The idea driving our PDF editor was to make it as intuitive as possible. The whole procedure of filling out ch 205 effortless in case you adhere to all of these actions.
Step 1: Click on the button "Get Form Here".
Step 2: The form editing page is currently open. Include information or manage existing details.
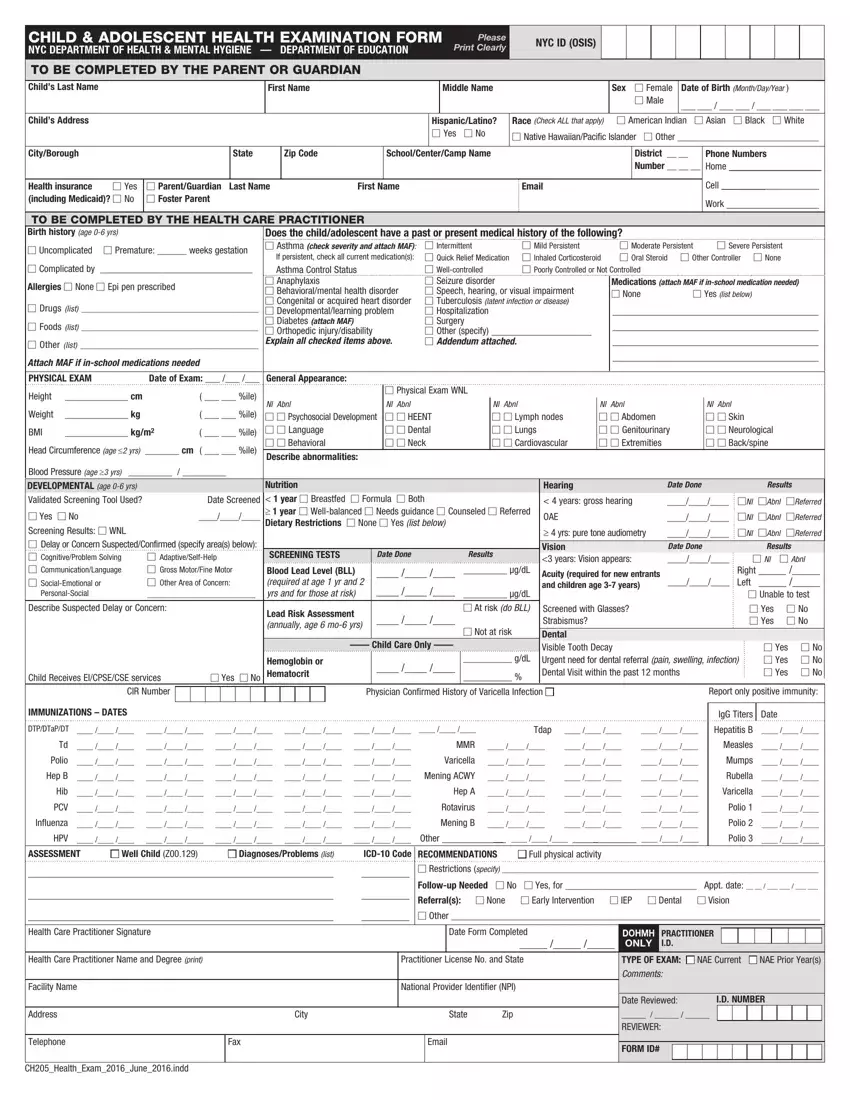
Create the ch 205 PDF and enter the material for each and every segment:
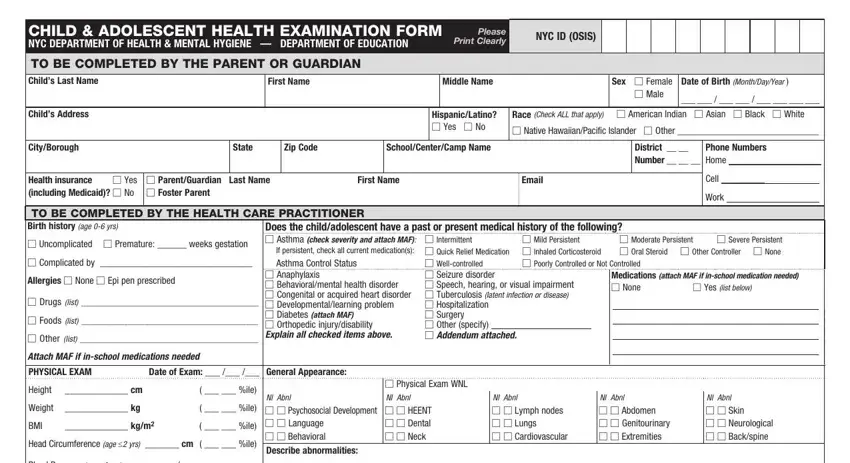
Fill in the Blood Pressure age yrs, Date Screened, M Yes M No Screening Results M WNL, M AdaptiveSelfHelp M Gross, Nutrition year M Breastfed M, SCREENING TESTS, Date Done, Results, Blood Lead Level BLL required at, gdL, Hearing, Date Done, Results, years gross hearing, and MNl MAbnl MReferred field using the data requested by the application.
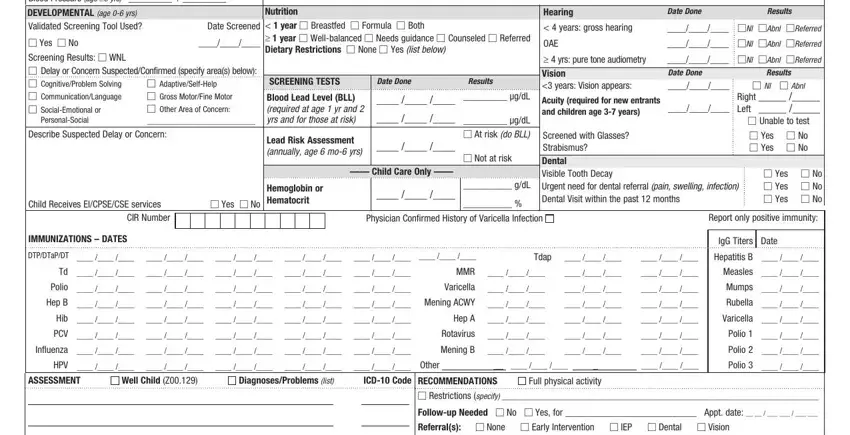
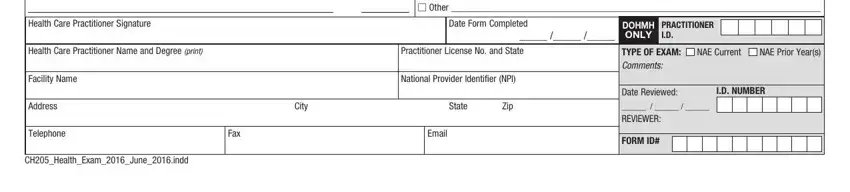
You can be asked to write down the data to let the application fill out the segment Health Care Practitioner Signature, M Other, Date Form Completed, DOHMH ONLY, PRACTITIONER ID, Health Care Practitioner Name and, Practitioner License No and State, Facility Name, Address, Telephone, National Provider Identifier NPI, City, State, Zip, and Fax.
Step 3: Hit "Done". It's now possible to export the PDF file.
Step 4: It may be more convenient to create duplicates of your file. You can rest assured that we won't reveal or read your particulars.