Navigating the complexities of healthcare expenses can be challenging, especially when it comes to pharmaceutical costs. The Catamaran Direct Member Reimbursement form serves as a lifeline for those who find themselves paying out-of-pocket for prescription medication due to various circumstances. This essential document outlines a clear process for members to seek reimbursement for medication expenses that should have been covered under their plan. It emphasizes the importance of providing detailed pharmacy receipts or, in their absence, a pharmacist’s verification and signature along with proof of payment. The form requires comprehensive information including the patient's name, date of birth, plan participant identification number, mailing address, and specific details about the medication purchased such as the drug name, physician, prescription number, and the amount paid. Furthermore, it outlines the reasons a member might request reimbursement, ranging from not having the Catamaran prescription drug card at the time of purchase to making an out-of-network purchase. All claims are subjected to the terms and conditions of the plan, reminding members that reimbursements may be adjusted based on various factors such as plan cost and copayments. The process for submission is streamlined, offering fax and mail options, and underscores the legal implications of submitting false claims, highlighting the importance of accuracy and honesty in the reimbursement process.
| Question | Answer |
|---|---|
| Form Name | Catamaran Direct Member Reimbursement Form |
| Form Length | 1 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 15 sec |
| Other names | reimbursement claim catamaran form, Catamaran, NPI, catamaran insurance reimbursement |
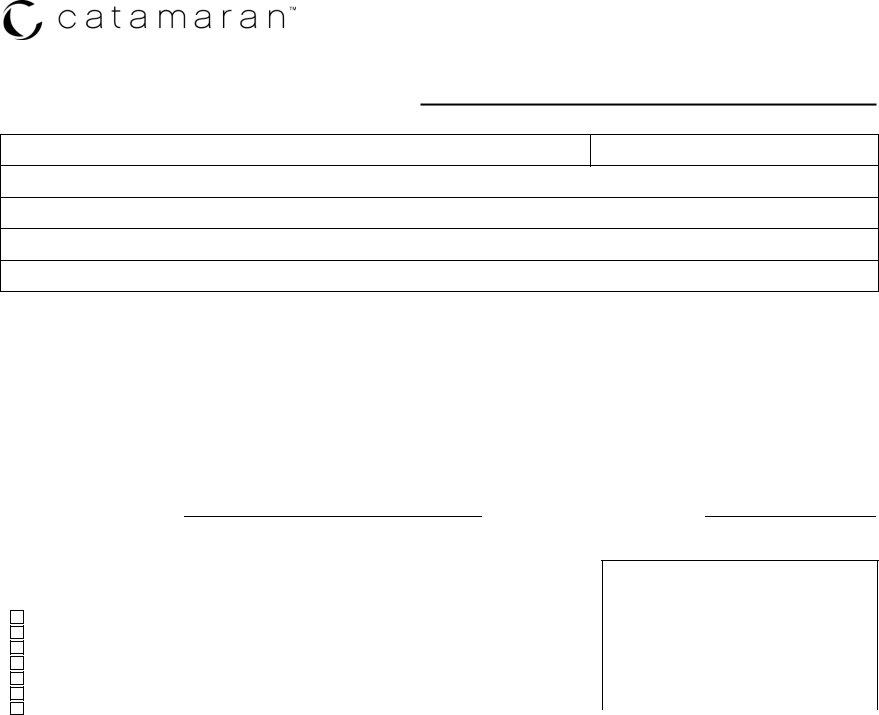
DIRECT MEMBER REIMBURSEMENT FORM
Please attach a detailed receipt from the pharmacy, including all of the following information. If this information is not on the receipt, please have the pharmacist complete and sign this form and attach proof of payment. Without the required information, Catamaran will not be able to process your claim.
PRESCRIPTION FILLED FOR (Patient Name):DATE OF BIRTH (Patient DOB): PLAN PARTICIPANT IDENTIFICATION NUMBER (Printed on prescription card):
MAILING ADDRESS:
PLAN NAME (Employer or Group Name):
|
Pharmacy |
Fill |
Drug Name |
|
Physician |
|
Days |
Amount |
|
|
|
|
|||||||
Rx # |
NDC Number |
Quantity |
|||||||
NABP/NPI # |
Date |
(including strength) |
DEA/NPI # |
Supply |
Paid |
||||
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PHARMACIST SIGNATURE:PHARMACY PHONE NUMBER:
*PHARMACIST SIGNATURE IS REQUIRED WHEN A DETAILED RECEIPT IS NOT PROVIDED.
All reimbursements are subject to plan terms and conditions and may be reduced from the submitted amounts based on plan cost and copayments. Any reimbursement due will be refunded to the policyholder.
Please check one of the following reimbursement request reasons: |
Fax to: |
|
|
||
Member did not have the Catamaran prescription drug card with them |
Mail to: |
|
Member did not receive the Catamaran prescription drug card before the time of purchase |
||
Catamaran |
||
Vacation supply |
||
|
||
Claim was rejected at the pharmacy |
Direct Member Reimbursement |
|
Claim consideration for Coordination of Benefits (secondary coverage) |
P.O. Box 1069 |
|
Rockville, MD |
||
Other; please attach a detailed explanation to be considered for reimbursement |
|
|
|
Any person who knowingly and willfully presents a false or fraudulent claim for payment for a loss or benefit or who knowingly and willfully
presents false information in an application for insurance is guilty of a crime and may be subject to fines and confinement in prison.
4/11