The PDF editor that you will begin using was made by our top level programmers. One could complete the emdeon therapy first plus form quickly and without problems applying our software. Just keep up with the following guide to start out.
Step 1: The first step would be to click on the orange "Get Form Now" button.
Step 2: You'll notice all the functions which you can undertake on the template once you've got entered the emdeon therapy first plus editing page.
Prepare the emdeon therapy first plus PDF by entering the data needed for each section.
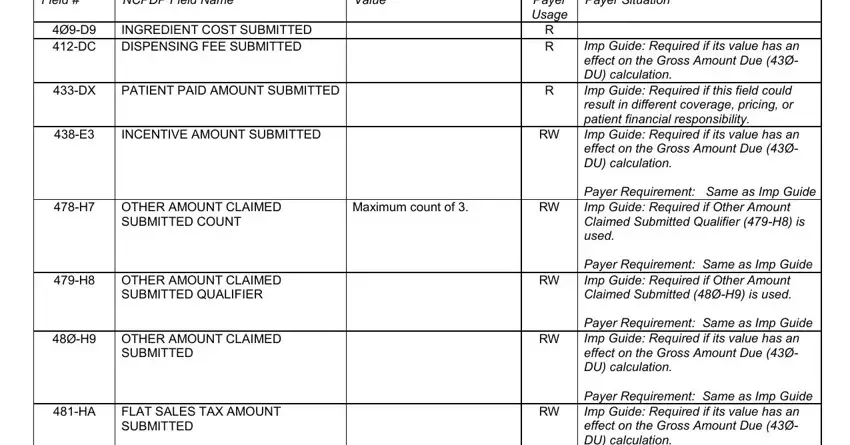
Fill out the PERCENTAGE SALES TAX AMOUNT, PERCENTAGE SALES TAX RATE SUBMITTED, Payer Requirement Same as Imp, Payer Requirement Same as Imp, Required if this field could, Required if needed to calculate, Payer Requirement Same as Imp, and Materials Reproduced With the field with all the details required by the system.
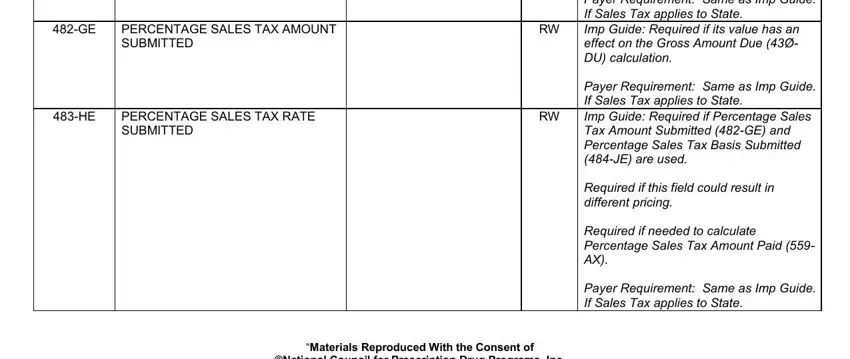
Put together the significant particulars in the Pricing Segment Segment, Value, Field, PERCENTAGE SALES TAX BASIS, USUAL AND CUSTOMARY CHARGE, ØDU DN, GROSS AMOUNT DUE BASIS OF COST, Payer Situation, Imp Guide Required if Percentage, Required if this field could, Required if needed to calculate, Payer Requirement Same as Imp, Imp Guide Required if needed for, Payer Usage RW, and R R segment.
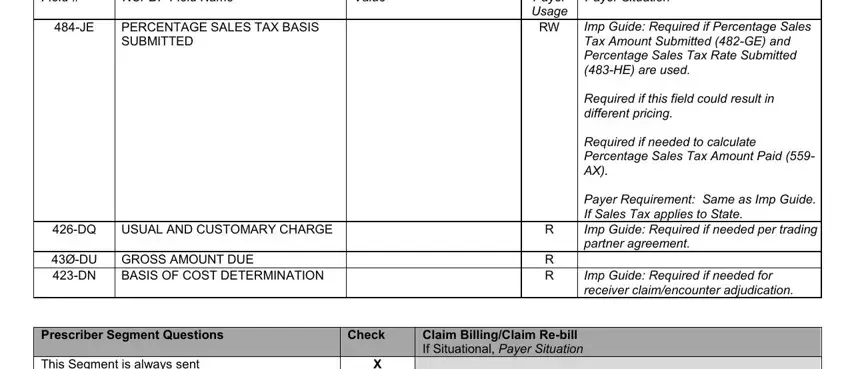
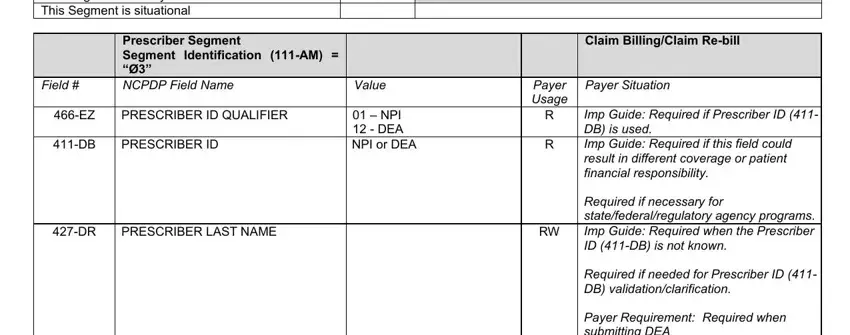
The This Segment is always sent This, Prescriber Segment Segment, Field, PRESCRIBER ID QUALIFIER, PRESCRIBER ID, Value, NPI DEA NPI or DEA, PRESCRIBER LAST NAME, Claim BillingClaim Rebill, Payer Usage R, Payer Situation, Imp Guide Required if Prescriber, Required if necessary for, Required if needed for Prescriber, and Payer Requirement Required when box is the place to include the rights and obligations of all parties.
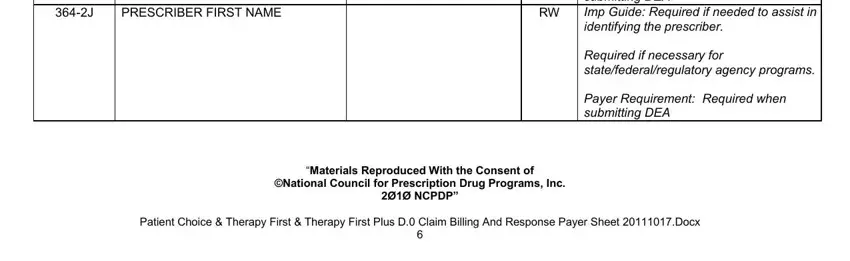
Look at the areas PRESCRIBER FIRST NAME, Payer Requirement Required when, Required if necessary for, Payer Requirement Required when, Materials Reproduced With the, and Patient Choice Therapy First and next fill them in.
Step 3: Once you have hit the Done button, your form will be available for upload to any gadget or email address you specify.
Step 4: Have a duplicate of each file. It's going to save you time and make it easier to avoid challenges down the road. Also, your information isn't revealed or monitored by us.