We were designing this PDF editor with the idea of allowing it to be as quick to apply as possible. For this reason the entire process of filling in the printable braden scale will undoubtedly be smooth perform all of these steps:
Step 1: The first step should be to choose the orange "Get Form Now" button.
Step 2: So, you can begin editing the printable braden scale. The multifunctional toolbar is at your disposal - insert, eliminate, transform, highlight, and perform other commands with the content material in the file.
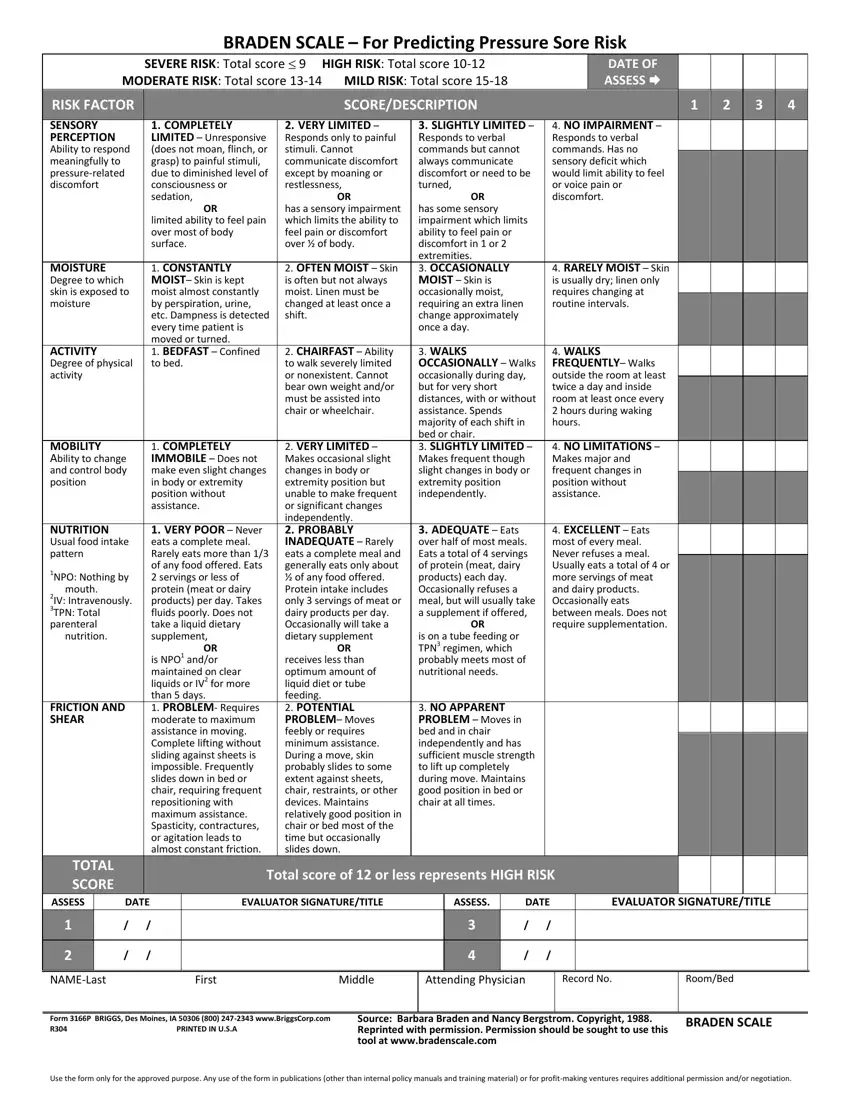
These sections will help make up your PDF file:
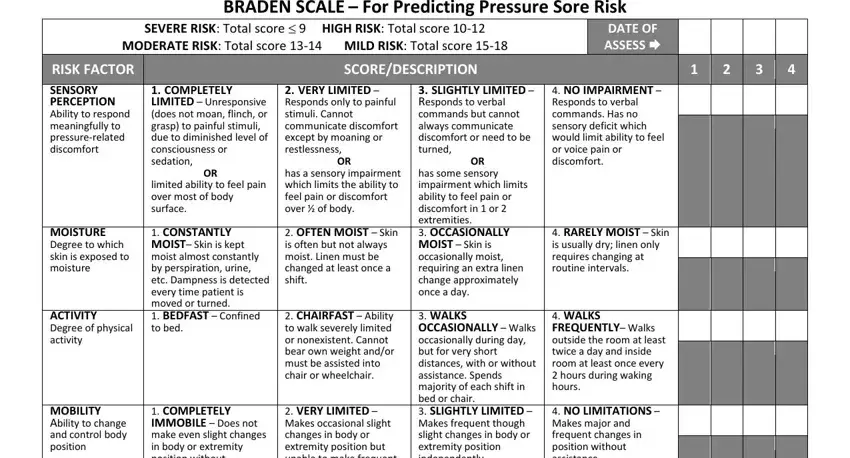
You have to fill in the NUTRITION Usual food intake pattern, NPO Nothing by mouth IV, FRICTION AND SHEAR, EXCELLENT Eats most of every, COMPLETELY IMMOBILE Does not, VERY POOR Never eats a complete, OR is NPO andor maintained on, VERY LIMITED Makes occasional, receives less than optimum amount, ADEQUATE Eats over half of most, is on a tube feeding or TPN, NO APPARENT PROBLEM Moves in bed, TOTAL SCORE, ASSESS, and DATE space with the required details.
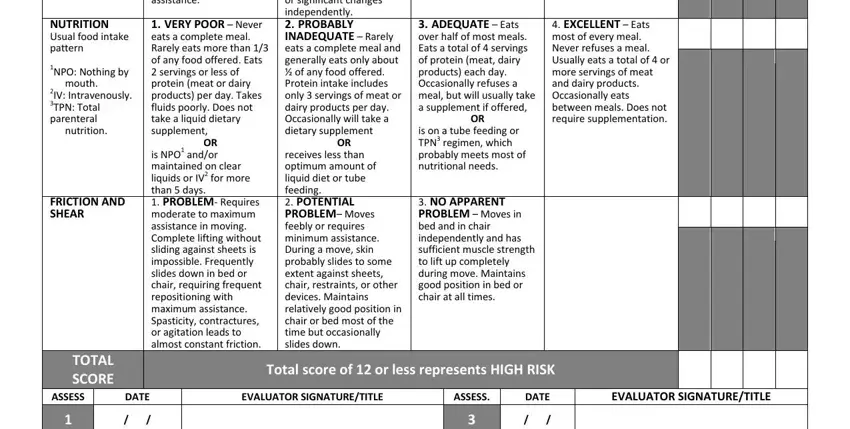
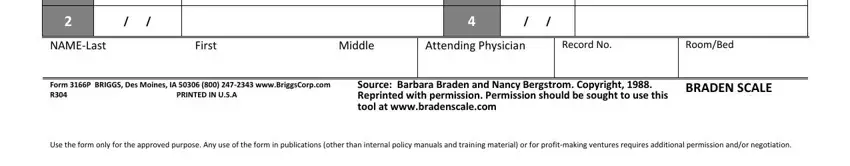
Put down the vital information since you are within the NAMELast, First, Middle, Attending Physician, Record No, RoomBed, Form P BRIGGS Des Moines IA, Source Barbara Braden and Nancy, BRADEN SCALE, and Use the form only for the approved section.
Step 3: Click the "Done" button. So now, it is possible to export the PDF document - download it to your electronic device or forward it by using electronic mail.
Step 4: Create copies of the form - it will help you keep away from potential troubles. And don't be concerned - we do not distribute or read your information.