PRIOR AUTHORIZATION REQUEST FORM
EOC ID:
BMCHPQHP Blood Clotting Disorder Medications (2)
Policy 9.165
FEIBA VH, FEIBA NF, NovoSeven, NovoSeven RT
Phone: 855-264-4964 Fax back to: 877-503-7231
manages the pharmacy drug benefit for your patient. Certain requests for coverage require review with the prescribing physician. Please answer the following questions and fax this form to the number listed above. Please note any information left blank or illegible may delay the review process.
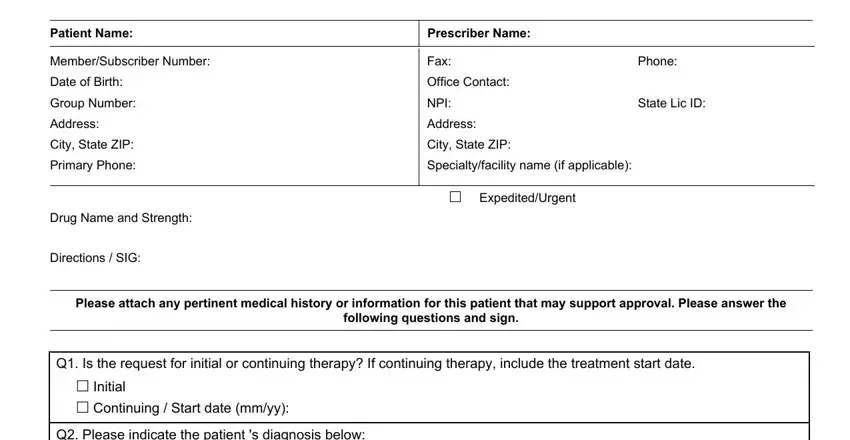
Patient Name: |
Prescriber Name: |
|
|
|
|
|
|
Member/Subscriber Number: |
Fax: |
Phone: |
|
Date of Birth: |
Office Contact: |
|
|
Group Number: |
NPI: |
State Lic ID: |
|
Address: |
Address: |
|
|
City, State ZIP: |
City, State ZIP: |
|
|
Primary Phone: |
Specialty/facility name (if applicable): |
|
|
|
|
|
|
|
Expedited/Urgent |
|
|
Drug Name and Strength: |
|
|
|
Directions / SIG: |
|
|
|
Please attach any pertinent medical history or information for this patient that may support approval. Please answer the
following questions and sign.
Q1. Is the request for initial or continuing therapy? If continuing therapy, include the treatment start date.
Initial
Continuing / Start date (mm/yy):
Q2. Please indicate the patient 's diagnosis below:
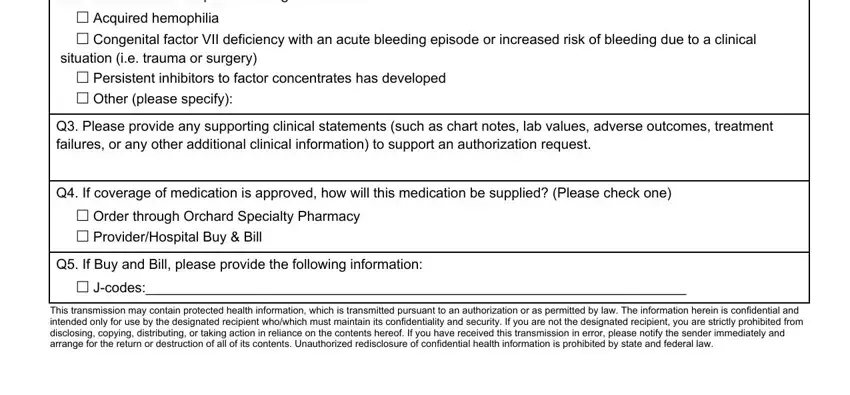
Acquired hemophilia
Congenital factor VII deficiency with an acute bleeding episode or increased risk of bleeding due to a clinical situation (i.e. trauma or surgery)
Persistent inhibitors to factor concentrates has developed
Other (please specify):
Q3. Please provide any supporting clinical statements (such as chart notes, lab values, adverse outcomes, treatment failures, or any other additional clinical information) to support an authorization request.
Q4. If coverage of medication is approved, how will this medication be supplied? (Please check one)
Order through Orchard Specialty Pharmacy
Provider/Hospital Buy & Bill
Q5. If Buy and Bill, please provide the following information:
J-codes:______________________________________________________________________
This transmission may contain protected health information, which is transmitted pursuant to an authorization or as permitted by law. The information herein is confidential and intended only for use by the designated recipient who/which must maintain its confidentiality and security. If you are not the designated recipient, you are strictly prohibited from disclosing, copying, distributing, or taking action in reliance on the contents hereof. If you have received this transmission in error, please notify the sender immediately and arrange for the return or destruction of all of its contents. Unauthorized redisclosure of confidential health information is prohibited by state and federal law.
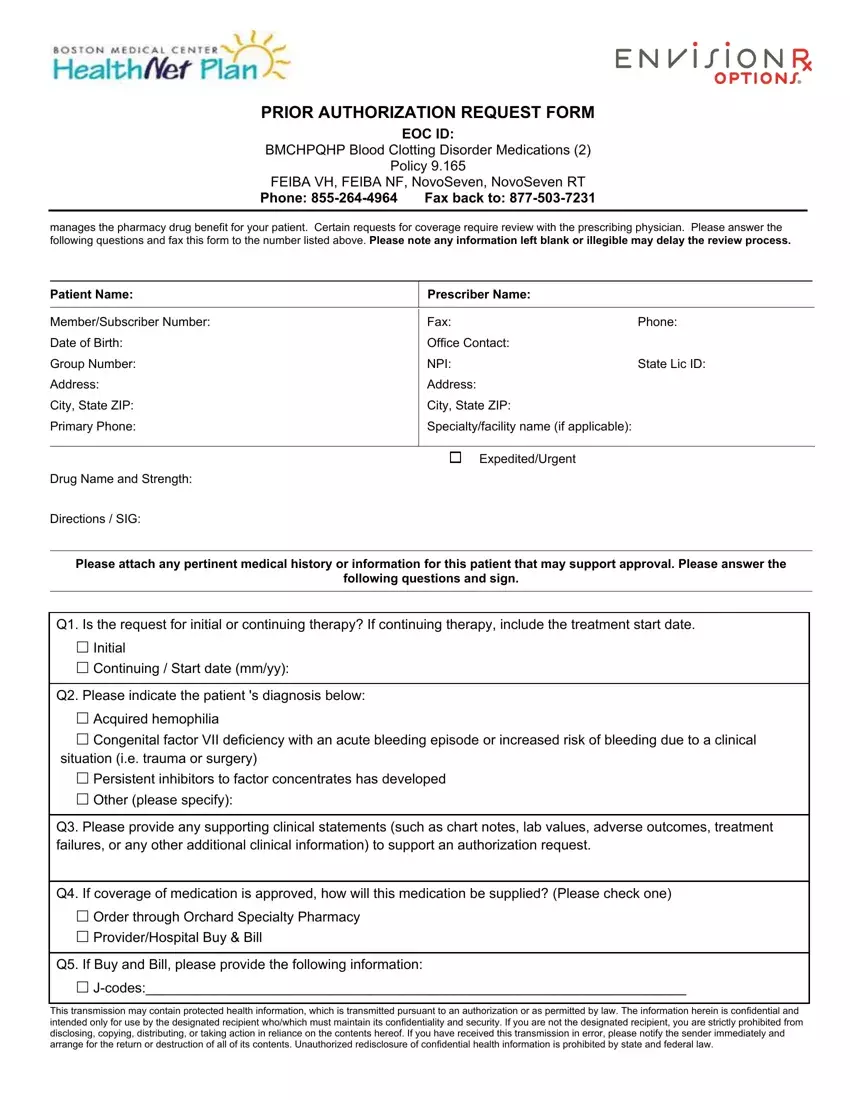
PRIOR AUTHORIZATION REQUEST FORM
EOC ID:
BMCHPQHP Blood Clotting Disorder Medications (2)
Policy 9.165
FEIBA VH, FEIBA NF, NovoSeven, NovoSeven RT
Phone: 855-264-4964 Fax back to: 877-503-7231
manages the pharmacy drug benefit for your patient. Certain requests for coverage require review with the prescribing physician. Please answer the following questions and fax this form to the number listed above. Please note any information left blank or illegible may delay the review process.
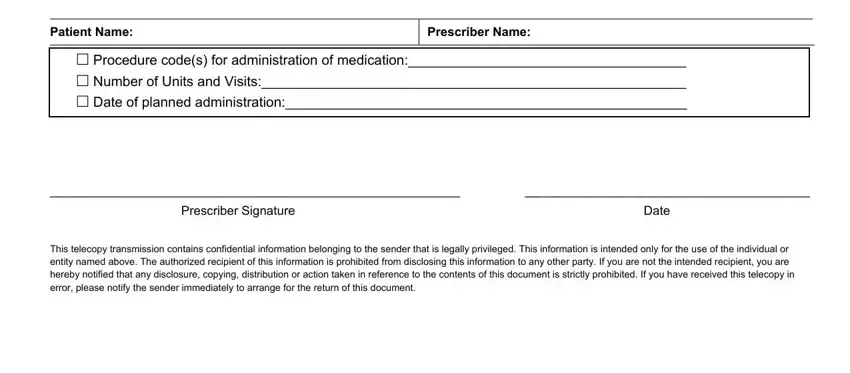
Procedure code(s) for administration of medication:____________________________________
Number of Units and Visits:_______________________________________________________
Date of planned administration:____________________________________________________
___________________________________________________________ |
_________________________________________ |
Prescriber Signature |
Date |
This telecopy transmission contains confidential information belonging to the sender that is legally privileged. This information is intended only for the use of the individual or entity named above. The authorized recipient of this information is prohibited from disclosing this information to any other party. If you are not the intended recipient, you are hereby notified that any disclosure, copying, distribution or action taken in reference to the contents of this document is strictly prohibited. If you have received this telecopy in error, please notify the sender immediately to arrange for the return of this document.
This transmission may contain protected health information, which is transmitted pursuant to an authorization or as permitted by law. The information herein is confidential and intended only for use by the designated recipient who/which must maintain its confidentiality and security. If you are not the designated recipient, you are strictly prohibited from disclosing, copying, distributing, or taking action in reliance on the contents hereof. If you have received this transmission in error, please notify the sender immediately and arrange for the return or destruction of all of its contents. Unauthorized redisclosure of confidential health information is prohibited by state and federal law.