Understanding the essentials of the 07 21 Hhsa form is integral for individuals navigating through the complex landscape of health and human services assistance. This particular form stands as a cornerstone document, enabling applicants to access a wide array of services provided by health and human services agencies. It serves not merely as a bureaucratic necessity but as a lifeline for many seeking crucial support, including but not limited to health care, nutritional assistance, and other social services. The form takes into account various facets of an applicant's personal and financial status to ensure a comprehensive evaluation of their needs. As such, it is meticulously designed to gather necessary information, streamline the application process, and facilitate the efficient delivery of services. For those embarking on the filing process, a thorough understanding of the form's components, its purpose, and how it seamlessly integrates into the larger framework of health and human services assistance cannot be overstated.
| Question | Answer |
|---|---|
| Form Name | 07-21 HHSA Form |
| Form Length | 1 pages |
| Fillable? | Yes |
| Fillable fields | 57 |
| Avg. time to fill out | 11 min 39 sec |
| Other names | sworn statement form, 07 21 form hhsa, 07 21 employment verification, ca 07 21 hhsa employment verification form |

A.9.1
Forms
Forms
FORM NUMBER |
FORM TITLE |
Request for Withdrawal or |
|
(SP) |
Discontinuance of Benefits |
Employment Verification |
|
(SP) |
|
Case Narrative |
|
Statement of Contribution & |
|
(SP) |
Declaration of a Loan/Gift |
Self Employment Income |
|
(SP) |
Statement |
Medical Services Screening |
|
Applicant Notice of |
|
|
Decentralization |
Transmittal of |
|
|
Information |
District Notice of |
|
|
Decentralization |
Sworn Statement |
|
(SP) |
|
CW 60 / CW 60 (SP) |
Release of Information – |
|
Financial Institution |
DHS 6155 |
Health Insurance |
|
Questionnaire |
HHSA: |
CMS General Property |
Limitations Notice |
|
HHSA: |
CMS SSI Advocacy Referral |
2(SP) |
|
HHSA: |
CMS Weekly Screening Log |
HHSA: |
Registration Information |
HHSA: |
|
HHSA: |
Third Party Liability Report |
HHSA: |
|
HHSA: |
Affidavit Residence (Spanish |
on Reverse) |
|
HHSA: |
Rights of Applicants |
|
|
HHSA: HCPA |
Authorization for Release of |
Information |
|
HHSA: |
Responsibilities of Applicants |
|
HHSA: |
Verification Checklist |
|
|
HHSA: |
Provider Statement (Spanish |
on Reverse) |
|
HHSA: |
Eligibility Narrative Checklist |
HHSA: |
Reminder Request for |
CMS 22 (SP) |
Verifications |
HHSA: |
Coverage Information |
|
|
HHSA: |
Decentralized Patient Letter |
|
|
HHSA: |
Fraud Referral |
HHSA: |
Request For Information |
|
|
HHSA: |
Repayment Demand Letter |
|
|
HHSA: |
Informing Letter |
|
|
HHSA: |
Income Work Sheet |
HHSA: |
Hardship Budget Work Sheet |
HHSA: |
Clinic Screening Sheet |
HHSA: |
Fraud Investigation Referral |
|
Narrative |
HHSA: |
General Relief Log |
HHSA: |
Health Insurance |
|
Questionnaire |
HHSA: |
Urgent Eligibility Request |
|
|
HHSA: |
Primary Care Services |
|
Transmittal |
HHSA: |
Clinic Statistics |
HHSA: |
|
|
Referral |
HHSA: |
Authorization For Release Of |
|
Medical Records |
HHSA: |
Important Information For |
|
Veterans |
HHSA: |
IDX Alert Referral |
HHSA: |
Credit Check Authorization |
99 (SP) |
|
HHSA: |
Statement of Facts |
|
|
HHSA: |
Agreement to Reimburse the |
County of San Diego |
|
HHSA: |
Image Verification Checklist |
|
|
HHSA: |
Share of Cost |
HHSA: |
Reimbursement Informing |
Notice |
|
HHSA: |
CMS Questions and Answers |
|
|
HHSA: |
Overpayment Payment and |
|
Collection Letter |
HHSA: |
Overpayment Collection |
|
Letter |
HHSA: |
Referral to BRCTP |
HHSA: |
Health Services Information |
|
for Native Americans |
HHSA: |
CMS Grant of Lien |
|
|
HHSA: |
CMS Lien Information |
|
|
HHSA: |
CMS Lien Acknowledgment |
|
Statement |
HHSA: |
County Medical Services |
Medical Need Form |
|
HHSA: |
Authorization For Release of |
CMS: |
Information |
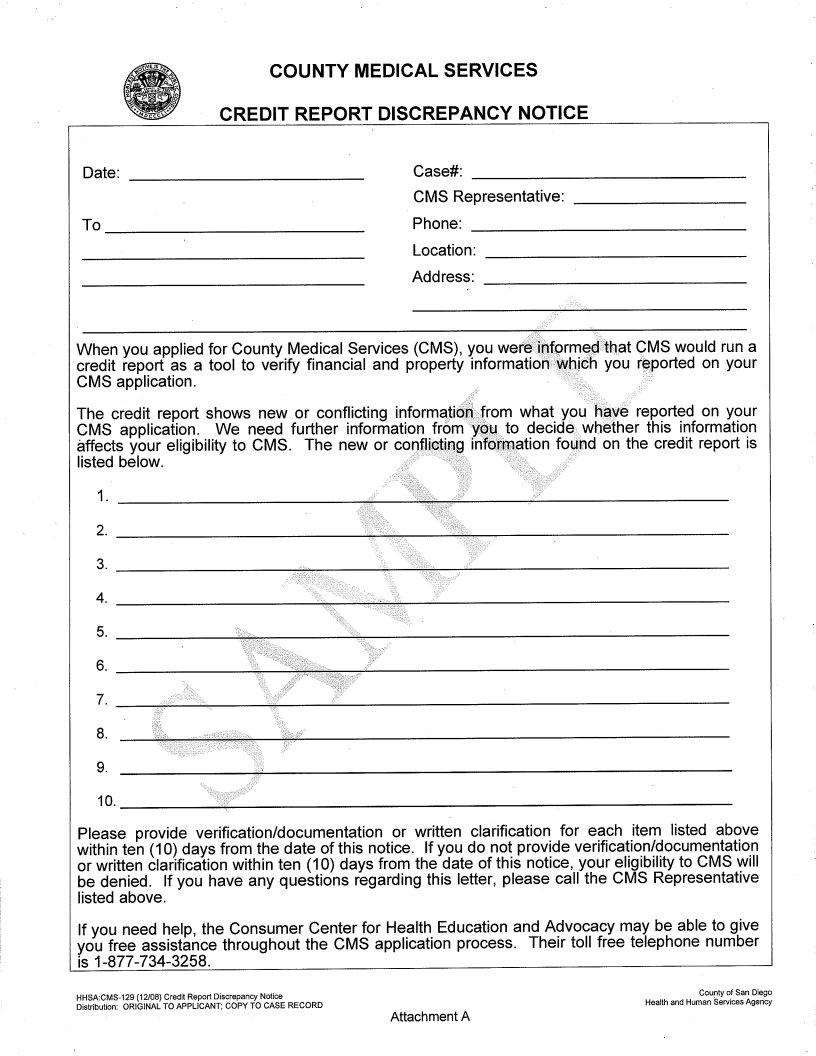
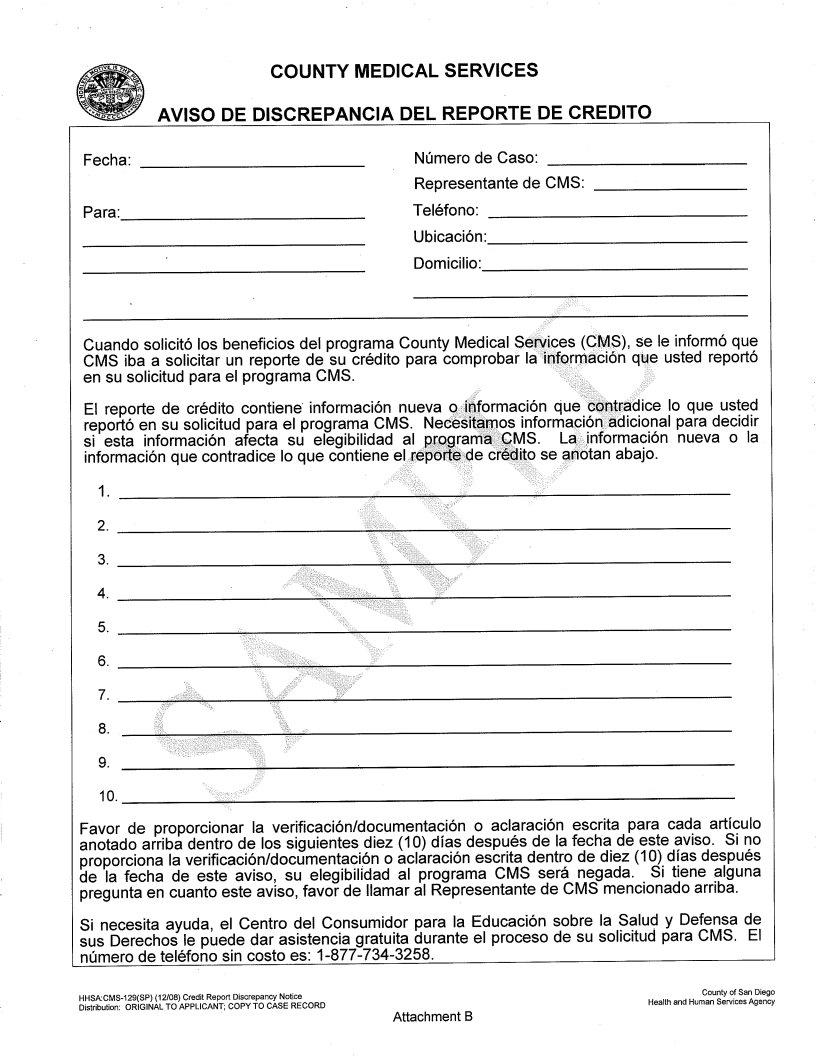
HHSA: |
Credit Report Discrepancy |
CMS: |
Notice |
|
|
MC 176M and MC 176W |
SOC Determination (CFBU) |
|
includes ABD Spouse or |
|
Parent) |
|
|
MC 176P |
Property Reserve Work |
|
Sheet |
MC 210 |
Statement of Facts |
None |
Fair Hearing Decision |
MPG Letter #666 (02/09)
A.8.1
CMS IT System
General The CMS IT System is a

A.
CMS Notices of Action (NOA)
verifications will be stored on the CMS IT System. The CMS IT System will also afford CMS contracted providers the ability to access the website to view CMS case status.
1) NOAs requiring manual mailing
a) Homeless
The CMS IT System will create various NOAs and Informing Notices for homeless patients, but will not automatically mail the notices. The notices will be stored in the patient’s record on the CMS IT System.
If the patient requests a copy of their NOA or Informing Notice, the worker will be able to access the notice and print it on site for the patient. The worker shall make a narrative entry indicating the date the notice was provided, and shall specify which notice was provided.
b)Excess Income Only Denials
The CMS IT System will create the Excess Income Only Denial NOA, but will not automatically mail the notice. The denial NOA will be available in patient’s record on the CMS IT System the following workday after the denial action was taken by the worker.
The worker shall access the patient’s record the next workday following the denial action and shall print the Excess Income Only Denial NOA. The worker shall mail the Excess Income Only Denial NOA and CMS Hardship Application (refer to Article A, Section 13) to the patient. The worker shall make a narrative entry indicating the date the notice was provided, and shall specify which notice was provided.
2)NOAs which will be automatically mailed
a)CMS Approval
The certification period will be automatically filled in prior to the NOA being mailed.
b)Denial NOAs except Excess Income Only
Workers shall enter all case specific information applicable to the denial into the system at the time the denial action is taken (ie, what specific items the patient failed to provide, the amount the patient needs to spend down). The case specific information will be
B.
Approval
Action
C.
Denial Action
D.
Credit Report
Request
automatically filled in prior to the NOA being mailed.
Based on the applicant’s/beneficiaries information entered, the CMS IT System will determine if the client is approved for CMS benefits.
All approval actions taken by the worker will remain in a “pending approval” status for a minimum of one night. Fifty percent of all approvals must be reviewed and released by a supervisor. Each night the CMS IT System will randomly select from the pending approvals, which approvals are to be reviewed by a supervisor, which pending approvals can be approved without a supervisor review.
Based on the applicant’s/beneficiaries information entered, the CMS IT System will determine the appropriate denial action, generate a denial NOA and automatically mail it to applicant as appropriate. Some denial NOAs require manual mailing.
Worker must order a credit report at initial application, recertification or reapplication when information is received from applicant/beneficiary or circumstances are noted which could indicate the possibility of fraud. Reasonable care must be taken to input the applicant’s/beneficiary’s identification information accurately when requesting a credit profile report. CMS will use the credit report as a verification tool for financial, property and eligibility information, which the applicant/beneficiary has provided on their application for CMS. At the end of each business day, the CMS IT System will batch and submit all credit report requests to Experian. The credit profile report is received from Experian on the following business day. Worker must
found on report. Worker must verify that all verifications/documents are provided to clear up discrepancy on report to evaluate for CMS eligibility as described in MPG Article A Sections 2 and 13. NOTE: The credit check authorization is good for only one (1) credit report profile request.
Credit reports obtained through the CMS IT System may not be given to the applicant/beneficiary. If the applicant/beneficiary requests a copy of their credit report, refer them to the sources

listed on the Credit Check Authorization form
MPG Letter #666 (2/09)