It is very easy to fill in the ar dhsar medicaid card gaps. Our software makes it nearly effortless to work with any kind of form. Down the page are the basic four steps you need to consider:
Step 1: Select the "Get Form Now" button to get going.
Step 2: Now you will be within the document edit page. You can include, adjust, highlight, check, cross, insert or remove fields or phrases.
Get the ar dhsar medicaid card PDF and type in the details for each segment:
Complete the Medicaid ARKids First and Your New, Getting to the Doctor NonEmergency, Transportation NET, Covered Services, Adult Development Day Treatment, and Ambulance Service Emergency Only section with all the data requested by the program.
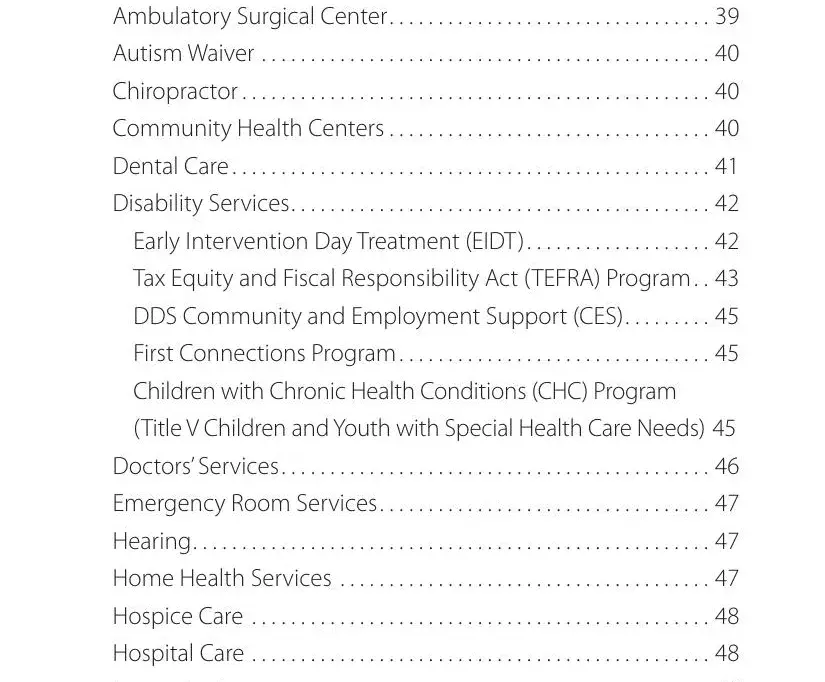
You need to highlight the vital data in the Ambulatory Surgical Center, Autism Waiver, Chiropractor, Dental Care, Disability Services, Early Intervention Day Treatment, Tax Equity and Fiscal, DDS Community and Employment, First Connections Program, Children with Chronic Health, Title V Children and Youth with, Doctors Services, Emergency Room Services, Hearing, and Home Health Services field.
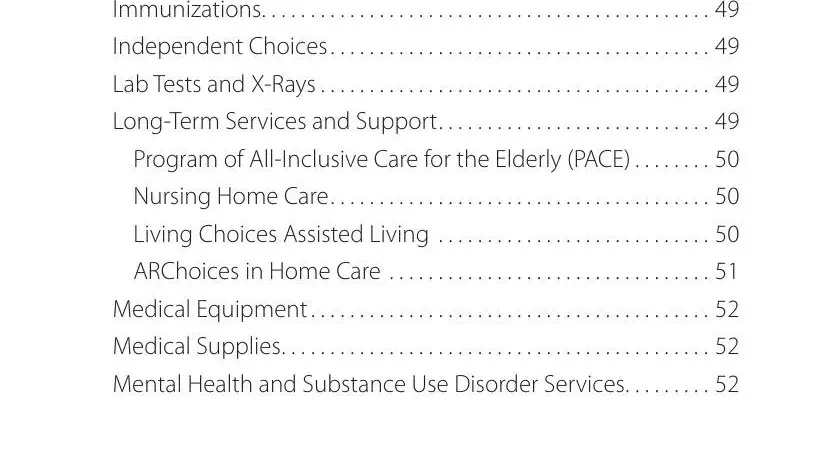
The Immunizations, Independent Choices, Lab Tests and XRays, LongTerm Services and Support, Program of AllInclusive Care for, Nursing Home Care, ARChoices in Home Care, Medical Equipment, Medical Supplies, and Mental Health and Substance Use field is the place to insert the rights and responsibilities of each side.
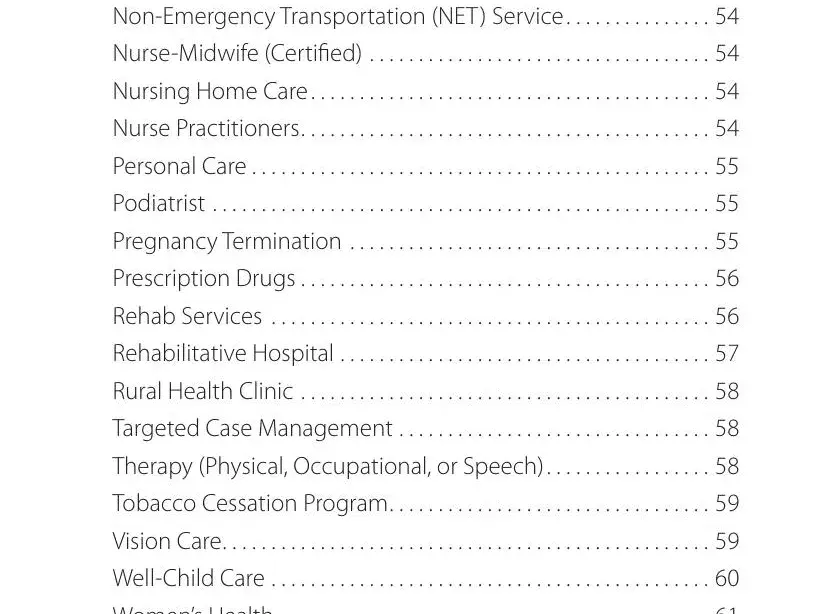
Finalize the template by checking these sections: NonEmergency Transportation NET, NurseMidwife Certified, Nursing Home Care, Personal Care, Podiatrist, Pregnancy Termination, Prescription Drugs, Rehab Services, Rehabilitative Hospital, Rural Health Clinic, Targeted Case Management, Therapy Physical Occupational or, Tobacco Cessation Program, Vision Care, and WellChild Care.
Step 3: Once you select the Done button, your prepared form can be transferred to any of your gadgets or to email indicated by you.
Step 4: To prevent any type of concerns in the long run, try to prepare at the very least two or three copies of the document.