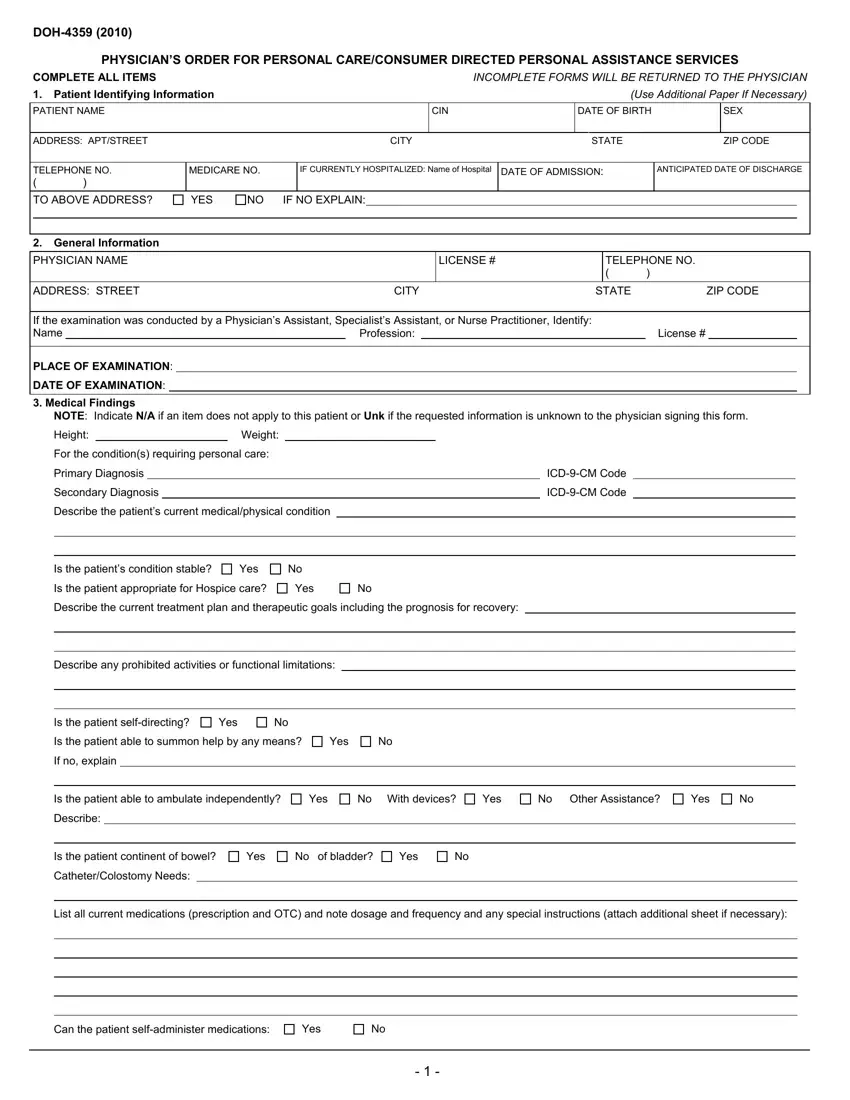
DOH-4359 (2010)
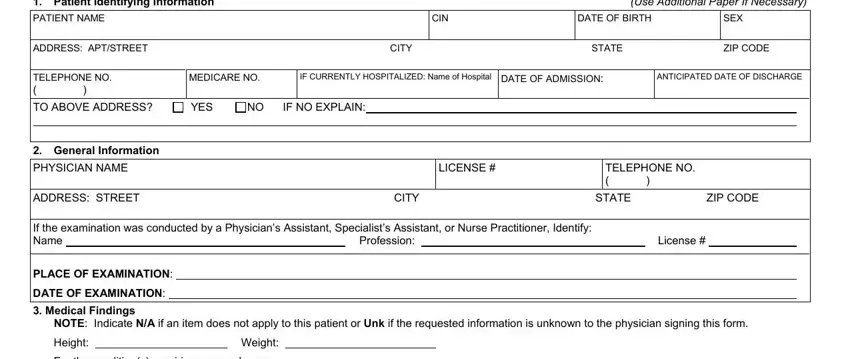
PHYSICIAN’S ORDER FOR PERSONAL CARE/CONSUMER DIRECTED PERSONAL ASSISTANCE SERVICES
COMPLETE ALL ITEMS |
|
|
|
|
|
|
|
|
|
|
INCOMPLETE FORMS WILL BE RETURNED TO THE PHYSICIAN |
1. |
Patient Identifying Information |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(Use Additional Paper If Necessary) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PATIENT NAME |
|
|
|
|
|
|
|
|
|
CIN |
|
|
|
DATE OF BIRTH |
|
|
SEX |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ADDRESS: APT/STREET |
|
|
|
|
|
|
|
CITY |
|
|
|
STATE |
|
|
|
|
|
ZIP CODE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TELEPHONE NO. |
MEDICARE NO. |
|
|
IF CURRENTLY HOSPITALIZED: Name of Hospital |
DATE OF ADMISSION: |
|
|
|
ANTICIPATED DATE OF DISCHARGE |
( |
) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TO ABOVE ADDRESS? |
YES |
NO |
IF NO EXPLAIN: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2. |
General Information |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PHYSICIAN NAME |
|
|
|
|
|
|
|
|
|
|
LICENSE # |
|
|
|
|
TELEPHONE NO. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
( |
) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ADDRESS: STREET |
|
|
|
|
|
|
|
CITY |
|
|
|
STATE |
ZIP CODE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
If the examination was conducted by a Physician’s Assistant, Specialist’s Assistant, or Nurse Practitioner, Identify: |
|
|
|
|
|
|
|
|
Name |
|
|
|
|
|
|
|
Profession: |
|
|
|
|
|
|
|
|
|
License # |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PLACE OF EXAMINATION: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
DATE OF EXAMINATION: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3. Medical Findings |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NOTE: Indicate N/A if an item does not apply to this patient or Unk if the requested information is unknown to the physician signing this form. |
|
|
Height: |
|
|
Weight: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
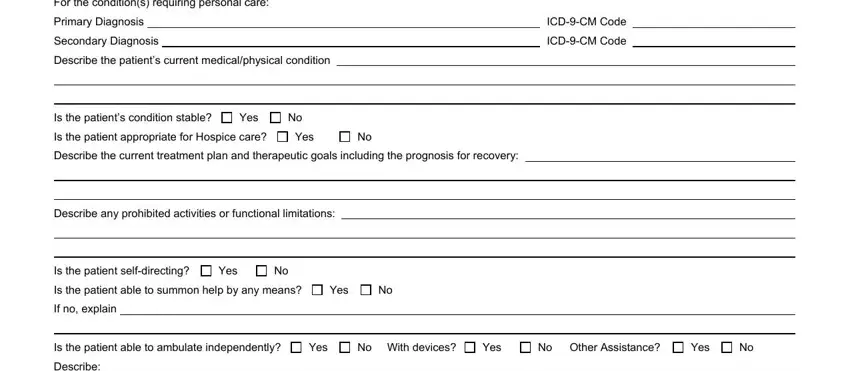
For the condition(s) requiring personal care: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Primary Diagnosis |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ICD-9-CM Code |
|
|
|
|
|
|
|
|
|
|
Secondary Diagnosis |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ICD-9-CM Code |
|
|
|
|
|
|
|
|
|
|
Describe the patient’s current medical/physical condition |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Is the patient’s condition stable? |
Yes |
|
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Is the patient appropriate for Hospice care? |
|
Yes |
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Describe the current treatment plan and therapeutic goals including the prognosis for recovery: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Describe any prohibited activities or functional limitations:
Is the patient self-directing? |
Yes |
No |
Is the patient able to summon help by any means? If no, explain
Is the patient able to ambulate independently? Describe:
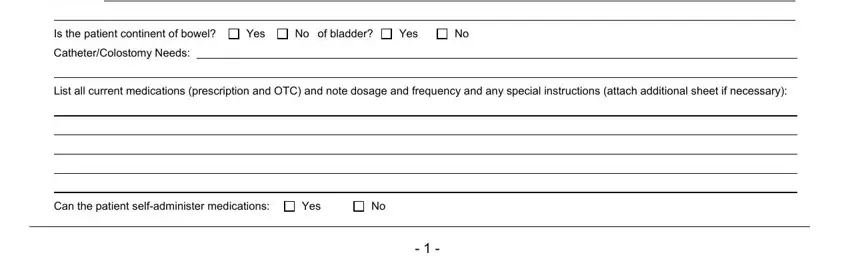
Is the patient continent of bowel? Catheter/Colostomy Needs:
List all current medications (prescription and OTC) and note dosage and frequency and any special instructions (attach additional sheet if necessary):
Can the patient self-administer medications:
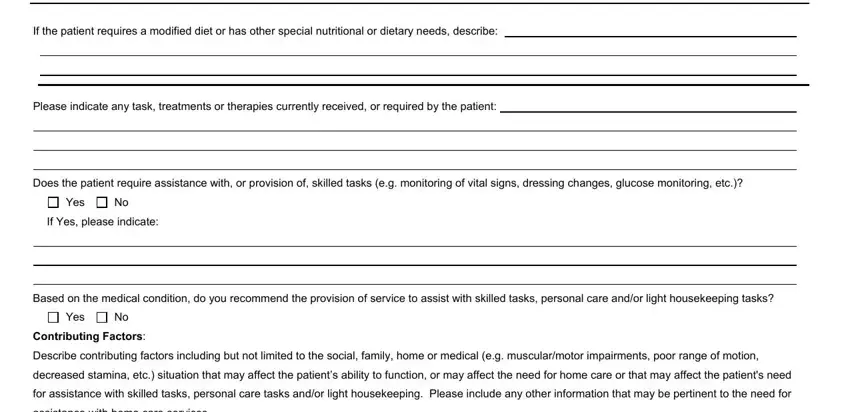
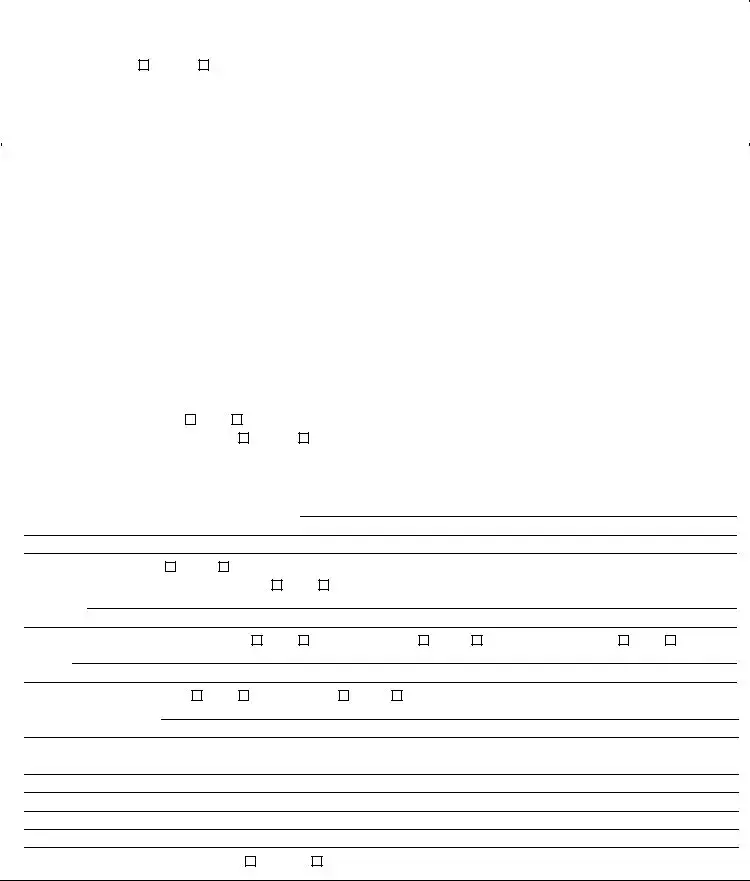
If the patient requires a modified diet or has other special nutritional or dietary needs, describe:
Please indicate any task, treatments or therapies currently received, or required by the patient:
Does the patient require assistance with, or provision of, skilled tasks (e.g. monitoring of vital signs, dressing changes, glucose monitoring, etc.)?
If Yes, please indicate:
Based on the medical condition, do you recommend the provision of service to assist with skilled tasks, personal care and/or light housekeeping tasks?
Contributing Factors:
Describe contributing factors including but not limited to the social, family, home or medical (e.g. muscular/motor impairments, poor range of motion,
decreased stamina, etc.) situation that may affect the patient’s ability to function, or may affect the need for home care or that may affect the patient's need
for assistance with skilled tasks, personal care tasks and/or light housekeeping. Please include any other information that may be pertinent to the need for
assistance with home care services.
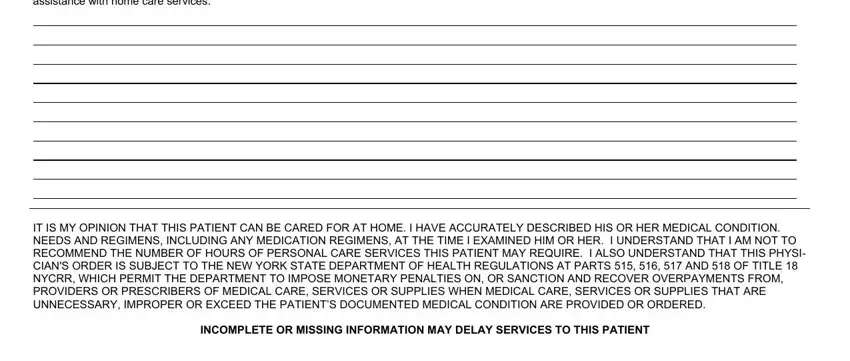
IT IS MY OPINION THAT THIS PATIENT CAN BE CARED FOR AT HOME. I HAVE ACCURATELY DESCRIBED HIS OR HER MEDICAL CONDITION. NEEDS AND REGIMENS, INCLUDING ANY MEDICATION REGIMENS, AT THE TIME I EXAMINED HIM OR HER. I UNDERSTAND THAT I AM NOT TO RECOMMEND THE NUMBER OF HOURS OF PERSONAL CARE SERVICES THIS PATIENT MAY REQUIRE. I ALSO UNDERSTAND THAT THIS PHYSI- CIAN'S ORDER IS SUBJECT TO THE NEW YORK STATE DEPARTMENT OF HEALTH REGULATIONS AT PARTS 515, 516, 517 AND 518 OF TITLE 18 NYCRR, WHICH PERMIT THE DEPARTMENT TO IMPOSE MONETARY PENALTIES ON, OR SANCTION AND RECOVER OVERPAYMENTS FROM, PROVIDERS OR PRESCRIBERS OF MEDICAL CARE, SERVICES OR SUPPLIES WHEN MEDICAL CARE, SERVICES OR SUPPLIES THAT ARE UNNECESSARY, IMPROPER OR EXCEED THE PATIENT’S DOCUMENTED MEDICAL CONDITION ARE PROVIDED OR ORDERED.
INCOMPLETE OR MISSING INFORMATION MAY DELAY SERVICES TO THIS PATIENT
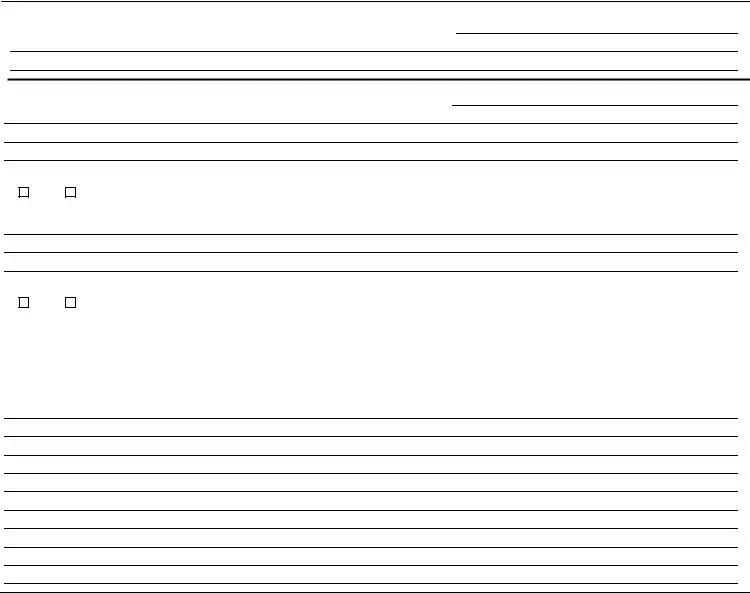
Physician’s Signature _________________________________________________________________ Date _________________________
PLEASE SIGN AND RETURN COMPLETED FORM WITHIN 30 CALENDAR DAYS OF EXAMINATION TO:
___________________________________________________________________________
___________________________________________________________________________
___________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
New York State Department of Health
- 2 -
PHYSICIAN’S ORDER FOR PERSONAL CARE/CONSUMER DIRECTED PERSONAL ASSISTANCE SERVICES
INSTRUCTIONS
COMPLETE ALL ITEMS. (Attach additional sheets, if necessary). INCOMPLETE FORMS WILL BE RETURNED TO THE PHYSICIAN.
INCOMPLETE OR MISSING INFORMATION MAY DELAY SERVICES TO THIS PATIENT.
1.Patient Identifying Information
•Patient Name. Enter the patient’s name.
•CIN. Found on the patient’s Medical Assistance ID card.
•Date of Birth. Enter the patient’s date of birth.
•Sex. Enter the patient’s gender.
•Address and telephone number. Enter the patient’s address and telephone number.
•Medicare #. Enter the patient’s Medicare number if available.
•If currently hospitalized. If the patient is hospitalized at the time of completion of the physician's order, indicate the name of the hospital, date of admission, and anticipated date of discharge.
•Discharge to above address. If the patient is to be discharged to an address other than the address listed above please explain.
•General Information
Physician’s Name, License #, Address, Telephone. Enter information for the physician signing the order. Enter either the physician’s license number as issued by the New York State Department of Education or the provider billing number issued by the New York State Department of Health Medicaid Management Information System.
•Examination conducted by other than a physician. If patient was examined, and the order form completed by a physician’s assistant, specialist’s assistant, or nurse practitioner, complete the required information.
•Place of Examination. Indicate the location (office, clinic, home, etc) of the examination of the patient.
•Date of Examination. Enter the date the patient was examined. This must be within 30 days of the date the physician signed the form.
3.Medical Findings
Note: Indicate N/A if an item does not apply to this patient or Unk if the requested information is unknown to the physician signing this form.
•Height, Weight. Enter the patient’s height and weight.
•Primary and Secondary Diagnosis. Enter the primary and secondary diagnosis with ICD-9-CM codes for the primary and secondary conditions which result in the patient being evaluated for home care services.
•Describes the current condition. Describe the patient’s current medical/physical condition, including any relevant history.
•Stability. Check Yes if the patient’s condition is not expected to show marked deterioration or improvement. A stable medical condition shall be defined as follows:
(a)the condition is not expected to exhibit sudden deterioration or improvement; and
(b)the condition does not require frequent medical or nursing judgment to determine changes in the patient's plan of care; and
(c)(1) the condition is such that a physically disabled individual is in need of routine supportive assistance and does not need skilled professional care in the home; or
(2)the condition is such that a physically disabled or frail elderly individual does not need professional care but does require assistance in the home to prevent a health or safety crisis from developing.
•Hospice. If the patient’s condition is terminal, indicate if the patient is appropriate for Hospice services.
•Describe the current treatment plan. Include therapeutic goals and prognosis for recovery and anticipated duration of the current treatment plan.
•Limitations. Indicate any functional limitations or prohibited activities.
•Self-Directing. Indicate if the patient is self-directing. Self-directing means that the patient is capable of making choices about activities of daily living, understanding the impact of the choices, and assuming responsibility for the results of the choices. A No response to this item should be reflected in the description of the patient’s condition as documented in the applicable section.
•Able to Summon Help. Check Yes if the patient is able to summon assistance in an emergency situation by any means. If the patient is not able to summon assistance, check No and explain.
-3 -
•Ambulation. Indicate the patient’s ability to ambulate independently, or with the need for assistance or devices. Specify assistance/devices used or needed.
•Bowel/Bladder. Indicate if the patient is continent. Describe any catheter or colostomy needs.
•Medications Required. List all prescription and over-the-counter medications the patient is taking and note dosage, frequency and any special instructions.
•Medication Administration. Indicate the patient’s ability to self-administer medications.
•Dietary Needs. Indicate if the patient has special nutritional or dietary needs, i.e. low salt or high potassium.
•Tasks/Treatments/Therapies. Indicate any tasks, treatments or therapies which the patient receives or requires in the home and describe.
•Need for completion/assistance with skilled tasks. If the patient requires assistance with skilled tasks including, but not limited to, glucose monitoring, wound care, vital signs, describe the need for such assistance.
•Recommendation to provide assistance. Check Yes if, in your opinion, the patient can be maintained in his or her home with provision of home care services.
•Contributing factors to need for assistance. Please indicate the functional deficits that support the need for the provision of home care services. Please include any pertinent information you may have regarding the patient’s surroundings, physical condition or other factors that may affect the ability of the patient to function in the community or the patient’s need for assistance with personal care tasks.
4.Physician’s Signature/Date of completion. The signature of the ordering physician as identified in Item 2. Note that by signing this document, the physician certifies that the patient’s condition and needs are accurately described. Forms lacking a signature and/or date are not acceptable.
5.Return Form To. The local district or other case management entity to whom the form is to be returned.
- 4 -