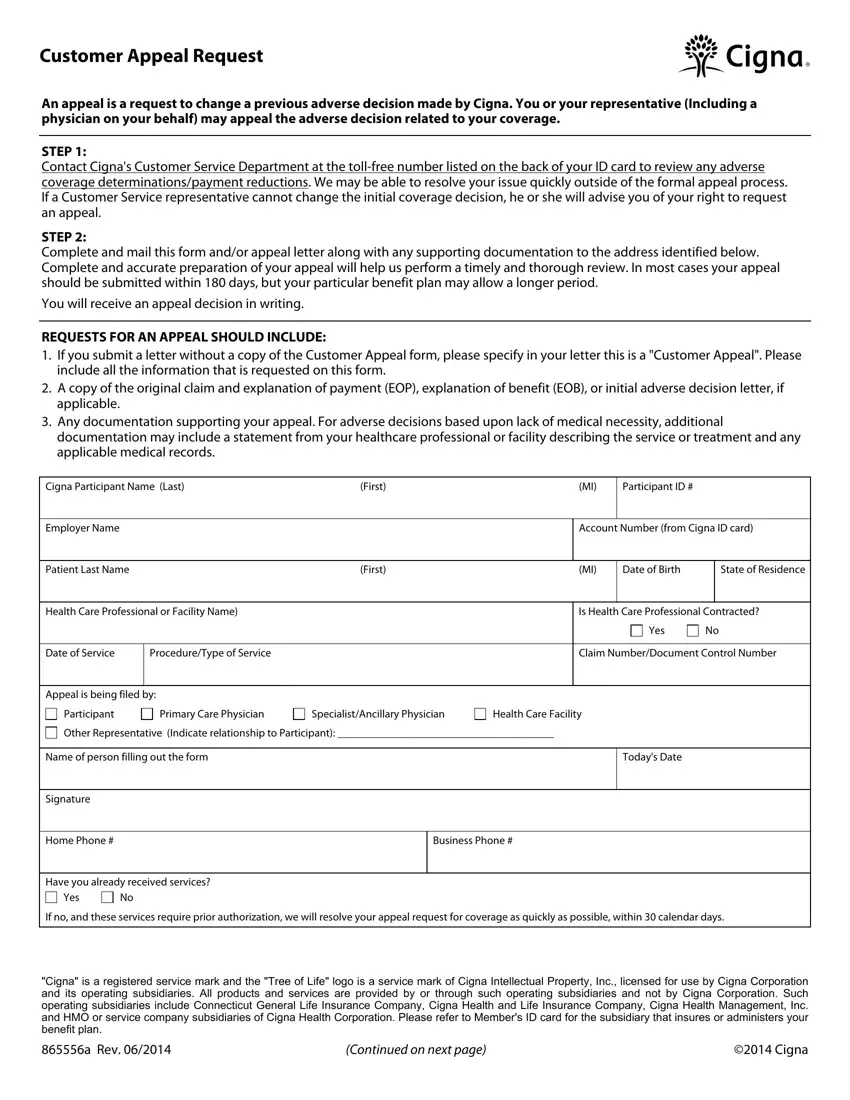
It is a breeze to complete the cignas provider appeal form. Our software was meant to be easy-to-use and assist you to fill in any PDF easily. These are the basic steps to follow:
Step 1: The first thing would be to choose the orange "Get Form Now" button.
Step 2: At this point, you are on the file editing page. You can add content, edit current information, highlight certain words or phrases, insert crosses or checks, insert images, sign the template, erase unwanted fields, etc.
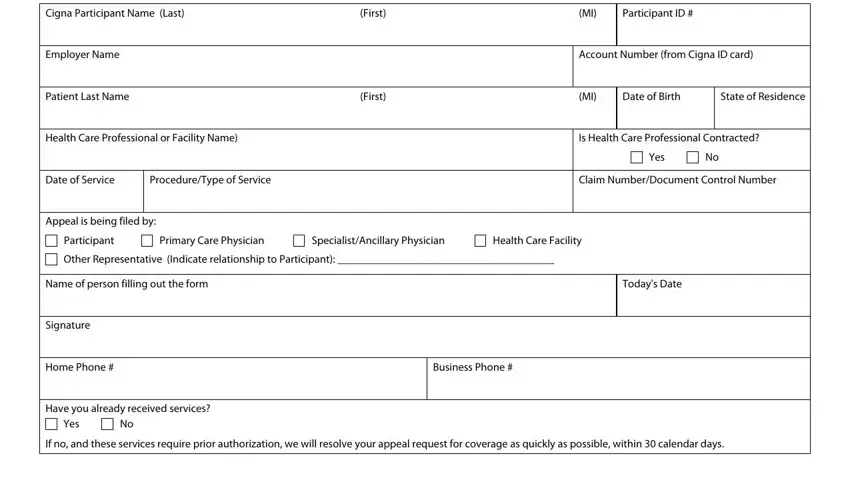
The following segments are in the PDF document you'll be completing.
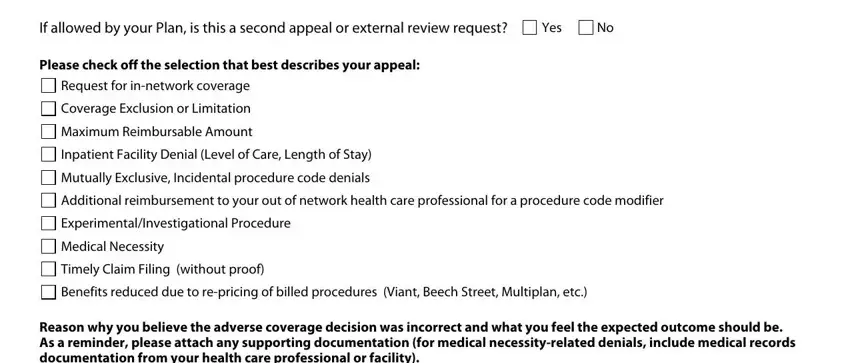
Please type in the crucial information in the If allowed by your Plan is this a, Yes, Please check off the selection, Request for innetwork coverage, Coverage Exclusion or Limitation, Maximum Reimbursable Amount, Inpatient Facility Denial Level of, Mutually Exclusive Incidental, Additional reimbursement to your, ExperimentalInvestigational, Medical Necessity, Timely Claim Filing without proof, Benefits reduced due to repricing, and Reason why you believe the adverse area.
In the area dealing with Reason why you believe the adverse, and Additional Comments, you should write down some necessary data.
The a Rev section allows you to indicate the rights and obligations of both parties.

Step 3: Hit the button "Done". The PDF form can be transferred. It's possible to upload it to your device or send it by email.
Step 4: You can generate duplicates of your file tokeep away from different forthcoming troubles. You need not worry, we do not share or track your data.


 Request for
Request for 
 Coverage Exclusion or Limitation
Coverage Exclusion or Limitation
 Maximum Reimbursable Amount
Maximum Reimbursable Amount
 Inpatient Facility Denial (Level of Care, Length of Stay)
Inpatient Facility Denial (Level of Care, Length of Stay)
 Mutually Exclusive, Incidental procedure code denials
Mutually Exclusive, Incidental procedure code denials
 Additional reimbursement to your out of network health care professional for a procedure code modifier
Additional reimbursement to your out of network health care professional for a procedure code modifier
 Experimental/Investigational Procedure
Experimental/Investigational Procedure
 Medical Necessity
Medical Necessity
 Timely Claim Filing (without proof)
Timely Claim Filing (without proof)
 Benefits reduced due to
Benefits reduced due to 