
|
|
|
|
|
|
|
FINAL |
|
|
||
|
|
|
|
scope) of professional knowledge and skills that can |
|
|
||||||
Making a commitment to assist those in need |
be applied competently within specific practice settings |
|
|
|||||||||
As stated earlier, one of the characteristics of a profes- |
or populations. |
|
|
|
|
|
|
|||||
|
|
|
|
When a person is newly qualified, this scope will be |
|
|
||||||
|
|
ELSEVIER |
|
|
|
|
|
|||||
sional is to want to ‘do good’. This is reflected in the |
based on the content of the |
|
|
|||||||||
ethical principles of |
the physiotherapy profession, |
Framework, but will also be informed by the indivi- |
|
|
||||||||
where there is a ‘duty of care’ incumbent on the indi- |
dual’s experience in clinical placements, and the amount |
|
|
|||||||||
vidual towards the patient, to ensure that the therapeu- |
of teaching and reflective learning that has been possible |
|
|
|||||||||
tic intervention is intended to be of benefit, as set out |
as part of those placements. |
|
|
|
|
|
||||||
in Rule 1 (CSP 2002a). This is a |
As a |
career progresses, |
and as a |
result of CPD, |
|
|
||||||
a breach of which (negligence) could lead to a civil |
|
|
||||||||||
some physiotherapists will become competent in high- |
|
|
||||||||||
claim for damages. |
|
|
|
|
||||||||
|
|
ly skilled areas such as intensive care procedures, or |
|
|
||||||||
|
More generally, Koehn (1994) suggests, professionals |
|
- |
NOT |
|
|
|
|
|
|||
|
|
|
|
splinting |
for |
children with |
cerebral palsy, which |
|
|
|||
▪ demand from the client the responsibilityCONTENTto provide, |
|
|
|
|
|
|
|
|||||
are perceived to have moral authority, or trustworthi- |
are unlikely to have been taught before qualification. |
|
|
|||||||||
ness, if they: |
|
|
Others will extend their skills in areas in which they |
|
|
|||||||
▪ use their skills in |
the context of the client’s best |
already had some experience: for example, dealing with |
|
|
||||||||
|
interests and ‘doing good’ |
people with neurological problems. Others will enhance |
|
|
||||||||
▪ are willing to act as long as it takes for assistance |
their communication and life skills, as well as refining |
|
|
|||||||||
|
to achieve what it set out to achieve, orOFfor a decision |
their physiotherapy skills by, for example, working |
|
|
||||||||
|
PROPERTY |
constantly evolving, based on professional and life |
|
|
||||||||
|
to be made that nothing more can be done to help |
with elderly people or people with learning difficulties. |
|
|
||||||||
|
the client |
|
|
It is the responsibility of the professional to under- |
|
|
||||||
▪ have a highly developed internalised sense of respon- |
stand his or her personal scope of practice as it changes |
|
|
|||||||||
|
sibility to monitor personal behaviour: for example, |
and evolves throughout a career. To practise in areas in |
|
|
||||||||
|
by not taking advantage of vulnerable patients |
which you are not competent puts patients at risk and |
|
|
||||||||
|
SAMPLE |
is a breach of the CSP’s Rules of Professional Conduct, |
|
|
||||||||
|
for example, sufficient information to allow decisions |
and the |
standards of the profession’s regulator, the |
|
|
|||||||
|
HPC (2003). |
|
|
|
|
|
|
|
||||
|
to be made (compliance) |
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|||
▪ are allowed to exercise discretion (judgement) to do |
|
|
|
|
|
|
|
|
|
|||
|
the best for the client, within limits. |
Maintaining competence to practise |
|
|
||||||||
|
Koehn (1994) argues |
that trustworthiness is what |
|
|
|
|
|
|
|
|
|
|
|
An individual’s scope of practice and competence are |
|
|
|||||||||
|
stands out as a particularly unique characteristic of |
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|||
|
being a professional |
to do good, to have the patient’s |
experiences, |
learning from |
reading, |
from evaluating |
|
|
||||
|
best interests at heart and to have high ethical stan- |
|
|
|||||||||
|
practice, |
from |
reflecting on |
practice, |
or more formal |
|
|
|||||
|
dards. Physiotherapists not prepared to maintain such |
|
|
|||||||||
|
ways of learning. It includes undertaking programmes |
|
|
|||||||||
|
ethics, even in difficult and stressful situations, run |
|
|
|||||||||
|
of structured CPD. Clinical reasoning skills are contin- |
|
|
|||||||||
|
the risk of losing the respect as well as the trust of their |
|
|
|||||||||
|
ually refined |
and further |
developed throughout a |
|
|
|||||||
|
patients and the public. |
|
|
|||||||||
|
career through evaluative and reflective practice, lead- |
|
|
|||||||||
|
|
|
|
|
|
|||||||
|
|
|
|
ing to the ability to deal with increasingly complex |
|
|
||||||
RESPONSIBILITIES OF BEING A PROFESSIONAL |
and unpredictable situations. |
|
|
|
|
|||||||
Physiotherapists have a duty to keep up to date |
|
|
||||||||||
|
|
|
|
|
|
|||||||
Physiotherapists in the UK are granted the right to |
with new information generated by research, with what |
|
|
|||||||||
make their own decisions, in partnership with patients, |
their peers are thinking and doing, and by formally |
|
|
|||||||||
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
6THE RESPONSIBILITIES OF BEING A PHYSIOTHERAPIST
1 |
|
evaluating the outcome of their practice. The responsi- |
standards (CSP 2005a). Where they do not, programmes |
|||||||||||
|
bility for this is dictated by the |
HPC |
(2003) and |
of professional development should be put in place |
||||||||||
|
|
reflected in the Standards of Physiotherapy Practice (CSP |
to facilitate full compliance, as part of the individual’s |
|||||||||||
|
|
2005a). In particular, Core Standards 19 22 are con- |
professional responsibility. |
|
|
|
||||||||
|
|
cerned with a requirement that individuals assess their |
Physiotherapists should not be critical of each other, |
|||||||||||
|
|
learning needs, then plan, implement and evaluate a |
except in extreme circumstances. However, they do |
|||||||||||
|
|
programme of CPD based on that assessment. |
|
|
|
have a duty to report circumstances that could put |
||||||||
|
|
|
|
|
|
|
|
|
|
patients at risk. In the NHS, there are procedures and |
||||
|
|
Responsibility to patients |
|
|
|
|
|
|
a nominated officer within each trust from whom |
|||||
|
|
|
|
|
|
|
|
|
|
advice can be sought. Outside the NHS, advice can be |
||||
|
|
This chapter has already discussed the importance of |
||||||||||||
|
|
sought from the CSP. Physiotherapists are encouraged |
||||||||||||
|
|
the individual physiotherapist as well as the profession |
||||||||||||
|
|
to be proactive in supporting each other’s professional |
||||||||||||
|
|
as a whole in maintaining the attributes of |
profes- |
|||||||||||
|
|
development and in promoting the value of the profes- |
||||||||||||
|
|
sionals. Trust is perhaps the most essential characteris- |
||||||||||||
|
|
sion in local workplace |
settings, in |
|||||||||||
|
|
tic with which to develop a sense of partnership with |
||||||||||||
|
|
forums and in the media. |
|
|
|
|||||||||
|
|
patients; in turn, this will optimise the benefits of inter- |
|
|
|
|||||||||
|
|
|
|
|
|
|
||||||||
|
|
vention. For physiotherapy, many of the other hall- |
|
|
|
|
|
|||||||
|
|
marks for building and securing trust are set out in |
BECOMING AN AUTONOMOUS PROFESSION |
|||||||||||
|
|
the profession’s Rules and Standards. For example: |
|
|
|
|
|
FINAL |
|
|||||
|
|
|
|
The CSP was founded in 1894, under the name of the |
||||||||||
|
|
|
|
|
|
|
|
|
|
|||||
|
▪ to provide safe and effective interventions (safety of |
Society of Trained Masseuses. This section will not |
||||||||||||
|
|
application as well as safe and effective) |
Rule 1 |
attempt to relate the history of the profession, except |
||||||||||
|
|
and Core Standards 4, 8, 16 |
|
|
|
|
|
|
in the context of developing autonomy. However, more |
|||||
|
▪ to treat patients with dignity and respect |
Rule 2 |
about the early days of the profession can be found in |
|||||||||||
|
|
and Core Standard 1 |
|
|
|
|
|
|
|
|
NOT |
|
|
|
|
|
|
|
|
|
|
|
|
the book In Good Hands (Barclay 1994). |
|||||
|
▪ to provide patients with information about their |
- |
|
|
|
|
||||||||
|
For many years, doctors governed the profession. |
|||||||||||||
|
|
options for treatment/interventions |
|
Rule 2 and |
One of the first rules of professional conduct stated |
|||||||||
|
|
Core Standard 2 |
|
|
|
|
|
ELSEVIER |
|
|
|
|||
|
|
|
|
|
|
|
|
|
‘no massage to be undertaken except under medical |
|||||
|
▪ to involve patients in decisions about their treatment |
direction’ (ibid). Even in the 1960s doctors were assert- |
||||||||||||
|
|
(informed consent) |
Rule 2 and Core Standard 2. |
ing that they must take full responsibility for patients |
||||||||||
|
|
|
|
|
OF |
|
|
in their charge |
and ‘professional and technical staff |
|||||
|
|
|
|
|
|
|
have no right to challenge [the doctor’s] views; only |
|||||||
|
|
Responsibility to those who pay for services |
|
|
||||||||||
|
|
Physiotherapists have an ethical responsibility to those |
he is equipped to decide how best to get the patients |
|||||||||||
|
|
fit again’ (ibid). It is hard to believe now that it took |
||||||||||||
|
|
who finance services, whether these are commissioners |
||||||||||||
|
|
more than 80 years to escape the paternalism of doctors, |
||||||||||||
|
|
of healthcare, taxpayers or individual patients, to pro- |
||||||||||||
|
|
on whom physiotherapists were dependent for referrals. |
||||||||||||
|
|
vide efficiently delivered, clinically and |
||||||||||||
|
|
|
|
|
|
|
||||||||
|
|
interventions and services, in order |
|
CONTENTThe first breakthrough came in the early 1970s, when a |
||||||||||
|
|
to give value in |
report by the Remedial Professions Committee, chaired |
|||||||||||
|
|
an era when resources for healthcare are limited. This |
||||||||||||
|
|
by Professor Sir Ronald Tunbridge, included a state- |
||||||||||||
|
|
is embedded within Rule 1 of the CSP’s Rules of Profes |
||||||||||||
|
|
ment that while the doctor should retain responsibility |
||||||||||||
|
|
sional Conduct in relation to the establishment of a ‘duty |
||||||||||||
|
|
for prescribing |
treatment, |
more scope in application |
||||||||||
|
|
of care’ towards the patient (CSP 2002a). |
|
|
|
|
||||||||
|
|
|
|
|
|
and duration should be given to therapists. |
||||||||
|
|
|
|
|
|
|
|
|
|
|||||
|
|
Responsibility to colleagues and |
|
|
|
|
|
The McMillan report (DHSS 1973) went further, by |
||||||
|
|
|
|
|
|
|
recommending |
that therapists should be allowed to |
||||||
|
|
PROPERTY |
|
|
|
|
|
|||||||
|
|
the profession |
|
|
|
|
|
|
|
decide the nature and duration of treatment, although |
||||
|
|
|
|
|
|
|
|
|
|
|||||
|
|
A profession has legitimate expectations of its members |
doctors would remain responsible for the patient’s wel- |
|||||||||||
|
|
SAMPLE |
|
|
|
|
|
fare. There was recognition that doctors who referred |
||||||
|
|
to conduct themselves in a way that does not bring the |
||||||||||||
|
|
profession into disrepute, but rather enhances public |
patients would not be skilled in the detailed application |
|||||||||||
|
|
perceptions. Physiotherapists have a duty to inform |
of particular techniques, and that the therapist would |
|||||||||||
|
|
themselves of what is expected of them. Indeed, the |
therefore be able to operate more effectively if given |
|||||||||||
|
|
Rules of Professional Conduct state that knowledge of |
greater responsibility and freedom. |
|||||||||||
|
|
and adherence to the Rules are part of the contract of |
Eventually, a Health Circular called Relationship |
|||||||||||
|
|
membership of the CSP. The Standards of Physiotherapy |
between the Medical and Remedial Professions was issued |
|||||||||||
|
|
Practice make it clear there is an expectation that all |
(DHSS, 1977). This acknowledged the therapist’s com- |
|||||||||||
|
|
physiotherapists should be able to achieve all the core |
petence and responsibility for deciding on the nature |
|||||||||||
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
7
‘Definition
of the treatment to be given. It recognised the ability of |
The accountability of chief executives |
|
|
1 |
|||||
the physiotherapist to determine the most appropriate |
for quality |
|
|
|
|||||
intervention for a patient, based on knowledge over |
|
|
|
||||||
Although some chief executives of NHS trusts claim |
|||||||||
and above that which it would be reasonable to expect |
|||||||||
they were always responsible for quality, this had not |
|||||||||
a doctor to possess. It also recognised the close relation- |
|||||||||
been a statutory responsibility in the way it was for a |
|||||||||
ship between therapist and patient, and the importance |
|||||||||
trust’s finances. Chief executives now have a statutory |
|||||||||
of the therapist interpreting and adjusting treatment |
|||||||||
responsibility for quality. |
|
|
|
||||||
according to immediate patient responses. |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|||
Autonomy was only achieved by being able to |
The introduction of a philosophy of |
|
|
|
|||||
demonstrate competence to make appropriate deci- |
continuous improvement |
|
|
|
|||||
sions, building up the trust of doctors and those paying |
the NHS |
||||||||
for physiotherapy services. The need to acquire skills |
|||||||||
has to move to a culture of continuous improvement |
|||||||||
of assessment and analysis became a key component |
|||||||||
to achieve excellence. In addition, the emphasis |
has |
||||||||
of student programmes from the 1970s. Today, qualify- |
|||||||||
shifted from improving a particular aspect of care in |
|||||||||
ing programmes stress even further the development |
|||||||||
isolation, to examining the whole system of care, cross- |
|||||||||
of skills, knowledge and attributes required for auto- |
|||||||||
ing professions, departments, organisations |
and |
sec- |
|||||||
nomous practice. |
|
|
|
||||||
|
|
|
tors, to ensure the whole process meets the needs of |
||||||
|
|
|
|
||||||
|
|
|
|
patients through an integratedFINALapproach to healthcare. |
|||||
CLINICAL GOVERNANCE |
|
|
|
An aspiration to achieve consistency of services |
|||||
So far, this chapter has explored the responsibilities |
across the NHS |
|
|
|
|||||
of being a physiotherapist from a professional perspec- |
This is founded on two principles: |
|
|
|
|||||
tive. The focus has been on the individual’s personal |
|
NOT |
|
|
|
||||
|
|
|
|
|
|
|
|
||
responsibility as a professional. This section will put |
▪ If one trust can provide excellence in a service, then |
||||||||
- |
|
|
|
|
|||||
|
|
|
|
|
|
|
|
||
all that in the context of a professional’s responsibilities |
so can all trusts. |
|
|
|
|||||
▪ Local services should, where possible, be based on |
|||||||||
to the employer organisation, whether it be in the public |
|||||||||
|
|
ELSEVIER |
|
|
|
||||
or the independent sector. |
|
|
|
national standards: for example, National Service |
|||||
|
|
|
Frameworks or nationally developed clinical guide- |
||||||
In the NHS, responsibility for the clinical safety of |
|||||||||
lines. |
|
|
|
|
|||||
patients and the quality and effectiveness of services |
|
|
|
|
|||||
|
|
|
|
|
|||||
is maintained via a system of clinical governance. It |
There is some evidence to suggest that nationally devel- |
||||||||
|
OF |
|
|
||||||
seems probable this will apply equally to the indepen- |
oped standards or clinical guidelines are likely to be |
||||||||
dent sector in the near future. However, even though |
|||||||||
more robustly developed (Sudlow and Thomson 1997) |
|||||||||
clinical governance is the responsibility of NHS trusts, |
|||||||||
and that their universal implementation locally |
will |
||||||||
its foundation is based on ‘the principle that health pro- |
|||||||||
ensure consistency and effectiveness. |
|
|
|
||||||
fessionals must be responsible and accountable for their |
|
|
|
||||||
|
|
|
|
|
|||||
own practice’ (Secretary of State for HealthCONTENT1998). The An emphasis on continuing professional |
|
|
|
||||||
individual’s professional responsibility is therefore still |
development (CPD) and |
||||||||
paramount. |
|
|
|
Clinical governance acknowledges the importance of |
|||||
|
|
|
|
||||||
What is clinical governance? |
|
|
|
CPD/LLL for all healthcare workers, in order to keep |
|||||
|
|
|
up to date and deliver |
|
|
|
|||
PROPERTY |
|
|
|
|
|
|
|
|
|
the quality ofSAMPLEtheir services and safeguarding high |
|
|
|
|
|
|
|
||
Clinical governance is a framework through which NHS organisations are accountable for continuously improving
standards of care by creating an environment in which excellence in clinical care will flourish (Secretary of State for Health 1998). (While this definition has been used in England, similar interpretations of the term have been made in Scotland, Wales and Northern Ireland.)
A number of key themes were introduced as part of clinical governance.
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
8THE RESPONSIBILITIES OF BEING A PHYSIOTHERAPIST
1 |
|
and trusts more readily for mistakes, thus drawing |
|
In 1991, Sir Michael Peckham, then Director of |
||||||||||||
|
money away from |
|
Research and Development for the Department of |
|||||||||||||
|
|
governance is about rebuilding the public’s confidence |
|
Health, noted that ‘strongly held views based on belief |
||||||||||||
|
|
in health services, providing |
|
rather than sound information still exert too much |
||||||||||||
|
|
care and, above all, reducing the risk of harm through |
|
influence in healthcare. In some instances the relevant |
||||||||||||
|
|
negligence, poor performance or system failures. |
|
|
|
knowledge is available but is not being used, in other |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
situations additional knowledge needs to be generated |
||
|
|
The components of clinical governance |
|
|
|
from reliable sources’ (Department of Health 1991). At |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
about the same time, a relatively small group of doctors |
||
|
|
Although clinical governance should be seen as a pack- |
|
|||||||||||||
|
|
|
began to write about |
|||||||||||||
|
|
age of measures that together ensure excellence and a |
|
|||||||||||||
|
|
|
|
FINAL |
||||||||||||
|
|
reduction in risk, it can also be viewed as a number of |
|
|
||||||||||||
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
‘ |
|
|
|
|
|
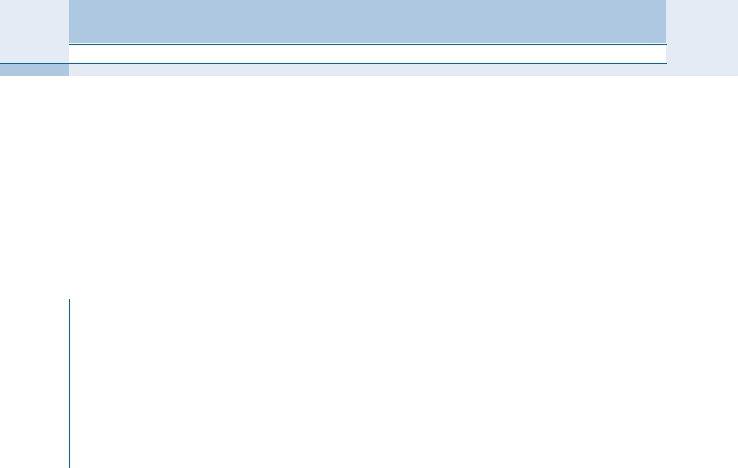
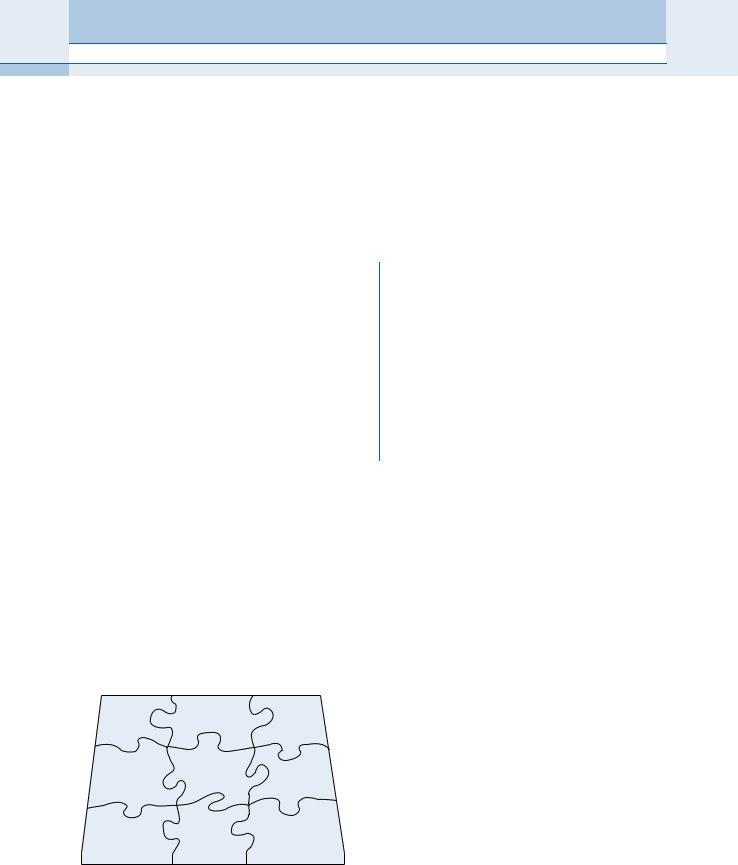
component parts, some of which have been in place for |
Definition |
|
|
|||||||||||
|
|
a number of years and are already familiar (Figure 1.1). |
|
An early definition of |
|
|||||||||||
|
|
They include: |
|
|
|
|
|
|
|
|
|
that it is the ‘conscientious, explicit and judicious use |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
ELSEVIER |
|
|
||
|
▪ |
|
|
of current best evidence in making decisions about |
|
|||||||||||
|
▪ applying national standards and guidelines locally |
|
the care of individual patients’ (Sackett et al. 1996). |
|
||||||||||||
|
▪ evaluating the effectiveness and quality of services |
|
A recent definition has updated this, drawing on |
|
||||||||||||
|
▪ continuing |
|
professional |
|
|
criticisms of the initial position and stating that |
|
|||||||||
|
|
|
learning |
|
|
|
|
|
|
|
|
|
|
|||
|
▪ having the right workforce and using it appropri- |
|
health care are based on the best available, current, |
|
||||||||||||
|
|
valid and relevant evidence. These decisions should be |
|
|||||||||||||
|
|
|
ately. |
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
made by those receiving care, informed by the tacit |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
The following sections deal with these aspects. |
|
|
|
and explicit knowledgeNOTof those providing care, within |
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
the |
|
|
|
|
|
|
CONTENTus about their condition, which treatments they find effec- |
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What do we mean by evidence? Is research the only |
||
|
|
At the beginning of this chapter, it was asserted that |
|
|||||||||||||
|
|
form of evidence? Certainly for some questions, such |
||||||||||||||
|
|
people |
who |
want to become |
physiotherapists |
have |
||||||||||
|
|
as the efficacy of particular drugs, or a particular modality |
||||||||||||||
|
|
an inherent desire to ‘do good’. But how do we know |
||||||||||||||
|
|
such as exercise programmes for the management of back |
||||||||||||||
|
|
|
|
PROPERTY |
|
|
|
|||||||||
|
|
|
|
|
|
|
encounter, will develop such expertise (Jones et al. |
|||||||||
|
|
what works |
what interventions have OFbeen shown |
pain, research studies which compare one intervention |
||||||||||||
|
|
to be effective? It is hard to comprehend that health |
with another or a placebo (randomised controlled trials) |
|||||||||||||
|
|
professionals have not always sought evidence for the |
can provide reliable information about the degree to |
|||||||||||||
|
|
effectiveness of the treatments they use. Perhaps they |
which an intervention is effective. But other forms of evi- |
|||||||||||||
|
|
did |
but until |
the early 1990s this ‘evidence’ |
was |
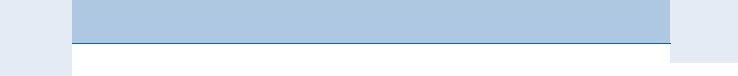
dence are also important (Figure 1.2). What patients tell |
||||||||||
|
|
based on personal experience and on opinions derived |
||||||||||||||
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
SAMPLE |
|
|
|
|
|
|
|
|
|||
|
|
from that experience, together with the experience of |
tive, the degree to which interventions improve their abil- |
|||||||||||||
|
|
colleagues, or those perceived to be experts and opin- |
ity to get on with their lives also provides important |
|||||||||||||
|
|
ion leaders. Is that good enough? |
|
|
|
|
evidence. The physiotherapist also contributes evidence |
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
in the form of clinical expertise, derived from clinical |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
reasoning experience. Thinking and reflecting on what |
|||
|
|
|
|
Evidence- |
Clinical audit |
|
|
|
Using |
|
|
you are doing, as a practitioner during or after a clinical |
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
based |
|
|
|
|
|
patient |
|
|
|
|
|
|
|
|
|
|
practice |
|
|
|
|
feedback |
|
|
2000). Knowledge which arises from and within practice |
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
Using nationally |
Continuing |
|
|
|
Clinical |
|
|
become part, along with research evidence, of your ratio- |
|||||
|
|
|
developed |
|
professional |
|
|
|
|
|
nale for practice (Higgs and Titchen 2001). Sackett and |
|||||
|
|
|
standards |
|
|
|
effectiveness |
|
|
|||||||
|
|
|
|
development |
|
|
|
|
colleagues reflected this in concluding their definition |
|||||||
|
|
|
and guidelines |
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
that |
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
The right |
|
Using |
|
|
Implementing |
|
|
cal expertise with best available external clinical evidence |
|||||
|
|
|
workforce and |
outcome |
|
National Service |
|
|
from systematic research’ (Sackett et al. 1996). |
|||||||
|
|
|
using it right |
|
measures |
|
|
|
frameworks |
|
|
|
A hierarchy of evidence is often described or used in |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
the literature. This ranges from (1) systematic reviews, |
|||
|
|
Figure 1.1 Components of clinical governance. |
|
|
||||||||||||
|
|
|
|
in which evidence on a topic has been systematically |
||||||||||||
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926

Porter: Tidy's Physiotherapy, 14th Edition
Published
Unpublished
Research evidence
9
1
Knowledge
Patient
practice
Interaction
Clinical expertise
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Past experience, |
|
|
|
|
|
|
||
|
Preferences |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
beliefs and values |
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
ELSEVIER |
|
|
||||||
|
|
|
|
|
|
|
|
|
|||||||
Figure 1.2 What do we mean by ‘evidence’? (Adapted from Bury 1998, with permission.) |
|||||||||||||||
identified, appraised and summarised according to |
|
|
NOT |
||||||||||||
from clinical reasoning experience, discussed above. |
|||||||||||||||
predetermined criteria (usually limited to randomised |
Physiotherapists need to contribute to an ongoing |
||||||||||||||
controlled trials) |
said to be the strongest evidence |
debate to develop a hierarchy that reflects more appro- |
|||||||||||||
(the most reliable estimate of effectiveness) to (2) expert |
priately a |
||||||||||||||
opinion, perceived as the least reliable. An example is |
|
So |
|||||||||||||
Level |
Type of evidence |
CONTENTpopulation (e.g. people with multiple sclerosis with |
|||||||||||||
shown in Table 1.1. |
|
|
|
|
|
siotherapists? Core Standard 4 (CSP 2005a) states that: |
|||||||||
However, such a hierarchy fails to recognise that dif- |
‘In order to deliver effective care, information relating |
||||||||||||||
ferent research methods are needed to answer different |
to treatment options is identified, based on the best |
||||||||||||||
types of question and that, while a qualitative study |
available evidence.’ A range of sources of information |
||||||||||||||
may be the best research method for a particular ques- |
the physiotherapist may need to draw on, including |
||||||||||||||
|
PROPERTY |
|
|
|
get the best results from a literature search (his or |
||||||||||
tion, it still receives a low rating. The hierarchyOF also |
research evidence, patient organisations and clinical |
||||||||||||||
fails to recognise the importance of expertise derived |
guidelines, is listed. What practical steps need to be |
||||||||||||||
|
|
|
|
|
|
|
|
taken to identify and use research evidence? |
|||||||
Table 1.1 A hierarchy of evidence |
|
|
▪ Think |
about the clinical question you are trying |
|||||||||||
|
EvidenceSAMPLEobtained from |
|
to answer in your information search. Identify the |
||||||||||||
III |
|
symptoms of urinary incontinence), the intervention |
|||||||||||||
Ia |
Evidence obtained from a systematic review or |
|
|||||||||||||
|
you are looking for (e.g. neuromuscular electrical |
||||||||||||||
|
|
||||||||||||||
|
|
stimulation) and the outcome (e.g. a reduction in |
|||||||||||||
Ib |
Evidence obtained from at least one randomised |
|
|||||||||||||
|
symptoms), and use this information to formulate a |
||||||||||||||
|
controlled trial |
|
|
|
|||||||||||
|
|
|
|
search strategy. |
|||||||||||
IIa |
Evidence obtained from at least one |
|
|||||||||||||
▪ Work in partnership with an information scientist to |
|||||||||||||||
|
controlled study without randomisation |
||||||||||||||
|
|
|
|
|
|
|
|
||||||||
IIb |
Evidence obtained from at least one other type of |
|
her information skills and knowledge combined |
||||||||||||
|
|
||||||||||||||
|
|
with your clinical skills and knowledge). |
|||||||||||||
|
|
|
|
|
|
|
|
|
|||||||
|
experimental descriptive studies, such as |
▪ Look first for evidence that has already been synthe- |
|||||||||||||
|
|
sised |
systematic reviews, nationally developed |
||||||||||||
|
comparative studies, correlation studies and |
|
|||||||||||||
|
|
clinical guidelines or standards. This saves a lot of |
|||||||||||||
|
case studies |
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
effort |
searching for individual studies. If it is a |
|||||||
IV |
Evidence obtained from expert committee reports |
|
|||||||||||||
|
|||||||||||||||
|
or opinions and/or clinical experience of |
|
|||||||||||||
|
|
|
|
|
|
|
|
||||||||
respected authorities
reliable estimate of effectiveness.
▪ Know your databases well enough to know which will have the most relevant information on any particular topic.
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
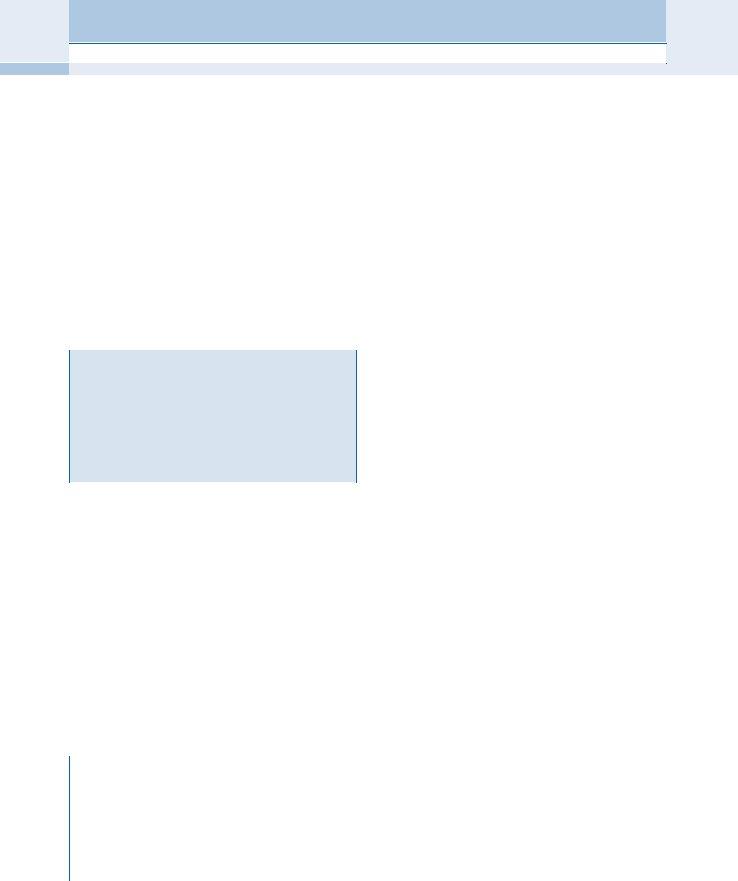
Porter: Tidy's Physiotherapy, 14th Edition
10THE RESPONSIBILITIES OF BEING A PHYSIOTHERAPIST
1 |
▪ Check the titles and abstracts for relevance. |
|
|
|
|
▪ Is the practitioner sufficiently skilled to apply the |
|||||||||||
▪ Critically |
appraise any relevant papers you |
have |
|
intervention safely and effectively? |
|
||||||||||||
|
|
found to assure yourself of their quality and of the |
▪ Is the practitioner an effective communicator? |
||||||||||||||
|
|
reliability of their conclusions. (A list of appraisal |
▪ Does the practitioner give the patient an opportunity |
||||||||||||||
|
|
instruments can be found at the end of this chapter.) |
|
to describe the symptoms fully, to explain the |
|||||||||||||
|
▪ When you find the ‘best available evidence’, think |
|
impact of the problem on daily life, and to ask |
||||||||||||||
|
|
about it in relation to your patient and your past |
|
questions? |
|
|
|
||||||||||
|
|
experience. Is it appropriate for that patient, will |
▪ Does the patient have enough information to be able |
||||||||||||||
|
|
you be able to quantify for the patient the degree |
|
to give informed consent? |
|
|
|||||||||||
|
|
of likely benefits and harms (if any)? |
|
|
|
|
|
▪ Are other options discussed that may have been |
|||||||||
|
▪ Discuss the evidence |
with the patient and |
agree |
|
more acceptable to the patient, even if less effective? |
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FINAL |
|
|
|
the preferred intervention(s) together. |
|
|
|
|
|
▪ Would treatment in a hospital setting mean a long, |
|||||||||
|
▪ Implement the preferred intervention(s). |
|
|
|
|
|
exhausting and expensive journey for the patient? |
||||||||||
|
▪ Evaluate the effect of the intervention(s) and act |
▪ Would the patient feel intimidated by a hospital |
|||||||||||||||
|
|
accordingly. |
|
|
|
|
|
|
|
|
|
environment? |
|
|
|||
|
|
|
|
|
|
|
|
|
ELSEVIER |
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
▪ Would treatment be more effective if it were |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
provided closer to home: for example, in the GP’s |
||||
|
@ |
|
|
|
|
|
|
|
|
|
|
surgery or health centre? |
|
|
|||
|
Weblink |
|
|
|
|
|
|
|
|
|
|
|
|
NOT |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
▪ Would treatment be more relevant if it were given in |
|||||
|
|
More information about |
|
|
|
|
a patient’s own home, to be able to develop a |
||||||||||
|
|
be found in Herbert et al. (2005) or at www. |
|
|
|
|
|
programme tailored to the person’s lifestyle and |
|||||||||
|
|
nettingtheevidence.org.uk/, a catalogue of useful |
|
|
|
|
|
environmental needs? |
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
||
|
|
electronic learning resources and links to organisations |
|
|
|
▪ Wherever treated, does the patient have adequate |
|||||||||||
|
|
that facilitate |
|
|
|
|
|
privacy, warmth and comfort? |
|
||||||||
|
|
fact that an intervention has been provedCONTENTto work in |
|
|
|
|
|||||||||||
|
|
‘Sources of Critical Appraisal Tools’ towards the end of |
|
|
|
▪ How long has the patient had to wait for treatment |
|||||||||||
|
|
this chapter. |
|
|
|
|
|
|
|
|
|
and will a delay alter the effectiveness of the |
|||||
|
|
|
|
|
|
|
OF |
|
|
|
|
interventions? |
|
|
|||
|
|
|
|
|
|
|
|
|
|
The answer to each of these questions can have an |
|||||||
|
|
from anPROPERTYintervention. |
|
|
|
impact on the patient’s ability to benefit from an inter- |
|||||||||||
|
|
CLINICAL EFFECTIVENESS |
|
|
|
|
|
vention, however effective the research evidence might |
|||||||||
|
|
Clinical effectiveness, as |
defined |
by |
the |
Department |
suggest an |
intervention is. This also |
illustrates the |
||||||||
|
|
complexity |
of the clinical reasoning |
process, where |
|||||||||||||
|
|
of Health, |
sounds very |
much |
like |
||||||||||||
|
|
highly skilled judgements have to be made based on a |
|||||||||||||||
|
|
practice |
doing things |
you know |
will |
be effective |
|||||||||||
|
|
consideration of the whole person, physically, emotion- |
|||||||||||||||
|
|
for a particular patient or group of patients. But the |
|||||||||||||||
|
|
ally and within society, as well as the environment, |
|||||||||||||||
|
|
|
SAMPLE |
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
practitioner skills and resources available, in order to |
|||||||||
|
|
research studies, in a relatively |
controlled environ- |
||||||||||||||
|
|
provide truly effective treatment. |
|
||||||||||||||
|
|
ment, does not necessarily mean that it will work for |
|
||||||||||||||
|
|
|
So while |
||||||||||||||
|
|
a particular |
patient. Both patients and |
practitioners |
|
||||||||||||
|
|
of clinical effectiveness, clinical effectiveness also takes |
|||||||||||||||
|
|
are unique beings, and there are many additional fac- |
|||||||||||||||
|
|
account of a range of other influences that could affect |
|||||||||||||||
|
|
tors, practical and behavioural, that need to be consid- |
|||||||||||||||
|
|
the patient’s ability to benefit from an intervention based |
|||||||||||||||
|
|
ered to ensure the patient gets the maximum benefit |
|||||||||||||||
|
|
on |
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
APPLYING NATIONAL STANDARDS AND |
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
GUIDELINES LOCALLY |
|
|
||
‘ |
|
|
|
|
|
|
|
|
|
|
|
||||||
|
Definition |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
Standards |
|
|
|
|
|||
|
|
Clinical effectiveness was defined by the Department of |
|
|
|
|
|
|
|||||||||
|
|
Health in 1996 as ‘the extent to which specific clinical |
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
One of the tenets of clinical governance is consistency |
|||||||||||
|
|
interventions, when deployed in the field for a particular |
|
|
|
||||||||||||
|
|
|
|
for the public, being confident that they will experience |
|||||||||||||
|
|
patient or population, do what they are intended to do — |
|
|
|
||||||||||||
|
|
|
|
the same quality of care and have access to the most |
|||||||||||||
|
|
that is, maintain and improve health and secure the |
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
effective interventions, regardless of where they live. |
||||||||||
|
|
greatest possible health gain from the available |
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
There should be no postcode lottery, where some treat- |
||||||||||
|
|
resources’ (NHS Executive 1996). |
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
ments might be available in some parts of the country |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
Applying national standards and guidelines locally 11
and not others; the quality of the average and worst ser- |
Clinical guidelines |
|
|
|
|
|
1 |
|||||||||
vices should be raised to that of the best. Where there are |
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
‘ |
|
|
|
|
|
|||||
Definition |
|
|
|
|
|
|
|
|||||||||
be used locally. Two examples are set out below. |
|
|
|
Clinical guidelines are ‘systematically developed |
|
|
||||||||||
Nationally developed standards |
|
|
|
|
|
statements to assist practitioner and patient decisions |
|
|
||||||||
|
|
|
|
|
about appropriate healthcare for specific circumstances’ |
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
||||||||
The CSP’s Standards of Physiotherapy Practice provides a |
|
(Field and Lohr 1992). |
|
|
|
|
|
|
||||||||
universal framework for the delivery of services |
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|||||||
throughout the UK, to which it is expected all phy- |
|
|
|
|
|
|
|
|
|
|
||||||
siotherapists will conform. So, for physiotherapy, |
|
|
The key factors in the development of clinical guide- |
|||||||||||||
patients can expect similar values and processes within |
lines are the systematic process for identifying and |
|||||||||||||||
a healthcare experience. |
|
|
|
|
||||||||||||
National Service Frameworks (NSFs) |
|
|
|
and transparent process used for the interpretation of |
||||||||||||
|
|
|
the evidence in the context of clinical practice, in order |
|||||||||||||
This government initiative aims to provide the NHS |
to formulate reliable recommendations for practice. |
|||||||||||||||
with explicit standards and principles for the pattern |
National Institute for Health and Clinical |
|||||||||||||||
and level of services required for a specific service or |
||||||||||||||||
Excellence (NIC ) |
|
FINAL |
||||||||||||||
care group. The NSFs aim to address the ‘whole system |
|
|||||||||||||||
|
|
|
|
|
||||||||||||
of care’ and each will set out where care is best |
|
|
|
|
|
|||||||||||
NICE is a Special Health Authority for England and |
||||||||||||||||
provided and the standard of care that patients should |
Wales, established by the government in 1999 to pro- |
|||||||||||||||
be offered in each setting. They provide ‘a clear set of |
vide health professionals and the public with authorita- |
|||||||||||||||
priorities against which local action can be framed’ |
tive information about the clinical effectiveness and |
|||||||||||||||
and seek to ensure that patients will get greater consis- |
||||||||||||||||
tency in the availability and quality of services, right |
|
|
|
NOT |
|
|
|
|
|
|||||||
grammes is to develop clinical guidelines, which are |
||||||||||||||||
across the NHS (Secretary of State for Health 1998). |
|
|
- |
|
|
|
|
|
|
|
||||||
carried out by a series of collaborating centres. The |
||||||||||||||||
Table 1.2 lists the NSFs that have been developed. |
Department of |
Health |
and the Assembly for Wales |
|||||||||||||
|
|
|
|
ELSEVIER |
|
|
|
|
|
|
||||||
They provide broad statements of expected services. |
have given NICE the remit for developing ‘robust and |
|||||||||||||||
For example, the NSF for older people states: ‘Older |
authoritative’ clinical guidelines, taking into account |
|||||||||||||||
people who |
have fallen receive |
effective treatment |
clinical effectiveness and cost effectiveness. More infor- |
|||||||||||||
and rehabilitation and, with their carers, receive advice |
mation about the key principles that underpin the way |
|||||||||||||||
|
|
|
OF |
|
|
NICE approaches clinical guideline development can |
||||||||||
on prevention through a specialised falls service.’ |
|
|
||||||||||||||
Physiotherapists will therefore need to address the |
be found on its website. |
|
|
|
|
|
||||||||||
implementation of this standard in any services they |
|
|
|
|
|
|
|
|
|
|
||||||
provide to older people. Implementation will also pro- |
|
|
|
|
|
|
|
|
|
|
||||||
@ |
Weblink |
|
|
|
|
|
|
|
||||||||
vide opportunities to promote the value of physiother- |
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
||||||||||
apy to this |
patient population |
and CONTENThighlight the |
|
|
|
|
|
|
|
|||||||
contribution |
physiotherapists can |
make to a trust’s |
|
National Institute for Health and Clinical Excellence (NICE): |
|
|
|
|||||||||
|
www.nice.org.uk. |
|
|
|
|
|
|
|||||||||
compliance with this particular standard. |
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
Scottish Intercollegiate Guidelines |
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|||||||
Table 1.2 National service frameworks developed by |
|
Network (SIGN) |
|
|
|
|
|
|
||||||||
the Department of Health |
|
|
|
|
SIGN was formed in 1993. Its objective is to improve |
|||||||||||
PROPERTY |
|
|
|
the quality of |
healthcare for patients in |
Scotland by |
||||||||||
▪ Coronary heart disease (including cardiac |
|
|
||||||||||||||
|
|
reducing variation in practice and outcome, through |
||||||||||||||
rehabilitation) |
|
|
|
|
||||||||||||
|
|
|
|
the development and dissemination of national clinical |
||||||||||||
▪ Cancer |
SAMPLE |
|
|
|
||||||||||||
|
|
|
guidelines containing |
recommendations |
for effective |
|||||||||||
|
|
|
|
|||||||||||||
▪ Paediatric intensive care |
|
|
|
|
||||||||||||
|
|
|
|
practice based on current evidence. Further information |
||||||||||||
▪ Mental health |
|
|
|
|
||||||||||||
|
|
|
|
can be found on its website. |
|
|
|
|
|
|||||||
▪ Older people (including falls, osteoporosis and stroke) |
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||
▪ Diabetes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
▪ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
@ |
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
▪ Renal |
|
|
|
|
|
Weblink |
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
▪ Children |
|
|
|
|
|
|
Scottish Intercollegiate Guidelines Network (SIGN): |
|
|
|
||||||
▪ Chronic obstructive pulmonary disease (2008) |
|
|
|
www.show.scot.nhs.uk/sign. |
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
12THE RESPONSIBILITIES OF BEING A PHYSIOTHERAPIST
1 |
|
Professionally led clinical guidelines |
|
|
|
|
|
an individual practitioner’s personal practice and/or |
|||||
The physiotherapy profession has developed national, |
the delivery of a whole service. Set out below are four |
||||||||||||
means |
by which physiotherapists can evaluate their |
||||||||||||
|
|
guidelines. To ensure |
|||||||||||
|
|
practice. They are not mutually exclusive. |
|||||||||||
|
|
quality and provide confidence for users, the CSP has |
|||||||||||
|
|
|
|
|
|
||||||||
|
|
established a process for the |
endorsement of |
these |
|
Evaluating the process of care (clinical audit) |
|||||||
|
|
clinical guidelines. The criteria for assessing whether |
|
||||||||||
|
|
|
|
|
|
||||||||
|
|
the quality of a guideline warrants CSP endorsement |
|
In order to evaluate the process of care, it is necessary to |
|||||||||
|
|
can be found in an appraisal questionnaire developed |
|
have a reliable benchmark with which to compare your |
|||||||||
|
|
by a European consortium, known as the AGREE instru- |
|
practice. Earlier, the importance of the local implemen- |
|||||||||
|
|
ment. For users of clinical guidelines, |
|
tation of nationally developed standards and evidence- |
|||||||||
|
|
clinical guidelines can be considered of high quality |
|
based clinical guidelines was discussed. These provide |
|||||||||
|
|
and should be implemented locally. Further informa- |
|
such a reliable benchmark. Clinical audit is a tool with |
|||||||||
|
|
tion about the process for the development of clinical |
|
which to measure your own performance (or more |
|||||||||
|
|
guidelines in physiotherapy is available from the CSP |
|
often, the performance of the service) against standards |
|||||||||
|
|
website. |
|
|
|
|
|
|
|
or criteria based on the ‘best available evidence’ of |
|||
|
@ Weblink |
|
|
|
|
|
|
|
effectiveness. This will enable you to identify the extent |
||||
|
|
|
|
|
|
|
|
to which you adhere to those standards or criteria, from |
|||||
|
|
AGREE Collaboration (Appraisal of Guidelines Research |
|
|
|
which recommendations can beFINALput in place to improve |
|||||||
|
|
|
|
|
adherence, if necessary. |
||||||||
|
|
and Evaluation): |
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
www.agreecollaboration.org. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
‘ |
|
|
||
|
|
Chartered Society of Physiotherapists (CSP): |
|
|
|
Definition |
|
||||||
|
|
www.csp.org.uk. |
|
|
|
|
|
|
|
Clinical audit is a cyclical process involving the |
|||
|
|
|
|
|
|
|
|
|
|
|
|
NOT |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
identification of a topic, setting standards, comparing |
|||
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
EVALUATING SERVICES |
|
|
|
|
|
|
|
practice with the standards, implementing changes, and |
|||
|
|
|
|
|
|
|
|
|
monitoring the effect of those changes (CSP 2005a). |
||||
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
ELSEVIER |
||||||
|
|
How do you know whether you are being effective? |
|
Further information about clinical audit can be found in |
|||||||||
|
|
Knowing whether you are or not is part of your profes- |
|
an information paper published by the CSP (2002d) and in |
|||||||||
|
|
sional responsibility as a physiotherapist. Rule 1 of |
|
Principles for Best Practice in Clinical Audit published by |
|||||||||
|
|
Rules of Professional Conduct (CSP 2002a) describes the |
|
NICE (2001). |
|
||||||||
|
|
|
|
|
OF |
|
|
|
|
|
|
||
|
|
responsibility a physiotherapist has to ensure that any |
|
|
|
|
|||||||
|
|
intervention offered to a patient is intended to be of |
|
|
|
|
|||||||
|
|
benefit. Several of the CSP’s standards of physiother- |
|
Evaluating the health outcomes of care |
|||||||||
|
|
apy practice include criteria that relate to evaluation, |
|
||||||||||
|
|
|
|
|
|
||||||||
|
|
|
This will determine the impact of the process of care on |
||||||||||
|
|
including: |
|
|
|
|
|
|
|
||||
|
|
|
|
|
CONTENTthe patient’s life by using specific measures before and |
||||||||
|
▪ As part of the assessment process, physiotherapists |
|
after treatment. The use of a test, scale or questionnaire |
||||||||||
|
|
consider and critically evaluate information |
about |
|
|||||||||
|
|
|
which |
records what it aims to record (is valid and |
|||||||||
|
|
effective interventions relating to the patient’s condi- |
|
||||||||||
|
|
|
responsive) and is sufficiently well described to ensure |
||||||||||
|
|
tion (Core Standard 4.1). |
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
that everyone who uses it does so in the same way (is |
||||
|
▪ A published, standardised, valid, reliable and respon- |
|
|||||||||||
|
|
reliable) will help to give physiotherapists the chance |
|||||||||||
|
|
sive outcome measure is used to evaluate the change |
|
||||||||||
|
|
|
to see whether the aims of their intervention have had |
||||||||||
|
|
in the patient’s health status (Core Standard 6). |
|
|
|
|
|||||||
|
|
|
|
|
|
the impact intended. |
|||||||
|
|
PROPERTY |
|
|
|
|
|
||||||
|
▪ All physiotherapists participate in |
a regular and |
|
A database of outcome measures can be found on |
|||||||||
|
|
systematic programme of |
clinical |
audit (Service |
|
||||||||
|
|
|
the CSP website. This will facilitate the selection of |
||||||||||
|
|
Standard 3.2)SAMPLE. |
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|||
the most appropriate measures for a specific patient or patient group. More information on using measures can be found in a CSP information paper (CSP 2001a).
As well as patients themselves having an interest in an objective assessment of their improvement, it is increasingly important for managers and team leaders to present such information to commissioners of health- care, to demonstrate the benefits of physiotherapy ser- vices and their value for money.
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
|
|
|
|
|
|
|
Continuing professional development |
13 |
||||||
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|||||||||
Using patient feedback |
|
|
behind the information recorded in the patient docu- |
|
|
|||||||||
|
|
|
1 |
|||||||||||
|
mentation can be explored. Guidance on peer review |
|
||||||||||||
Another mechanism for evaluating practice is to ask the |
||||||||||||||
can |
be found in the clinical audit |
tools document |
|
|||||||||||
patient for feedback. This could be through the use of a |
|
|
||||||||||||
contained in the Standards of Physiotherapy Practice pack |
|
|
||||||||||||
validated |
|
|
||||||||||||
(CSP 2005a). |
|
|
|
|
|
|
|
|||||||
information about the patient’s perception of health |
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|||||
gain, or through the use of a structured questionnaire |
CONTINUING PROFESSIONAL DEVELOPMENT |
|
|
|||||||||||
to determine the patient’s perception of the quality |
|
|
||||||||||||
of the treatment. The CSP’s Standards of Physiotherapy |
|
|
|
|
|
|
|
|
|
|
||||
Practice pack includes a |
|
|
|
|
|
|
|
|
|
|
||||
‘ |
|
|
|
|
|
|
|
|
||||||
Questionnaire, designed to measure criteria in the core |
Definition |
|
|
|
|
|
|
|
||||||
standards, for which only patients can judge compli- |
|
Continuing professional development (CPD) is the |
|
|
||||||||||
|
|
|
||||||||||||
ance. Patients are asked to respond to statements that |
|
|
|
|||||||||||
|
be seen as a systematic, ongoing structured process of |
|
|
|||||||||||
mirror the criteria (Table 1.3). |
|
|
|
|
|
|||||||||
|
|
|
maintaining, developing and enhancing skills, knowledge |
|
|
|||||||||
Responses from the feedback questionnaires can be |
|
|
|
|||||||||||
|
and competence both professionally and personally in |
|
|
|||||||||||
used by individuals or services to reflect on the extent |
|
|
|
|||||||||||
|
order to improve performance at work (CSP 2003). |
|
|
|||||||||||
to which the criteria are being met, and to introduce |
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|||||
new processes or development opportunities to secure |
|
|
|
|
|
|
FINAL |
|
|
|||||
greater conformance, if necessary. |
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
‘ |
|
|
|
|
|
|
|
|
||
Another valuable source of patient feedback is |
Definition |
|
|
|
|
|
|
|
||||||
patients’ complaints. These should be considered posi- |
|
|
|
|||||||||||
tively as opportunities to address the issues contained |
|
promulgates across all sectors of the population, in order |
|
|
||||||||||
within them, in order to introduce a service improve- |
|
to ensure the workforce is equipped to do the jobs that |
|
|
||||||||||
ment. Any issue that becomes a problem for a patient |
|
|
|
|
NOT |
|
|
|
|
|||||
|
|
|
|
|
will contribute to |
|
|
|||||||
is a problem for the service, which should be analysed. |
|
|
- |
|
|
|
|
|
|
|||||
|
|
|
|
|
promote prosperity in the UK. |
|
|
|
||||||
The involvement of the patient making the complaint |
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|||||
in this process, if willing, will facilitate the finding ofELSEVIERa |
|
|
|
|
|
|||||||||
solution that can then be embedded into systems and |
In healthcare, the connection between CPD/LLL and |
|
|
|||||||||||
the quality of services is at the centre of the govern- |
|
|
||||||||||||
processes. |
|
OF |
|
|
|
|||||||||
|
|
ment’s view of a new, modernised NHS. Physiothera- |
|
|
||||||||||
|
|
|
|
|
||||||||||
Peer review |
|
|
pists |
have always had |
a strong |
commitment to |
|
|
||||||
|
|
CPD evidenced by the clear statement in Rule 1 of |
|
|
||||||||||
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|||||||||
Peer review provides an opportunity to evaluate the |
|
|
||||||||||||
Rules of Professional Conduct: ‘Chartered physiothera- |
|
|
||||||||||||
clinical reasoning behind your |
pists shall only practise to the extent that they have. . . |
|
|
|||||||||||
trusted peer. It can be applied most effectively to the |
maintained. . . their ability to work safely and compe- |
|
|
|||||||||||
assessment, treatment planning and evaluative compo- |
tently.’ The Core Standards of Physiotherapy Practice, with |
|
|
|||||||||||
nents of physiotherapy practice, whereCONTENTthe reasoning which all physiotherapists should conform, include |
|
|
||||||||||||
Table 1.3 Extract from a patient feedback questionnaire |
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|||||||
Criteria |
|
|
Patient feedback questionnaire |
|
Response option |
|
|
|||||||
PROPERTY |
|
|
|
|
|
|
|
|
|
|
|
|
||
Core Standard 5.3 |
|
By the end of your first visit, were |
|
Yes, no, don’t know |
|
|
||||||||
The findings of the clinical assessment are explained to |
|
the results of the assessment |
|
|
|
|
|
|||||||
the patient |
|
|
explained? |
|
|
|
|
|
|
|
||||
|
SAMPLE |
|
I felt involved in deciding about my |
|
Strongly disagree, disagree, |
|
|
|||||||
Core Standard 8.1 |
|
|
|
|
||||||||||
Physiotherapists ensure that the patient is fully |
|
treatment plan |
|
|
|
uncertain, agree, strongly |
|
|
||||||
involved in any |
|
|
|
|
|
|
|
agree |
|
|
|
|||
treatment planning |
|
|
|
|
|
|
|
|
|
|
|
|
||
Core Standard 12.3 |
|
The physiotherapists used words |
|
Strongly disagree, disagree, |
|
|
||||||||
All communication, written and verbal, is clear, |
|
I didn’t understand |
|
|
|
uncertain, agree, strongly |
|
|
||||||
unambiguous and easily understood by the recipient |
|
|
|
|
|
|
|
agree |
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(Adapted from CSP 2000.)
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
14THE RESPONSIBILITIES OF BEING A PHYSIOTHERAPIST
1 |
standards for the assessment, planning, implementation |
skills such as |
and evaluation of a CPD programme. Service Standards |
critical analysis. |
|
|
6 and 7 require that all physiotherapy services should |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
‘ |
|
|
|
|
|
have a programme of |
Definition |
|
|
|
|
||||||||||
|
The requirement for |
|
Reflective practice is the process of reviewing an episode |
||||||||||||
pists and other healthcare professionals, discussed ear- |
|
of practice to describe, analyse, evaluate and inform |
|
||||||||||||
lier, makes CPD an essential component of professional |
|
professional learning; in such a way, new learning |
|
|
|||||||||||
life. A philosophy of LLL and individual responsibility |
|
modifies previous perceptions, assumptions and |
|
|
|||||||||||
for this will be introduced in qualifying programmes, |
|
understanding, and the application of this learning to |
|
||||||||||||
equipping students for a lifetime of learning in order |
|
practice influences treatment approaches and outcomes |
|||||||||||||
to maintain and continually improve their competence |
|
(CSP 2002b). |
|
|
|
|
|||||||||
to practise. Written evidence of learning and develop- |
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
||||||||||
ment, and its impact on improving practice, is now an |
|
|
|
|
|
|
|||||||||
essential requirement. Every physiotherapist must |
|
|
|
|
|
|
|||||||||
establish a portfolio containing such evidence, which |
|
HAVING THE RIGHT WORKFORCE (AND USING |
|||||||||||||
will need to be maintained throughout a career. Guid- |
|
IT APPROPRIATELY) |
|
|
|
||||||||||
ance |
on this can |
be |
found |
in |
Developing |
a Portfolio: |
|
|
|
|
|
|
|||
|
Physiotherapists have a professional responsibility |
||||||||||||||
a Guide for CSP Members (CSP 2001b). |
|
|
|
|
|||||||||||
|
|
|
|
to use their skills appropriately.FINALThis reflects Rule 1 |
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
of Rules of Professional Conduct, which states that phy- |
||||
|
Some key characteristics of continuing professional |
|
|||||||||||||
|
|
|
siotherapists should ‘only practise to the extent that |
||||||||||||
|
development (CSP 2003) |
|
|
|
|
|
|
they have established, maintained and developed their |
|||||||
|
▪ It should comprise a broad range of learning |
|
|
|
ability to work safely and competently’. But there is |
||||||||||
|
|
|
|
also a professional responsibility to use resources |
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
NOT |
|
|
|
|
|
activities (courses, |
|
|
|
(human as |
|||||||||
|
|
supervision, research, audit, reflections on |
|
|
|
|
healthcare. This means giving consideration |
as |
to |
||||||
|
|
experience, peer review — this is not an exhaustive |
|
|
|||||||||||
|
|
|
|
whether you need to refer a patient on, either because |
|||||||||||
|
|
list). |
|
|
|
|
|
|
ELSEVIER |
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
he or she requires a higher level of skill than you |
|||||
|
▪ It is based on individual responsibility, trust and self- |
|
|
||||||||||||
|
|
|
possess, or needs a specialist in a different clinical area. |
||||||||||||
|
|
evaluation. |
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
qually, consideration should be given as to whether |
|||||
|
|
It links learning with enhancement of quality of |
|
|
|
||||||||||
|
▪ |
|
|
|
there are elements of the treatment programme that |
||||||||||
|
|
|
|
|
|
OF |
|
|
|
||||||
|
|
patient care and professional excellence whilst |
|
|
|
can be delegated to a physiotherapy assistant or other |
|||||||||
|
|
ensuring public safety. |
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
support worker. (The word ‘assistant’ is used in the |
|||||||
|
▪ It should recognise the outcomes of CPD with a |
|
|
|
|||||||||||
|
|
|
|
following section to mean both of these.) |
|
|
|||||||||
|
|
focus on achievement. |
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
The decision about whether to delegate, and which |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
tasks or activities to delegate, is entirely the responsi- |
||||
|
|
|
|
|
|
CONTENT |
|
|
|
|
|||||
|
The emphasis |
on |
the importance of |
CPD/LLL |
|
bility of the physiotherapist making that decision. The |
|||||||||
|
|
physiotherapist |
also takes |
full responsibility |
for |
the |
|||||||||
within clinical governance is a welcome development. |
|
||||||||||||||
|
application of |
the tasks or |
activities carried |
out |
by |
||||||||||
The challenges for physiotherapists in keeping up to |
|
||||||||||||||
|
the person who has been delegated. So choosing tasks |
||||||||||||||
date are huge, with the fast pace of change in health- |
|
||||||||||||||
|
to be undertaken by an assistant is a complex element |
||||||||||||||
care |
in particular the rapid increase in the volume |
|
|||||||||||||
|
of professional activity, which depends on an informed |
||||||||||||||
of information |
that |
has |
to |
be evaluated and |
|
||||||||||
|
professional opinion. |
|
|
|
|||||||||||
incorporatedPROPERTYinto practice. It is hoped that protected |
|
|
|
|
|||||||||||
|
|
|
|
|
|
||||||||||
|
|
SAMPLE |
|
|
|
|
|
|
|
|
|
||||
time for CPD, including time in the workplace, will become a reality in the NHS, as recommended by the Kennedy Report (Bristol Royal Infirmary Inquiry 2001) and the CSP (2003).
Another form of professional development is reflec- tive practice, a process in which practitioners think crit- ically about their practice and as a result may modify their action or behaviour. ‘Reflection enables learning at a
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
|
|
|
|
|
|
|
|
|
|
|
|
The future |
15 |
||
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|||||||||
|
condition and progress with the plan, and advising |
|
The Healthcare Commission is an independent stat- |
|
|
||||||||||
|
|
|
1 |
||||||||||||
|
the physiotherapist of any variations in either of |
utory body established to raise standards throughout |
|
||||||||||||
|
these. As there are no hard and fast rules about what |
England and |
Wales. In Scotland a similar function |
|
|
||||||||||
|
to delegate, the physiotherapist should consider |
is provided by NHS Quality Improvement Scotland, |
|
|
|||||||||||
|
carefully the scope and nature of the task and ensure |
the Health and Personal Social Services Regulation |
|
|
|||||||||||
|
that these are clearly defined and communicated to |
and Improvement Authority (HPSSRIA) undertakes |
|
|
|||||||||||
|
the assistant. |
|
|
|
regular reviews of the quality of services in Northern |
|
|
||||||||
▪ Who to delegate to? The factors to be considered here |
Ireland. The Healthcare Commission is tasked with |
|
|
||||||||||||
|
are the competence of the assistant and the nature of |
assessing the implementation of clinical governance |
|
|
|||||||||||
|
the task. The competence of the assistant will be |
in every NHS trust and making its findings public. |
|
|
|||||||||||
|
affected by the person’s length of service, prior expe- |
Teams of trained reviewers visit trusts every 3 5 years |
|
|
|||||||||||
|
rience and training received, coupled with judge- |
(and can be called in at any time should concerns be |
|
|
|||||||||||
|
ments by the physiotherapist about the assistant’s |
raised) to review trust information and data, talk to |
|
|
|||||||||||
|
ability to deal with that particular patient in those |
staff and patients, and consider the trust’s performance |
|
|
|||||||||||
|
particular circumstances. |
|
|
|
in specified categories. The Healthcare Commission has |
|
|
||||||||
|
The decision about what to delegate and who to del- |
added to its existing responsibilities those for inspect- |
|
|
|||||||||||
|
ing hospitals and care homes in the private sector and |
|
|
||||||||||||
egate to is one that, while ultimately the responsibility |
|
|
|||||||||||||
carrying out |
|
|
|||||||||||||
of the physiotherapist, also requires the active involve- |
|
|
|||||||||||||
|
|
|
|
|
FINAL |
|
|
||||||||
ment of the person to whom the task is being delegated. |
management within the NHS. |
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|||||||
The assistant, therefore, must be allowed to make an |
|
xamples of a physiotherapy manager’s |
|
|
|
||||||||||
|
|
|
|
||||||||||||
assessment of his or her own competence in relation to |
|
|
|
|
|||||||||||
|
responsibilities within a clinical governance |
|
|
|
|||||||||||
the particular task. The task should not be delegated if |
|
|
|
|
|||||||||||
|
programme |
|
NOT |
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
either the physiotherapist or the assistant is concerned |
|
|
- |
|
|
|
|
||||||||
|
|
|
|
|
|
|
|||||||||
about the assistant’s competence. The physiotherapist |
|
|
|
|
|
|
|
||||||||
will then need to decide whether training is required. |
|
▪ Check staff are currently on the state register. |
|
|
|
||||||||||
|
▪ Deal with and learn from complaints. |
|
|
|
|||||||||||
|
Newly qualified physiotherapists should recognise |
|
|
|
|
||||||||||
|
|
|
|
|
ELSEVIER |
|
|
|
|
||||||
and value the skills and knowledge many assistants |
|
▪ Carry out programmes for quality improvement, |
|
|
|
||||||||||
|
including clinical audit and evaluation, and report |
|
|
|
|||||||||||
possess, |
particularly those who have |
long service |
|
|
|
|
|||||||||
|
how these have led to improvements for patients. |
|
|
|
|||||||||||
within the profession, so that effective |
partnerships |
|
|
|
|
||||||||||
|
▪ Ensure that nationally produced, |
|
|
|
|||||||||||
between physiotherapists and assistants canOFcontribute |
|
|
|
|
|||||||||||
|
standards and clinical guidelines are implemented |
|
|
|
|||||||||||
to the efficient and effective delivery of physiotherapy |
|
|
|
|
|||||||||||
|
locally. |
|
|
|
|
|
|
||||||||
services. Physiotherapy assistant members of the CSP |
|
|
|
|
|
|
|
||||||||
|
▪ Have an appropriate skill mix and staffing level to |
|
|
|
|||||||||||
have a Code of Conduct (CSP 2002c) to which they are |
|
|
|
|
|||||||||||
|
ensure the safety of patients, making appropriate use |
|
|
|
|||||||||||
expected to adhere in the same way physiotherapists |
|
|
|
|
|||||||||||
|
of human and financial resources, in order to provide |
|
|
|
|||||||||||
are to the Rules. Users of physiotherapy services have |
|
|
|
|
|||||||||||
|
effective care. |
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
CONTENT |
|
|
|
|
|
|
|
||||
a right to expect those who deliver them to be compe- |
|
▪ Have a process for identifying and supporting staff |
|
|
|
||||||||||
tent to |
do so. The physiotherapist has |
the ultimate |
|
|
|
|
|||||||||
|
members whose competence is in question. |
|
|
|
|||||||||||
responsibility to the patient for ensuring this is the case, |
|
|
|
|
|||||||||||
|
▪ Provide an |
|
|
|
|||||||||||
but also needs to consider competence in the context of |
|
|
|
|
|||||||||||
|
for individual CPD activities. |
|
|
|
|||||||||||
effective |
resource use, in terms of both |
finance and |
|
|
|
|
|||||||||
|
▪ Ensure appropriate participation in multiprofessional |
|
|
|
|||||||||||
skills. |
PROPERTY |
|
|
|
|
|
|
|
|||||||
|
|
|
|
clinical audit and quality improvement activities. |
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
MONITORING CLINICAL GOVERNANCE |
|
So, being a competent physiotherapist who displays |
|
|
|||||||||||
|
|
|
SAMPLE |
|
|
|
the essential |
characteristics of a professional in the |
|
|
|||||
NHS physiotherapy managers are responsible for devis- |
|
|
|||||||||||||
current climate is a complex and demanding process. |
|
|
|||||||||||||
ing, implementing and reporting on a |
departmental |
|
|
||||||||||||
Figure 1.3 attempts to summarise the elements of pro- |
|
|
|||||||||||||
clinical governance programme, which should reflect |
|
|
|||||||||||||
fessionalism described in this chapter. |
|
|
|||||||||||||
all the aspects of clinical governance discussed in this |
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|||||||
chapter. Physiotherapists should play an active part |
|
|
|
|
|
|
|
|
|
||||||
in contributing to physiotherapy clinical governance |
THE FUTURE |
|
|
|
|
|
|
||||||||
programmes and also participate in relevant multi- |
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|||||||
professional clinical governance activities such as clini- |
The health service continues to be a high priority for the |
|
|
||||||||||||
cal audit or local protocol/clinical pathway design. |
government. Change is constant and a key challenge for |
|
|
||||||||||||
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
16THE RESPONSIBILITIES OF BEING A PHYSIOTHERAPIST
1 |
|
|
|
|
||||||
|
|
reasoning and professional judgement, ongoing reflection, |
|
|||||||
|
|
|
and critical application of the evidence base |
|
|
|
||||
|
|
|
|
|
|
|
||||
|
|
|
Professional responsibility, manifested in |
|
|
|
|
|
|
|
|
|
|
adherence to a professional code of |
|
|
|
|
|
|
|
|
|
conduct/standards of practice, undertaking |
|
|
Professional privilege, expressed through |
|||||
|
|
structured, evaluated CPD to meet identified |
|
|
professional autonomy and |
|||||
|
|
learning needs, and engagement with the full |
|
|
|
|
|
|
||
|
|
|
implications of clinical effectiveness |
|
|
|
|
|
|
|
|
|
Figure 1.3 Elements of professionalism. (With thanks to Dr Sally Gosling.) |
|
|
|
|||||
|
|
physiotherapists is to respond to the opportunities and |
community settings. The success of domiciliary and |
|||||||
|
|
risks presented to ensure that |
||||||||
|
|
delivered to patients. Many of the government’s priority |
hospital admissions and allowing speedier discharges |
|||||||
|
|
health programmes will be dependent for their success |
will be further reinforced through the introduction of |
|||||||
|
|
on the provision of effective rehabilitation in order to |
intermediate care. The musculoskeletal physiotherapy |
|||||||
|
|
ensure people can continue to lead independent lives, |
services delivered in GP practices and health centres, |
|||||||
|
|
including services for older people, children and those |
|
|
|
FINAL |
||||
|
|
where trust is already established between doctors |
||||||||
|
|
with |
and physiotherapists, has facilitated more direct access |
|||||||
|
|
a key contribution to make to keeping people fit for |
to patients and better referrals, making services more |
|||||||
|
|
work through, for example, the effective management |
efficient as well as effective. |
|
||||||
|
|
of musculoskeletal problems or the delivery of cardiac |
The challenges, however, will lie with greater team |
|||||||
|
|
rehabilitation |
programmes. Ensuring |
ergonomically |
|
NOT |
|
|||
|
|
working and delegation of tasks, with physiotherapists |
||||||||
|
|
safe environments in the workplace and offering a rapid |
- |
|
|
|
||||
|
|
having to be prepared to be more flexible, often taking |
||||||||
|
|
on teaching roles in order to allow other staff such as |
||||||||
|
|
other examples of the value of the profession. |
ELSEVIER |
|
||||||
|
|
|
|
rehabilitation assistants to deliver services. There will |
||||||
|
|
|
|
|
|
|
be a need to take on some |
|||
|
|
Structural changes |
|
|
|
such as key worker or case manager, in order to deliver |
||||
|
|
|
|
|
a more consistent approach to care to vulnerable people |
|||||
|
|
|
|
|
|
|
||||
|
|
|
|
OF |
|
|
||||
|
|
|
|
|
|
living in the community. |
|
|||
|
|
Continued investment in healthcare will bring with it an |
|
|||||||
|
|
increase in the expectations of the public whose money |
Another challenge will be the experience of working |
|||||||
|
|
is being used, and challenges from the government |
in more isolated settings, with less easy access to peer |
|||||||
|
|
and the public about the need to change and modernise |
support, supervision or shared CPD with colleagues. |
|||||||
|
|
the way in which healthcare is delivered. Services will |
At a time when clinical governance, the requirement |
|||||||
|
|
need to be more responsive to patients’ needs,CONTENTprovided for |
||||||||
|
|
in settings closer to patients’ own environments, and |
patients of practitioners’ competence and safety are to |
|||||||
|
|
delivered more speedily to maximise health benefits |
the fore, physiotherapists will need to work hard to cre- |
|||||||
|
|
and utilise available resources more effectively. |
|
|
ate systems to support their ongoing learning, while |
|||||
|
|
Many more physiotherapy services will be provided |
also ensuring their managers accept their responsibil- |
|||||||
|
|
in primary care and community settings. Primary Care |
ities too. Networking with colleagues with similar |
|||||||
|
|
Trusts ( CTs) will hold 60 per cent of the total budget |
interests and case mix at a local and national level will |
|||||||
|
|
PROPERTY |
|
|
|
become more important. Where |
||||
|
|
for healthcare in their local area, and local people will |
||||||||
|
|
have a much stronger voice in the |
not possible, the use of electronic networks for commu- |
|||||||
|
|
cess about how those funds are used. In addition, the |
nication and accessing learning resources will need to |
|||||||
|
|
|
SAMPLE |
|
|
|
be embraced. |
|
|
|
|
|
government has committed itself to increasing integra- |
|
|
|
|||||
|
|
tion between |
health and social care, |
through Care |
Delivering clinically effective and |
|||||
|
|
Trusts, where budgets are pooled in order that they |
||||||||
|
|
services |
|
|
|
|||||
|
|
can be used more flexibly to meet the needs of the local |
|
|
|
|||||
|
|
|
|
|
|
|||||
|
|
population. |
|
|
|
|
The profession can thrive only if it can clearly demon- |
|||
|
|
More services delivered in primary care and |
|
|
strate the ‘added |
value’ it offers to patients through |
||||
|
|
|
|
increasing their independence, shorter hospital stays, |
||||||
|
community settings |
|
|
|
||||||
|
|
|
|
fewer work days lost and so on. In order to achieve |
||||||
|
|
|
|
|
|
|
||||
|
|
Physiotherapy already has a track record of delivering |
this, the profession needs a |
|||||||
|
|
responsive and effective services in primary care and |
First, it needs to |
increase its knowledge base about |
||||||
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
|
|
|
|
|
|
|
|
|
Sources of critical appraisal tools |
17 |
||
|
|
|
|
|||||||||
|
|
|
|
|||||||||
the effectiveness of specific interventions, through |
will continue to be highly complex, |
|
|
|||||||||
|
1 |
|||||||||||
research. Second, it needs to use information from the |
|
|||||||||||
evaluation of practice to demonstrate the benefit to |
with equipping physiotherapy students ‘with the atti- |
|
|
|||||||||
patients of those interventions. The profession urgently |
tude, aptitude and capacity to cope with change, uncer- |
|
|
|||||||||
requires |
tainty and unpredictability and with a commitment to |
|
|
|||||||||
and other funding in order to increase the knowledge |
the concept of quality improvement’ (CSP 2002b). Quali- |
|
|
|||||||||
base of the profession. Challenges from commissioners |
fying physiotherapists of today will therefore be better |
|
|
|||||||||
of services, to provide evidence of the effectiveness of |
equipped than ever to cope. The NHS is increasingly |
|
|
|||||||||
physiotherapy for particular patient or diagnostic |
looking for leaders who are innovative, clear, lateral |
|
|
|||||||||
groups, will not go away and physiotherapy services |
thinkers and |
|
|
|||||||||
are in increasing jeopardy without it. |
|
|
|
placed to adopt such roles and should be proactive in |
|
|
||||||
The profession must be brave enough to look critically |
looking for opportunities to do so. The skill is to turn |
|
|
|||||||||
at the outcomes of interventions. Where research evi- |
challenges and pressures into opportunities to demon- |
|
|
|||||||||
denceshows that particular interventions are ineffective, |
strate the ‘added value’ of physiotherapy, which in turn |
|
|
|||||||||
these should cease to be provided. Where patient out- |
will provide job satisfaction, recognition and benefit for |
|
|
|||||||||
comes are used as a determinant and demonstrate little |
patients and the profession. |
FINAL |
|
|
||||||||
or no effect, consideration should be given to possible |
|
|
|
|
|
|
|
|||||
alternative strategies for securing benefit to those |
|
|
|
|
|
|
|
|||||
patients which may lie outside physiotherapy. For phy- |
|
|
|
|
|
|
|
|||||
SOURCES OF CRITICAL APPRAISAL TOOLS |
|
|
||||||||||
siotherapists to continue to provide services in areas |
|
|
|
|
|
|
|
|
||||
where there is little benefit weakens the image of the pro- |
Critical Appraisal Skills Programme |
|
|
|||||||||
fession to the public and to colleagues from other |
|
|
||||||||||
|
|
|
|
|
|
|
|
|||||
professions. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
@ |
|
|
NOT |
|
|
|
||
|
|
|
|
|
Weblink |
|
|
|
||||
There is a growing emphasis in the NHS on working |
|
|
|
- |
|
|
|
|||||
|
|
|
|
|
|
|
||||||
smarter, looking at systems |
of care |
from a patient’s |
|
|
|
|
|
|
|
|||
|
Qualitative research: |
|
|
|
||||||||
perspective, breaking down |
what are perceived as |
|
www.phru.org.uk/casp/resources/qualitative.pdf |
|
|
|||||||
|
|
|
ELSEVIER |
|
|
|
||||||
tribal boundaries between professions, and redesigning |
|
Randomised controlled trials: |
|
|
|
|||||||
|
www.phru.org.uk/casp/resources/rct.pdf |
|
|
|||||||||
things that way because we always have’. Physiothera- |
|
Systematic review: |
|
|
|
|||||||
pists will need to embrace new ways of working with- |
|
www.phru.org.uk/casp/resources/reviews.pdf |
|
|
||||||||
|
|
OF |
|
|
|
|
|
|
|
|
|
|
out feeling defensive or appearing to be protectionist. |
|
|
|
|
|
|
|
|
||||
Opportunities will emerge from redesign for physio- |
Scottish Intercollegiate Guidelines Network |
|
|
|||||||||
therapists to adopt new and highly skilled roles in just |
@ Weblink |
|
|
|
|
|||||||
the same way as the successful creation of extended- |
|
|
|
|
||||||||
scope practitioner and physiotherapy consultant roles. |
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
||||
Influencing the agenda |
|
CONTENT |
|
|
|
|
|
|||||
|
|
|
|
|
www.sign.ac.uk/guidelines |
|
|
|
||||
To make any of this work, physiotherapists need to be |
|
Cohort study: |
|
|
|
|
||||||
|
www.sign.ac.uk/guidelines |
|
|
|
||||||||
confident about their roles and able |
to articulate to |
|
|
|
|
|||||||
|
Diagnostic study: |
|
|
|
||||||||
others the value of physiotherapeutic interventions or |
|
|
|
|
||||||||
|
www.sign.ac.uk/guidelines |
|
|
|
||||||||
approaches from a |
|
|
|
|
||||||||
|
Randomised controlled trial: |
|
|
|
||||||||
point of view. Physiotherapists must adopt a political |
|
|
|
|
||||||||
|
www.sign.ac.uk/guidelines |
|
|
|
||||||||
astutenessPROPERTYthat makes them aware of the wider national |
|
|
|
|
||||||||
|
Systematic review: |
|
|
|
||||||||
and local drivers for change in order that opportunities |
|
|
|
|
||||||||
|
www.sign.ac.uk/guidelines |
|
|
|
||||||||
for the profession and for services can be identified and |
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|||||
SAMPLE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
seized positively. They need to be seen to be engaged |
Users’ guide series |
|
|
|
||||||||
with and responsive to current agendas through con- |
|
|
|
|||||||||
Guyatt GH, Sackett DL, Cook DJ 1993 Users’ guides to the |
|
|
||||||||||
tacts with patient and public representatives as well |
|
|
||||||||||
|
|
medical literature. II: How to use an article about therapy |
|
|
||||||||
as senior managers and local politicians. |
|
|
|
|
|
|
||||||
|
|
|
|
or prevention, pt A. JAMA 270(21): 2598 2601 |
|
|
||||||
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
Guyatt GH, Sackett DL, Cook DJ 1994 Users’ guides to the |
|
|
|||||
Characteristics of the profession required to |
|
|
medical literature. II. How to use an article about therapy |
|
|
|||||||
maximise the opportunities being presented |
|
|
|
|
or prevention, pt B. JAMA 271(1): 59 63 |
|
|
|||||
|
|
|
|
|
Oxman AD, Cook DJ, Guyatt GH 1994 Users’ guides to the |
|
|
|||||
One thing is certain. The delivery of healthcare within |
|
|
||||||||||
|
|
medical literature. VI: How to use an overview. JAMA |
|
|
||||||||
organisations, whether funded by the state or privately, |
|
|
272(17): 1367 1371 |
|
|
|
||||||
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
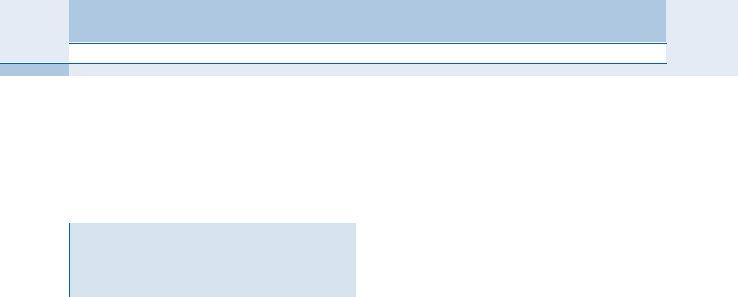
Porter: Tidy's Physiotherapy, 14th Edition
18THE RESPONSIBILITIES OF BEING A PHYSIOTHERAPIST
1 |
|
Books |
|
|
Dawes M, Summerskill W, Glasziou P et al. 2005 Sicily |
|||
|
Bury T, Mead J (eds) 1998 Evidence Based Healthcare: |
statement on evidence based practice. MBC Med Educ |
||||||
|
|
a Practical Guide for Therapists. Butterworth |
5: 1 |
|
|
|
||
|
|
|
|
|
||||
|
|
Heinemann: Oxford |
|
|
DHSS (Department of Health and Social Security) 1973 |
|||
|
|
Greenhalgh T 2000 How to Read a Paper: the Basics of |
McMillan Report: The Remedial Professions (report by a |
|||||
|
|
Evidence Based Medicine. BMJ Books: London |
working party set up in March 1973 by the Secretary of |
|||||
|
|
|
|
|
State for Social Services). HMSO: London |
|||
|
|
Clinical Guidelines |
|
|
DHSS 1977 Health Services Development: Relationship |
|||
|
|
|
|
between the Medical and Remedial Professions [HC(77) |
||||
|
|
|
|
|
||||
|
|
|
|
|
33]. DHSS: London |
|||
|
@ Weblink |
|
|
|||||
|
|
|
Department of Health 1991 Research for Health: an R&D |
|||||
|
|
Appraisal of Guidelines for Research and Evaluation |
|
Strategy for the NHS. DoH: London |
||||
|
|
|
Department of Health 2002 Health Professions Order |
|||||
|
|
(AGREE) instrument: |
|
|
||||
|
|
|
|
Statutory Instrument 2002 No. 254. HMSO: ondon |
||||
|
|
www.agreecollaboration.org |
|
|
||||
|
|
|
|
Department of Health 2004 The Shipman Inquiry: Fifth |
||||
|
|
|
|
|
||||
|
|
|
|
|
Report |
|
Safeguarding Patients: Lessons from the Past, |
|
|
|
Barclay J 1994 In Good Hands. Butterworth Heinemann: ELSEVIER |
||||||
|
|
ACKNOWLEDGEMENTS |
|
|
Proposals for the Future. HMSO: London. Website: |
|||
|
|
|
|
|
www.the shipman inquiry.org.uk/home.asp; accessed |
|||
|
|
With thanks to Judy Mead who created the original chapter |
4 December 2006 |
|||||
|
|
|
|
|
|
|
|
NOT |
|
|
in the 13th edition. We are also grateful to a number of col |
Ersser SJ, Atkins S 2000 Clinical reasoningFINALand patient |
|||||
|
|
leagues who commented on an earlier draft of this chapter |
centred care. In: Higgs J, and Jones M (eds) Clinical |
|||||
|
|
and whose thoughts have improved its content, in particular |
Reasoning in the Health Professions. Butterworth |
|||||
|
|
Sarah Fellows and Sally Gosling. |
|
|
Heinemann: Oxford |
|||
|
|
|
|
Field MJ, |
Lohr KN (eds) 1992 Guidelines for Clinical |
|||
|
|
|
|
|
||||
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
Practice: From Development to Use. National Academy |
|||
|
|
|
|
|
Press: Washington, DC |
|||
|
|
|
CONTENT |
|
|
|||
|
|
REFERENCES |
|
|
Herbert R, Mead J, Jamtvedt G, Birger Hagen K 2005 |
|||
|
|
|
|
|
Practical Evidence based Physiotherapy. Butterworth |
|||
|
|
|
|
|
Heinemann: Oxford |
|||
|
|
Oxford |
|
|
Higgs J, Jones M (eds) 2000 Clinical Reasoning in the Health |
|||
|
|
Bristol Royal Infirmary Inquiry 2001 The Report of the Public |
Professions, 2nd edn. Butterworth Heinemann: Oxford |
|||||
|
|
Inquiry into Children’s Heart Surgery at the Bristol Royal |
Higgs J, Titchen A 2001 Rethinking the practice |
|||||
|
|
ProgrammesPROPERTYin Physiotherapy. CSP: London |
physiotherapy. In: Higgs J, Jones M (eds). Clinical |
|||||
|
|
Infirmary 1984 1995. Stationery Office: LondonOF |
knowledge interface in an uncertain world: a model |
|||||
|
|
Bury T 1998 Evidence based healthcare explained. In: Bury |
for practice development. Br J Occup Ther 64(11): |
|||||
|
|
T, Mead J (eds) Evidence Based Healthcare a Practical |
526 533 |
|
|
|||
|
|
Guide for Therapists. Butterworth Heinemann: xford |
HPC (Health Professions Council) 2002 The Health |
|||||
|
|
Cott CA, Finch E, Gasner D et al. 1995 The movement |
Professions Order 2001: Stationery Office: London; www. |
|||||
|
|
continuum theory of physical therapy. Physiother Can |
hpc uk.org/publications/ruleslegislation/index.asp? |
|||||
|
47(2): 87 95 |
|
|
id=89 |
|
|
|
|
|
|
CSP (Chartered Society of hysiotherapy) 2000 Clinical |
HPC 2003 Standards of conduct performance and ethics. |
|||||
|
|
Audit Tools. CSP: London |
|
|
HPC: London |
|
||
|
|
CSP 2001a Outcome Measures. CSP: ondon |
HPC 2005 What Happens if a Complaint is Made about me?. |
|||||
|
|
CSP 2001b Developing a Portfolio: a Guide for CSP |
HPC: London |
|
||||
|
|
Members. CSP: London |
|
|
HPC 2006 About Us; www.hpc uk.org/, accessed 1 |
|||
|
|
CSP 2002a Rules of Professional Conduct. CSP: London |
December 2006 |
|||||
|
|
CSP 2002b Curriculum Framework for Qualifying |
Jones M, Jensen G, Edwards I 2000 Clinical reasoning in |
|||||
|
|
CSP 2002c Physiotherapy Assistants Code of Conduct. CSP: |
Reasoning in the Health Professions. Butterworth |
|||||
|
|
London |
|
|
Heinemann: Oxford |
|||
|
|
CSP 2002d ClinicalSAMPLEAudit. CSP: London |
|
|
Koehn D 1994 The Ground of Professional Ethics. Routledge: |
|||
|
|
CSP 2003 Policy statement on Continuing Professional |
London |
|
|
|||
|
|
Development (CPD). CSP: London |
|
|
NHS Executive 1996 Promoting Clinical Effectiveness. |
|||
|
|
CSP 2005a Standards of Physiotherapy Practice. CSP: London |
Department of Health: London |
|||||
|
|
CSP 2005b Demonstrating Professionalism through CPD. |
NICE (National Institute for Health and Clinical Excellence) |
|||||
|
|
CSP: London |
|
|
2001 The Guideline Development Process Information |
|||
|
|
CSP 2006 website. http://tinyurl.com/ydbr7d; accessed 18 |
for National Collaborating Centres and Guideline |
|||||
|
|
October 2006 |
|
|
Development Groups. NICE: London |
|||
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926
Porter: Tidy's Physiotherapy, 14th Edition
References 19
Royal College of Nursing, University of Leicester, National Institute for Clinical Excellence 2002 Principles for Best Practice in Clinical Audit. Radcliffe
Medical: Oxford
Royal College of Physicians 2005 Doctors in society: medical professionalism in a changing world: Report of a Working Party of the Royal College of Physicians of London. RCP: London
Sackett DL, Rosenberg WMC, Gray JAM et al. 1996
Secretary of State for Health 1998 A First Class Service:
Quality in the New NHS. Department of Health:1 London
Sudlow M, Thomson R 1997 Clinical guidelines: quantity without quality (editorial). Qual Health Care 6:
World Congress for Physical Therapy 1999 Declaration of Principles and Position Statements. London: WCPT. www.wcpt.org; accessed 29 November 2006
|
|
ELSEVIER |
FINAL |
||
|
|
|
|||
|
|
|
- |
NOT |
|
|
CONTENT |
|
|
||
|
|
|
|
||
PROPERTY |
OF |
|
|
|
|
|
|
|
|
|
|
SAMPLE |
|
|
|
|
|
http://www.us.elsevierhealth.com/product.jsp?isbn=9780443103926