In the realm of workers' compensation in Florida, the DFS F5 DWC 25 form stands as a pivotal document, designed to streamline communication between healthcare providers, insurers, and employers regarding the medical treatment and status of injured employees. This comprehensive form, officially titled Florida Workers' Compensation Uniform Medical Treatment/Status Reporting Form, serves multiple critical functions. It captures the insurer's details, the dates of medical visits or reviews, and the injured employee’s personal and accident-related information. Health care providers are required to complete this form with legible accuracy, ensuring that their responses are confined to their areas of expertise. The form encompasses several sections, including clinical assessments/determinations on the work-relatedness of the injury, objective relevant medical findings, major contributing cause of the condition, and the patient's classification level based on the severity and nature of their condition. Furthermore, it outlines a management or treatment plan, delineates any functional limitations or restrictions, and, when applicable, establishes the date of maximum medical improvement and assigns a permanent impairment rating. The instructions for completing the DFS F5 DWC 25 form emphasize its role in the authorization of treatment services, making it an indispensable tool in the administration of workers' compensation claims in Florida. As such, it embodies a comprehensive approach to documenting and managing the care of injured workers, ensuring their treatment is accurately reflected and communicated to all pertinent parties.
| Question | Answer |
|---|---|
| Form Name | Dfs F5 Dwc 25 Form |
| Form Length | 18 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 4 min 30 sec |
| Other names | f5dwc, dwc25, dwc 25 form 2021, dwc 25 form florida |
Florida Workers' Compensation Uniform Medical Treatment/Status Reporting Form - PAGE 1
BEFORE COMPLETING THIS FORM, PLEASE CAREFULLY REVIEW THE INSTRUCTIONS BEGINNING ON PAGE 3
NOTE: Health care providers shall legibly and accurately complete all sections of this form, limiting their responses to their area of expertise.
1. |
Insurer Name: |
|
|
2. |
Visit/Review Date: |
5. |
FOR INSURER USE ONLY |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
3. |
Injured Employee (Patient) Name: |
|
|
4. |
Date of Birth: |
5. Social Security #: |
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
6. |
Date of Accident: |
|
|
7. |
Employer Name |
8. |
Initial visit with this physician? |
||||
|
|
|
|
|
|
|
|
|
|
a) NO |
b) YES |
|
|
SECTION I |
CLINICAL ASSESSMENT / DETERMINATIONS |
|
|
||||||||
9. No change in Items 9 - 13d since last reported visit. If checked, GO TO SECTION II.
10.Injury/ Illness for which treatment is sought is:
a) NOT WORK RELATED |
b) WORK RELATED |
c) UNDETERMINED as of this date |
11.Has the patient been determined to have Objective Relevant Medical Findings? Pain or abnormal anatomical findings, in the absence of objective relevant medical findings, shall not be an indicator of injury and/or illness and are not compensable.
a) NO |
b) YES |
c) UNDETERMINED as of this date |
If YES or UNDETERMINED, explain: |
|
|
|
|
|
12.Diagnosis(es):
13.Major Contributing Cause: When there is more than one contributing cause, the reported
a) Is there a
a1) NO a2) YES a3) UNDETERMINED as of this date b) Do the objective relevant medical findings identified in Item 11 represent an exacerbation (temporary worsening)
or aggravation |
(progression) of a |
|
|
b1) NO |
b2) exacerbation |
b3) aggravation |
b4) UNDETERMINED as of this date |
c) Are there other relevant |
|||
c1) NO |
c2) YES |
|
|
d) Given your responses to the Items above, is the injury/illness in question the major contributing cause for: |
|||
d1) NO |
d2) YES |
the reported medical condition? |
|
d3) NO |
d4) YES |
the treatment recommended (management/treatment plan)? |
|
d5) NO |
d6) YES |
the functional limitations and restrictions determined? |
|
SECTION II |
PATIENT CLASSIFICATION LEVEL |
|
|
14. LEVEL I - Key issue: specific,
15. LEVEL II - Key issue: regional or generalized deconditioning (i.e. deficits in strength, flexibility, endurance, and motor control. Treatment: physical reconditioning and functional restoration.
16. LEVEL III
17. LEVEL UNDETERMINED AS OF THIS DATE.
SECTION III |
MANAGEMENT / TREATMENT PLAN |
||||
|
18. |
No clinical services indicated at this time. |
If checked, GO TO SECTION IV |
||
|
19. |
No change in Items 20a - 20g since last report submitted. |
If checked, GO TO SECTION IV |
||
20.The following proposed, subsequent clinical service(s) is/are deemed medically necessary.
***THIS IS A PROVIDER'S WRITTEN REQUEST FOR INSURER AUTHORIZATION OF TREATMENT OR SERVICES. ***
a) Consultation with or referral to a specialist. |
|
|
||||||
Identify principal physician: |
|
|
||||||
Identify specialty & provide rationale: |
|
|
|
|
|
|
||
a1) CONSULT ONLY |
|
a2) |
|
|
|
|
|
|
REFERRAL & |
a3) TRANSFER CARE |
|
||||||
b) Diagnostic Testing: (Specify)
c) Physical Medicine. Check appropriate box and indicate specificity of services, frequency and duration below:
c1) Physical/Occupational therapy, Chiropractic, Osteopathic or comparable physical rehabilitation.
c2) Physical Reconditioning (Level II Patient Classification)
c3) Interdisciplinary Rehabilitation Program (Level III Patient Classification)
Specific instruction(s):
d) Pharmaceutical(s) (specify):
e) DME or Medical Supplies:
f) Surgical Intervention - specify procedure(s):
f1)
f2) Surgical Facility:
f3) Injectable(s) (e.g. pain management):
g) Attendant Care:
Form |
Page 1 of 2 |
Florida Workers' Compensation Uniform Medical Treatment/Status Reporting Form - PAGE 2
Patient Name: |
|
D/A: |
|
VISIt/Review Date: |
|
|
|
|
|
|
|
|
|
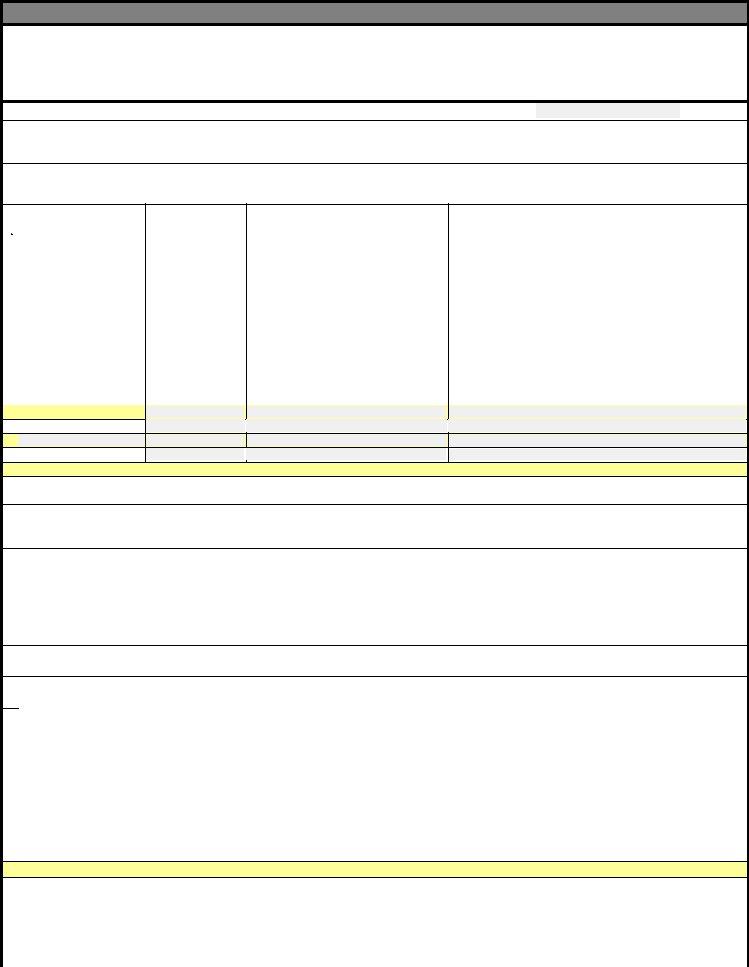
SECTION IV |
FUNCTIONAL LIMITATIONS AND RESTRICTIONS |
|||||
Assignment of limitations or restrictions must be based upon the injured employee's specific clinical
dysfunction or status related to the work injury. However, the presence of objective relevant medical findings
does not necessarily equate to an automatic limitation or restriction in function.
21 No functional limitations identified or restrictions prescribed as of the following date: _________________.
22. The injured workers' functional limitations and restrictions, identified in detail below, are of such severity that he/she
cannot perform activities, even at a sedentary level (e.g. hospitalization, cognitive impairment, infection, contagion),
as of the following date: ___________________. |
Use additional sheet if needed. |
23. The injured worker may return to activities so long as he/she adheres to the functional limitations and restrictions identified below. Identify ONLY those functional activities that have specific limitations and restrictions for this patient. Identify joint and/or body part __________________________________. Use additional sheet if needed.
Functional Activity |
Load |
|
Frequency & Duration |
|
|
ROM/ Position & Other Parameters |
||
Bend |
|
|
|
|
|
|
|
|
Carry |
|
|
|
|
|
|
|
|
Climb |
|
|
|
|
|
|
|
|
Grasp |
|
|
|
|
|
|
|
|
Kneel |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Pull |
|
|
|
|
|
|
|
|
Push |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Sit |
|
|
|
|
|
|
|
|
Squat |
|
|
|
|
|
|
|
|
Stand |
|
|
|
|
|
|
|
|
Twist |
|
|
|
|
|
|
|
|
Walk
_
Other
COMMENTS:
Other choices; Skin Contact/ Exposure; Sensory; Hand Dexterity; Cognitive; Crawl; Vision; Drive/Operate Heavy Equipment; Environmental Conditions: heat, cold, working at heights, vibration; Auditory; Specific Job Task(s); etc.
NOTE: Any functional limitations or restrictions assigned above apply to both on and off the job activities, and are in effect until the next scheduled appointment unless otherwise noted or modified prior to the appointment date.
Specify those functional limitations and restrictions, in Item 23, which are permanent if MMI / PIR have been assigned in Item 24.
SECTION V |
MAXIMUM MEDICAL IMPROVEMENT / PERMANENT IMPAIRMENT RATING |
|
|
|
|||||||||||
24. |
Patient has achieved maximum medical improvement? |
|
|
|
|
|
|
|
|||||||
|
a) YES, Date: |
|
|
|
b) NO |
c) Anticipated MMI date: |
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|||||||
|
d) Anticipated MMI date cannot be determined at this time. |
Future Medical Care Anticipated: e) Yes |
f) No |
||||||||||||
|
|
Comments: |
|
__________________________________________________________________________________ |
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
25. |
|
_____ |
% Permanent Impairment Rating (body as a whole) |
Body part/system: |
_____________________________ |
|
|||||||||
26.Guide used for calculation of Permanent Impairment Rating (based on date of accident - see instructions):
a) 1996 FL Uniform PIR Schedule |
b) Other, specify |
|
______________________________________________ |
||
|
27.Is a residual clinical dysfunction or residual functional loss anticipated for the
b) NO c) Undetermined at this time. a) YES
SECTION VI |
|||
28. Next Scheduled Appointment Date & Time: |
________________________________ |
|
|
SECTION VII |
ATTESTATION STATEMENT |
||
“As the Physician, I hereby attest that all responses herein have been made, in accordance with the instructions as part of this form, to a reasonable degree of medical certainty based on objective relevant medical findings, are consistent with my medical documentation
regarding this patient, and have been shared with the patient." |
"I certify to any MMI / PIR information provided in this form.” |
||||||||||||
Physician Group: |
|
|
Date: |
|
|
|
|
|
|||||
Physician Signature: |
|
Physician DOH License #: |
|
|
|||||||||
Physician Name: |
|
|
|
|
|
Physician Specialty: |
|
|
|
|
|
||
|
|
|
|||||||||||
|
|
|
|
|
(print name) |
|
|
|
|
|
|
|
|
If any direct billable services for this visit were rendered by a provider other than a physician, please complete sections below:
“I hereby attest that all responses herein relating to services I rendered have been made, in accordance with the instructions as part of this form, to a reasonable degree of medical certainty based on objective relevant medical findings, are consistent with my medical documentation regarding this patient, and have been shared with the patient."
Provider Signature: |
|
|
Provider DOH License #: |
|
|
|
|
|||
Provider Name: |
|
|
Date: |
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(print name) |
|
|
|
|
|
|
Form |
|
|
|
|
Page 2 of 2 |
|
||||
FORM
COMPLETION/SUBMISSION INSTRUCTIONS
GENERAL INFORMATION
The Form
Insurers/employers and providers shall utilize only the Form
Accurate completion of the Form
No reimbursement shall be made for completion of the Form
a. Evaluating an injury or illness,
Form |
3 |
|
Revised 01/31/2008 |
||
|
b.Ordering, prescribing or rendering remedial treatment care or attendance, and
c.Assigning functional limitations or restrictions.
COMPLETION GUIDELINES
Physicians completing the Form
•Accurate completion and submission of the Form
•Accurate completion and submission of the Form
•The Form
•Physician notes, medical records, or other relevant diagnostic tests and evaluations must be consistent with all information submitted on the Form
•A copy of the Form
•Physicians shall provide a copy of the accurately completed Form
COMPLETION REQUIREMENTS
Providers required to complete the Form
•All physicians, including physician assistants and advanced registered nurse practitioners (ARNPs) under the supervision of a physician, who provide direct billable services immediately following the reported work related injury, regardless of location.
•Physicians providing preliminary treatment, care or attendance in the emergency room of a hospital licensed under Chapter 395, F.S. shall be required to accurately complete Items
Form |
4 |
|
Revised 01/31/2008 |
||
|
•All principal physicians or physicians accepting consults, referrals or transfers of care (including physician assistants and ARNPs under the supervision of a physician) who provide initial or ongoing treatment, care or independent medical examinations.
COMPLETION EXEMPTIONS
Providers exempt from completing the
•Physicians providing only medical interpretation of diagnostic testing (i.e. radiographic films; lab specimens;
•Physicians performing diagnostic testing (i.e.
•Anesthesiologists or ARNPs, under the supervision of a physician, who provide anesthesia services in the presence of an operating surgeon.
•Physicians functioning as a second surgeon or as an assistant surgeon and not as the primary surgeon.
COMPLETION/ SUBMISSION EXCEPTIONS
Physicians providing treatment when the patient is admitted to hospital for greater than 24 hours shall:
complete the Form
on the date of admission for unscheduled hospitalizations, and upon the date of discharge.
When Form
•Physicians providing treatment when the patient is participating in an interdisciplinary pain
management program, interdisciplinary rehabilitation program or receiving more than three times
Form |
5 |
|
Revised 01/31/2008 |
||
|