Working with PDF files online is quite easy with our PDF tool. Anyone can fill in florida blue prior authorization form pdf here effortlessly. The editor is constantly improved by our staff, receiving handy features and becoming greater. With just several simple steps, you can start your PDF journey:
Step 1: Just press the "Get Form Button" in the top section of this webpage to launch our pdf file editing tool. Here you will find everything that is necessary to work with your document.
Step 2: The editor offers the opportunity to work with nearly all PDF files in a variety of ways. Enhance it by writing any text, adjust original content, and add a signature - all when it's needed!
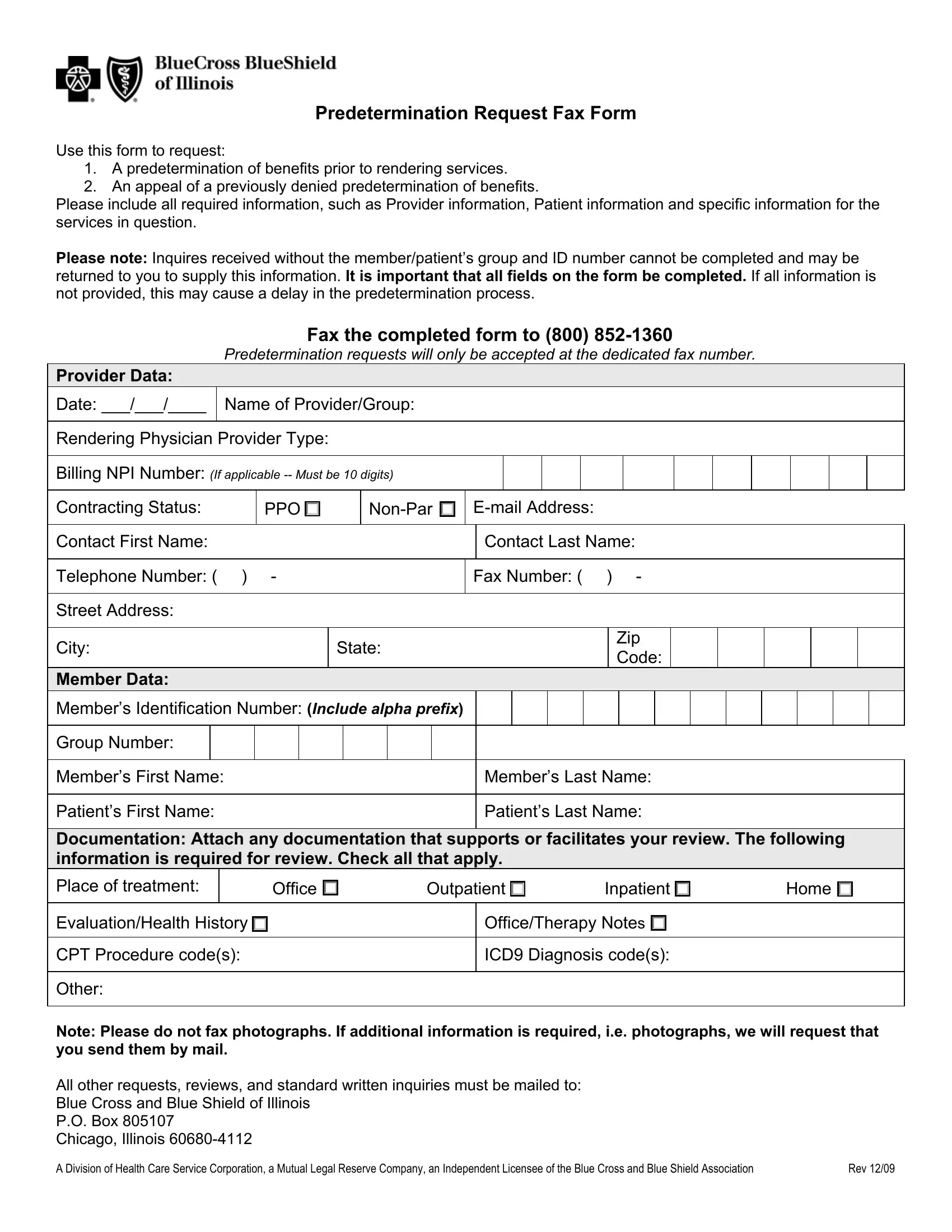
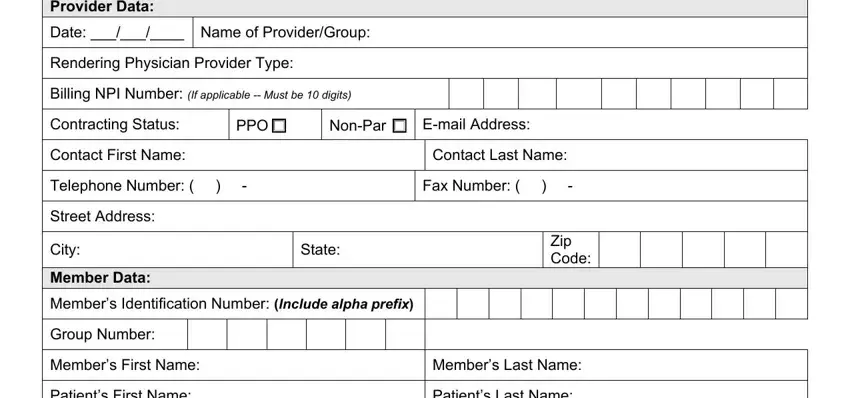
This form will need specific data to be entered, so be sure to take your time to type in precisely what is expected:
1. First, when filling in the florida blue prior authorization form pdf, start out with the form section containing next blank fields:
2. After this section is filled out, proceed to enter the relevant details in all these: Documentation Attach any, Place of treatment, Office , Outpatient , Inpatient , Home , EvaluationHealth History , CPT Procedure codes, Other, OfficeTherapy Notes , ICD Diagnosis codes, Note Please do not fax photographs, A Division of Health Care Service, and Rev .
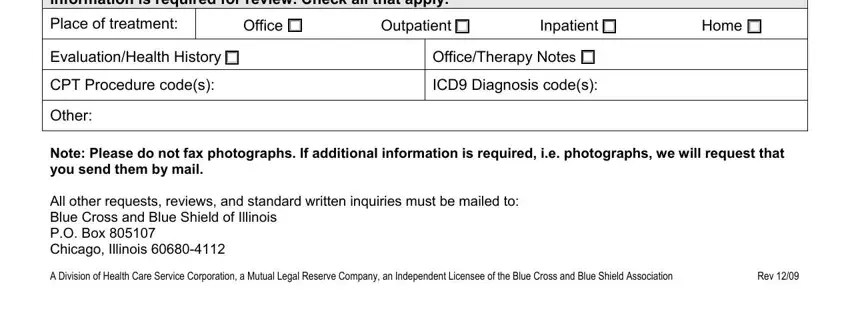
It is possible to make an error while completing your EvaluationHealth History , so ensure that you reread it before you'll finalize the form.
Step 3: Prior to submitting this document, make certain that blanks have been filled in right. Once you think it's all good, click on “Done." Make a free trial account with us and gain instant access to florida blue prior authorization form pdf - accessible from your FormsPal account page. We do not share any information that you type in while completing documents at FormsPal.