California Do Not Resuscitate Order (DNR) Form
The do not resuscitate order form is a document that proves the patient’s desire not to save their life—thus, not to resuscitate them—in case their heart or other vital organs stop functioning. The form prevents the usage of many forms of medical treatment if the patient’s vital system fails to work. All the medical staff serving the particular patient must be acknowledged about the presence of the order.
The form is often signed when the health of the patient is seen to be continuously deteriorating. The patient or their trusted proxy desires to stop the treatment in case of a further reduction.
Build Your Document
Answer a few simple questions to make your document in minutes
Save and Print
Save progress and finish on any device, download and print anytime
Sign and Use
Your valid, lawyer-approved document is ready
Which Procedures does the DNR Form Include?
The form covers anything touching on the patient’s cardiopulmonary attack.
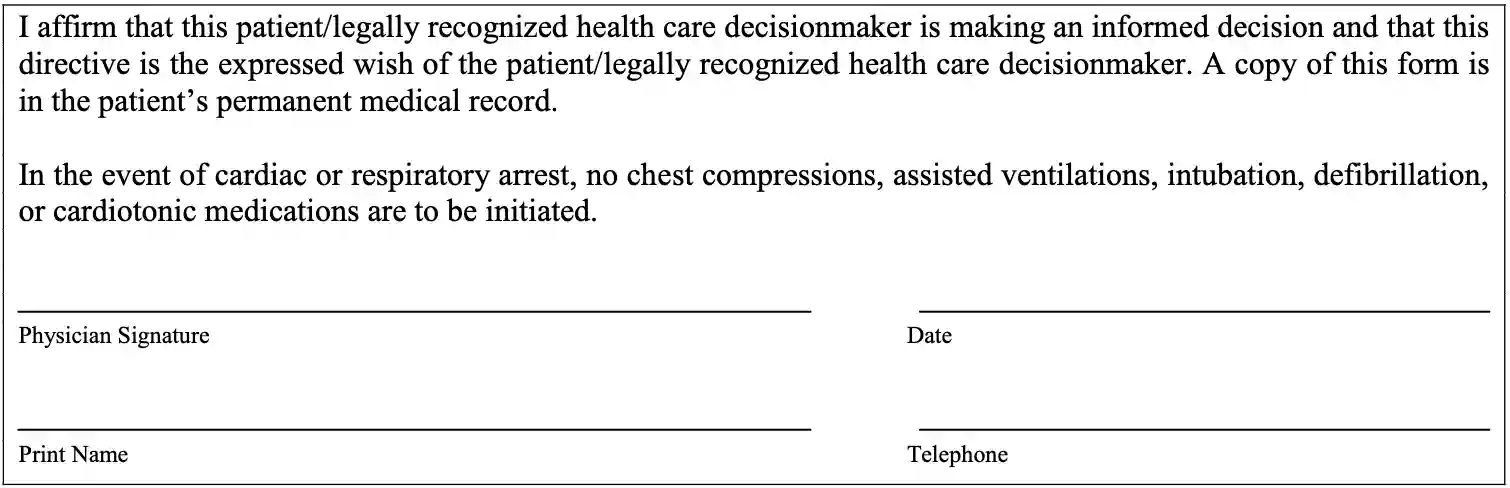
It restrains the California Medical Association and EMS staff (emergency medical services) from engaging in such treatment as:
- defibrillation
- chest compression (CPR)
- any types of stimulating drugs (stimulants)
- endotracheal intubation
- angioplasty
- assisted ventilation (breathing)
However, the DNR form cannot stop the physicians from providing life-sustaining types of equipment (artificial subsistence, hydration, vitamins), treatments to decrease pain, delays in breathing, or bleeding (including inner bleeding).
Terms of the DNR Form Completion
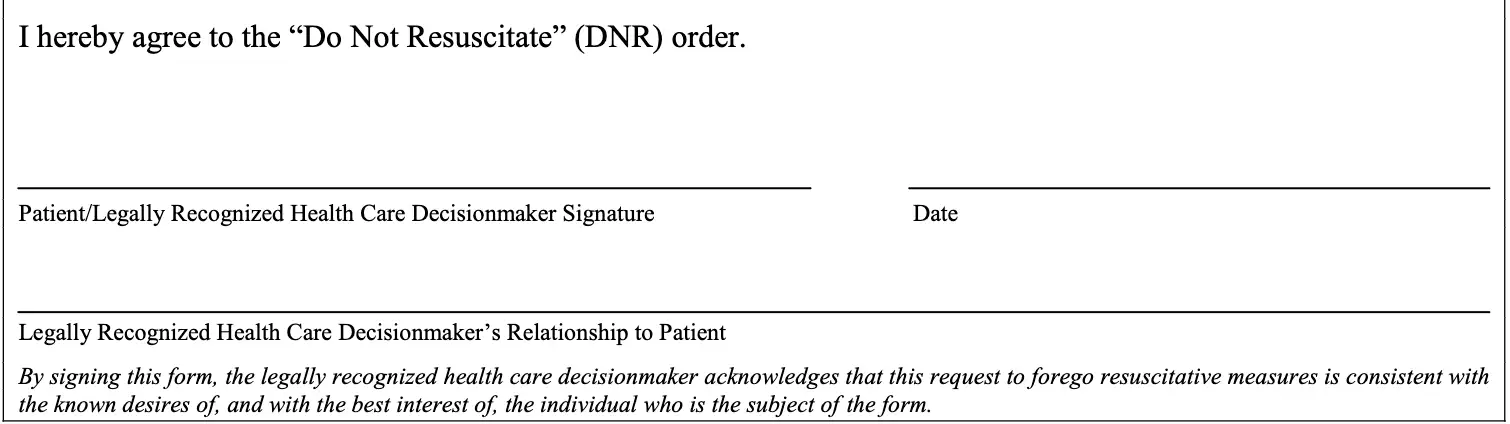
According to local legislation (all the rights and responsibilities of both sides included in PROB § 4780), both the patient and their primary physician must sign the form. If the primary physician is unable to do so, the second doctor fills in the position. Moreover, there must be two witnesses at the moment of signing; optionally, a public notary may be involved. If the patient is incapable of completing the document, their representative should act on their behalf.
Alternatively, the witness must be present at the patient’s verbal consent to set the DNR form. All the participants should follow the local signing requirements.
How to Fill the DNR Form
Stage 1. Take a look and print the form required by California state.
Stage 2. As the patient, insert your full printed name and once again review all the employed agreements to be sure you are ready to leave such an important authority to your physician.
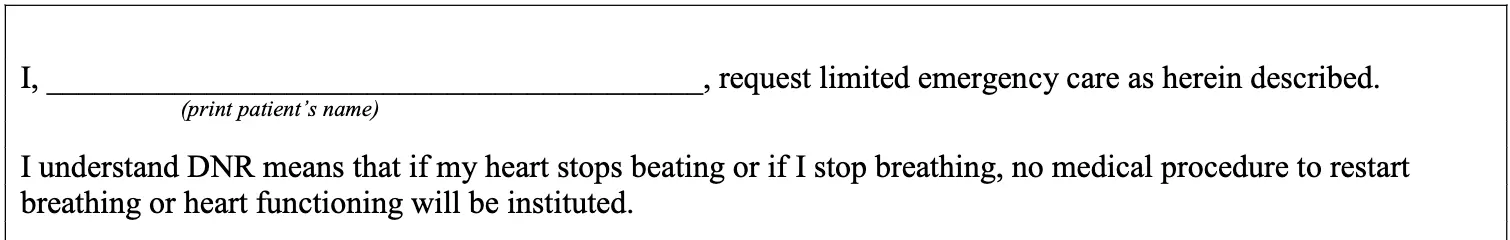
Stage 3. If the patient is capable of independent decisions and physical actions, they must sign the form by themselves and write the date of the signing. However, if the patient is incapacitated, their attorney-in-form or a trusted medical proxy can sign the form, leave the date, and fill the following field with their relationship tie to the patient.
Stage 4. The second part of the document is dedicated to the physician. As follows, the doctor should appreciate the existence of the form by leaving their printed name, signature, date, and optionally the phone number.
Stage 5. After completing the form, the patient (or their medical proxy) or the physician should check if the copy of the form is placed near the patient’s couchette. It is also possible for the patient to wear a special indicator that informs the people around about the presence of such a desire. The permanent personnel taking care of the patient must also be notified about the document completion, thus, of the patient’s will.