Understanding the DSS 486T form is essential for providers and patients navigating the intricate world of Disability Medicaid in New York State. This comprehensive document, a critical piece of the application process for determining disability, requires meticulous completion by healthcare providers. With its primary goal to capture an applicant's current medical condition, the form serves as a bridge between the medical assessment and the eligibility for benefits. It demands detailed information ranging from diagnostics, medication regimens, and general medical findings to more nuanced sections that evaluate the patient's functional capacity through exertional and non-exertional functions. Physicians are tasked with not just outlining the current health status but also providing insights into the patient’s ability to perform work-related activities, thereby influencing the decision on their application. Furthermore, sections dedicated to specific systems of the body such as musculoskeletal, cardiovascular, and mental disorders require in-depth insights, ensuring a comprehensive view of the patient's condition is presented. Through this form, the interconnectedness of medical evaluation and social support systems is underscored, highlighting the importance of thorough, accurate documentation in supporting the needs of individuals seeking Disability Medicaid benefits.
| Question | Answer |
|---|---|
| Form Name | Dss 486T Form |
| Form Length | 25 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 6 min 15 sec |
| Other names | 486t medicaid, 486t medicaid forms, westchester dss forms, dss 486 |
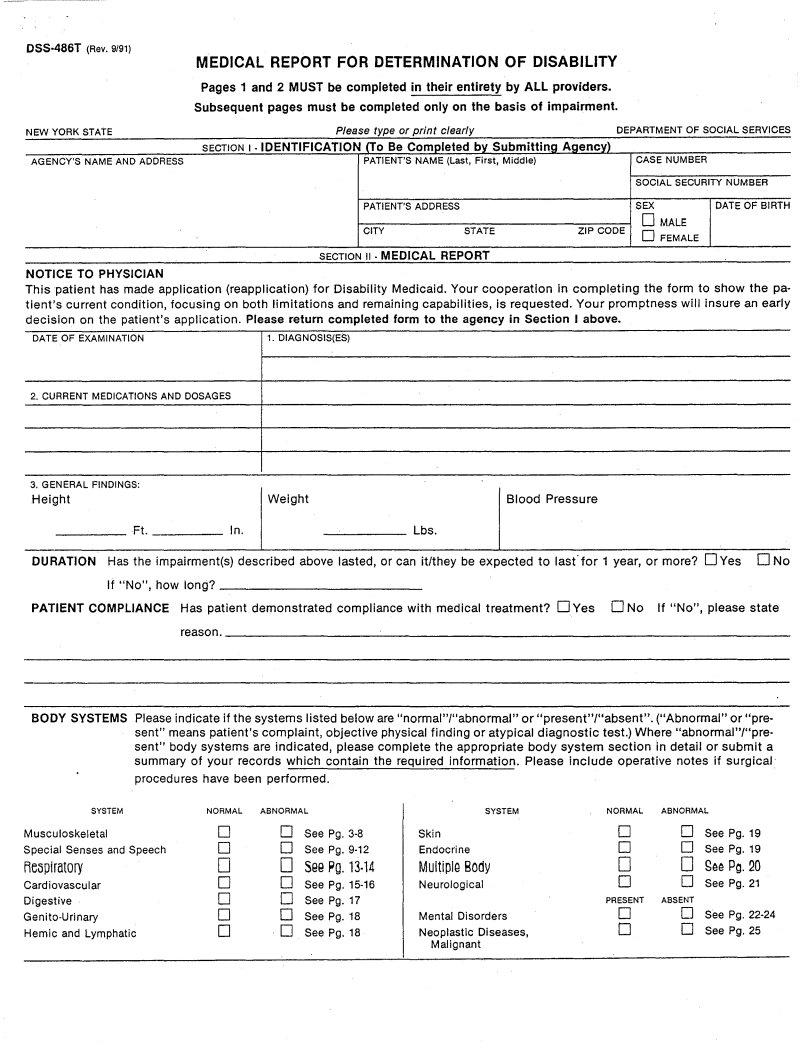
DSS·486T (Rev. 9/91)
MEDICAL REPORT FOR DETERMINATION OF DISABILITY
Pages 1 and 2 MUST be completed in their entirety by ALL providers.
Subsequent pages must be completed only on the basis of impairment.
NEW YORK STATE |
|
DEPARTMENT OF SOCIAL SERVICES |
|
|
|
|
|
AGENCY'S NAME AND ADDRESS |
|
CASE NUMBER |
|
|
|
SOCIAL SECURITY NUMBER |
|
PATIENT'S ADDRESS |
|
SEX |
DATE OF BIRTH |
|
|
D MALE |
|
CITY |
STATE |
ZIP CODE D FEMALE |
|
SECTION II • MEDICAL REPORT
NOTICE TO PHYSICIAN
This patient has made application (reapplication) for Disability Medicaid. Your cooperation in completing the form to show the pa- tient's current condition, focusing on both limitations and remaining capabilities, is requested. Your promptness will insure an early decision on the patient's application. Please return completed form to the agency in Section I above.
DATE OF EXAMINATION |
1. DIAGNOSIS(ES) |
2. CURRENT MEDICATIONS AND DOSAGES |
|
3. GENERAL FINDINGS:
HeightFt. |
|
'". |
[weight |
Lbs. |
[ Blood Pressure |
DURATION Has the impairment(s) described above lasted, or can it/they be expected to last"for 1 year, or more? DYes D No
If "No", how long? |
_ |
PATIENT COMPLIANCE Has patient demonstrated |
compliance with medical treatment? DYes D No If "No", please state |
reason. |
_ |
BODY SYSTEMS Pleaseindicate if the systems listed below are "normal"I"abnormal" or "present"/"absent". ("Abnormal" or "pre- sent" means patient's complaint, objective physical finding or atypical diagnostic test.) Where "abnormal"I"pre- sent" body systems are indicated, please complete the appropriate body system section in detail or submit a summary of your records which contain the required information. Please include operative notes if surgical
procedures have been performed.
SYSTEM |
NORMAL |
ABNORMAL |
|
SYSTEM |
NORMAL |
ABNORMAL |
|
Musculoskeletal |
D |
D |
See |
Skin |
0 |
D |
SeePg.19 |
SpecialSensesandSpeech |
D |
0 |
Endocrine |
0 |
0 SeePg. 19 |
||
Re\ipiratory |
0 |
0 |
5BB Pg. 13·14 |
MultiplQ Body |
0 |
0 gaa Pg. 20 |
|
Cardiovascular |
D |
D |
Neurological |
0 |
D |
SeePg.21 |
|
Digestive |
D |
D |
SeePg.17 |
|
PRESENT |
ABSENT |
|
D |
D |
SeePg. 18 |
MentalDisorders |
|
Hemic and Lymphatic |
D |
D |
SeePg.18 |
NeoplasticDiseases, |
|
|
|
|
Malignant |
00
0D SeePg.25
DSS.486T |
(Rev. 9/91) |
|
|
|
|
|
|
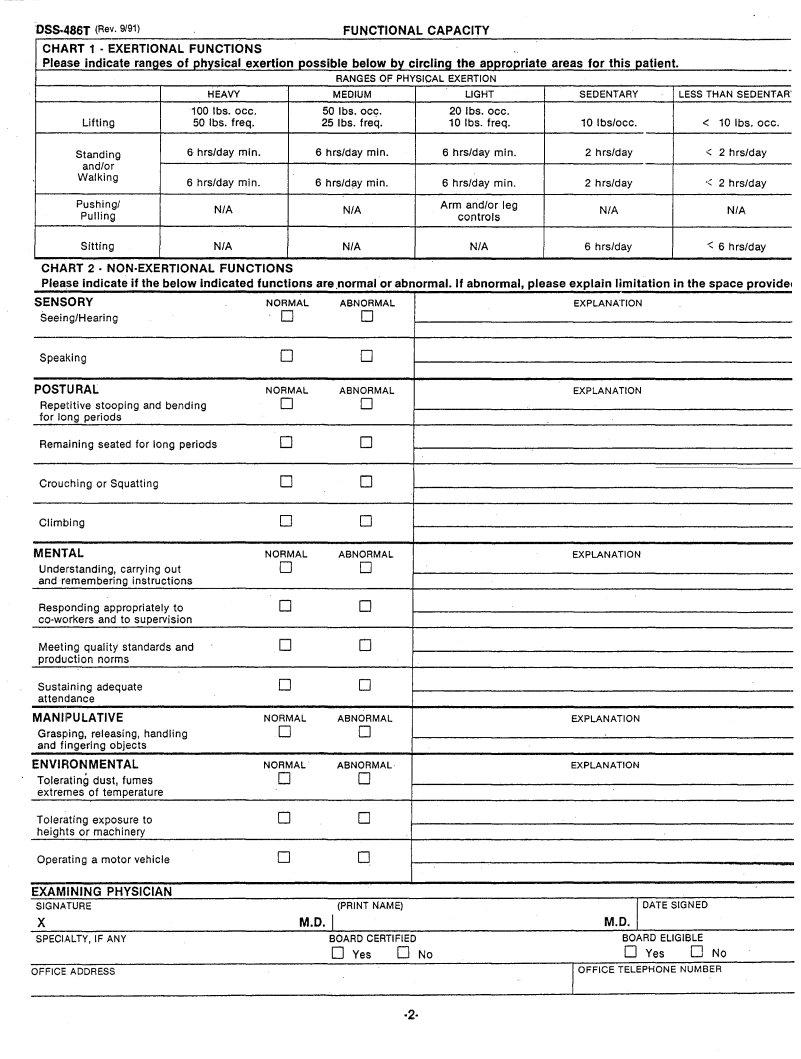
FUNCTIONAL CAPACITY |
|
|
|
|
|
|
|
|
|||||||||
CHART 1 . EXERTIONAL FUNCTIONS |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
Please indicate ranges of physical exertion possible below by circling the appropriate areas for this patient. |
|
|
- |
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
RANGES OF PHYSICAL EXERTION |
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
HEAVY |
MEQIUM |
|
|
LIGHT |
SEDENTARY |
LESS THAN SEDENTAR' |
|||||||||
|
|
|
|
|
|
|
100 |
Ibs. |
occ. |
50 |
Ibs. |
occ. |
|
20 |
Ibs. |
occ. |
|
|
|
|
|
|
|
||
|
Lifting |
|
|
|
|
50 |
Ibs. |
freq. |
25 |
Ibs. |
freq. |
|
10 |
Ibs. |
freq. |
10 |
Ibs/occ. |
< |
10 Ibs. occ. |
||||||
|
Standing |
|
|
6 |
hrs/day |
min. |
6 hrs/day |
min. |
6 |
hrs/day |
min. |
2 |
hrs/day |
< |
2 |
hrs/day |
|||||||||
|
and/or |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
Walking |
|
|
6 |
hrs/day |
min. |
e hrs/d~y |
min. |
6 |
hrs/day |
min. |
2 |
hrs/day |
<: |
2 |
hrs/day |
|||||||||
|
|
|
|
|
|
|
|||||||||||||||||||
|
Pushing! |
|
|
|
|
|
N/A |
|
|
N/A |
Arm |
and/or leg |
|
N/A |
|
|
N/A |
||||||||
|
Pulling |
|
|
|
|
|
|
|
|
controls |
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
Sitting |
|
|
|
|
|
N/A |
|
|
N/A |
|
|
N/A |
|
6 |
hrs/day |
< 6 |
hrs/day |
|||||||
CHART 2 . NON·EXERTIONAL |
FUNCTIONS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
~.e |
indicate if the below indicated functions are .normal or abnormal. If abnormal, please explain limitation in the space providel |
||||||||||||||||||||||||
SENS ORY |
|
|
|
|
|
|
|
|
|
|
NORMAL |
ABNORMAL |
|
|
|
|
EXPLANATION |
|
|
|
|||||
Seein g/Hearing |
|
|
|
|
|
|
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
||||
Spea king |
|
|
|
|
|
|
|
|
|
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
|
POST URAL |
|
|
|
|
|
|
|
|
|
NORMAL |
ABNORMAL |
|
|
|
|
EXPLANATION |
|
|
|
||||||
Repe titive |
stooping |
and |
bending |
|
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
||||||
for 10ng periods |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
Rema :ining |
|
seated |
for long periods |
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
|||||||
Crou ching |
or Squatting |
|
|
|
|
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
|||||
Climt |
ling |
|
|
|
|
|
|
|
|
|
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
MENl 'AL |
|
|
|
|
|
|
|
|
|
|
NORMAL |
ABNORMAL |
|
|
|
|
EXPLANATION |
|
|
|
|||||
Unde rstanding, |
carrying |
out |
|
|
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
||||||
andr |
I~membering |
|
instructions |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
Resp cnding |
appropriately |
|
to |
|
|
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
Meet ing quality |
standards |
|
and |
|
|
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
|||||
produ 'ction |
|
norms |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Susta .ining |
adequate |
|
|
|
|
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
|||||
atten |
dance |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MAN IIPULATIVE |
|
|
|
|
|
|
NORMAL |
ABNORMAL |
|
|
|
|
EXPLANATION |
|
|
|
|||||||||
Gras~ ling, |
releasing, |
handling |
|
|
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
||||||
and |
f ingering |
|
objects |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
ENVIF ION MENTAL |
|
|
|
|
|
NORMAL |
ABNORMAL |
|
|
|
|
EXPLANATION |
|
|
|
||||||||||
Toler. °lting |
dust, |
fumes |
|
|
|
|
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
||||
extrer nes of |
temperature |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
Tolen |
lting |
exposure |
to |
|
|
|
|
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
|||
heigh |
ts or |
machinery |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
Opere lting |
a motor |
vehicle |
|
|
|
|
|
0 |
|
0 |
|
|
|
|
|
|
|
|
|
|
|
||||
- |
|
|
|
PHYSICIAN |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
EXAMINING |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
SIGNATURE |
|
|
|
|
|
|
|
|
|
|
|
(PRINT NAME) |
|
|
|
|
|
|
DATE SIGNED |
|
|
||||
X |
|
|
|
|
|
|
|
|
|
|
|
M.D. I |
|
|
|
|
|
|
|
M.D. I, |
|
|
|
||
SPECIALTY, IF ANY |
|
|
|
|
|
|
BOARD CERTIFIED |
|
|
|
|
|
BOARD ELIGIBLE |
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
DYes |
0 No |
|
|
|
|
IOFFICE |
DYes |
|
0 No |
|
|||
OFFICE ADDRESS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TELEPHONE |
NUMBER |
|
||||||||
·2·
DSS.486T (Rev. 9/91)
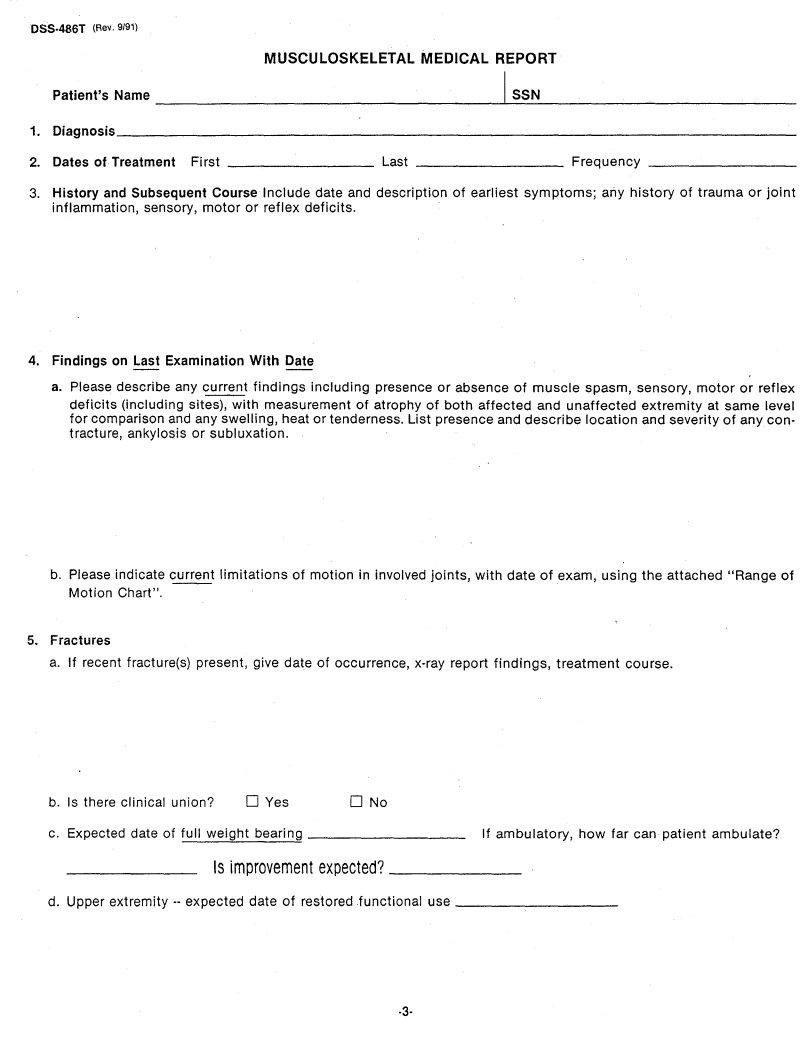
MUSCULOSKELETAL MEDICAL REPORT
|
Patient's Name |
|
I_S_S_N |
_ |
1. |
Diagnosis |
|
|
_ |
2. |
Dates of Treatment First |
Last _________ |
Frequency |
_ |
3.History and Subsequent Course Include date and description of earliest symptoms; any history of trauma or joint inflammation, sensory, motor or reflex deficits.
4.Findings on Last Examination With Date
a. Please describe any current findings including presence or absence of muscle spasm, sensory, motor or reflex
deficits (including sites), with measurement of atrophy of both affected and unaffected extremity at same level for comparison and any swelling, heat or tenderness. List presence and describe location and severity of any con- tracture, ankylosis or subluxation.
b. Please indicate current limitations of motion in involved joints, with date of exam, using the attached "Range of
Motion Chart",
5.Fractures
a. If recent fracture(s) present, give date of occurrence,
b. Is there clinical |
union? |
DYes |
o No |
|
c. Expected date of full weight |
bearing |
|
_ If ambulatory, how far can patient ambulate? |
|
|
Is improvement |
expected? |
_ |
|
d. Upper extremity |
date of restored functional use |
_ |
||
·3-
DSS~486T (Rev. 9/91) .
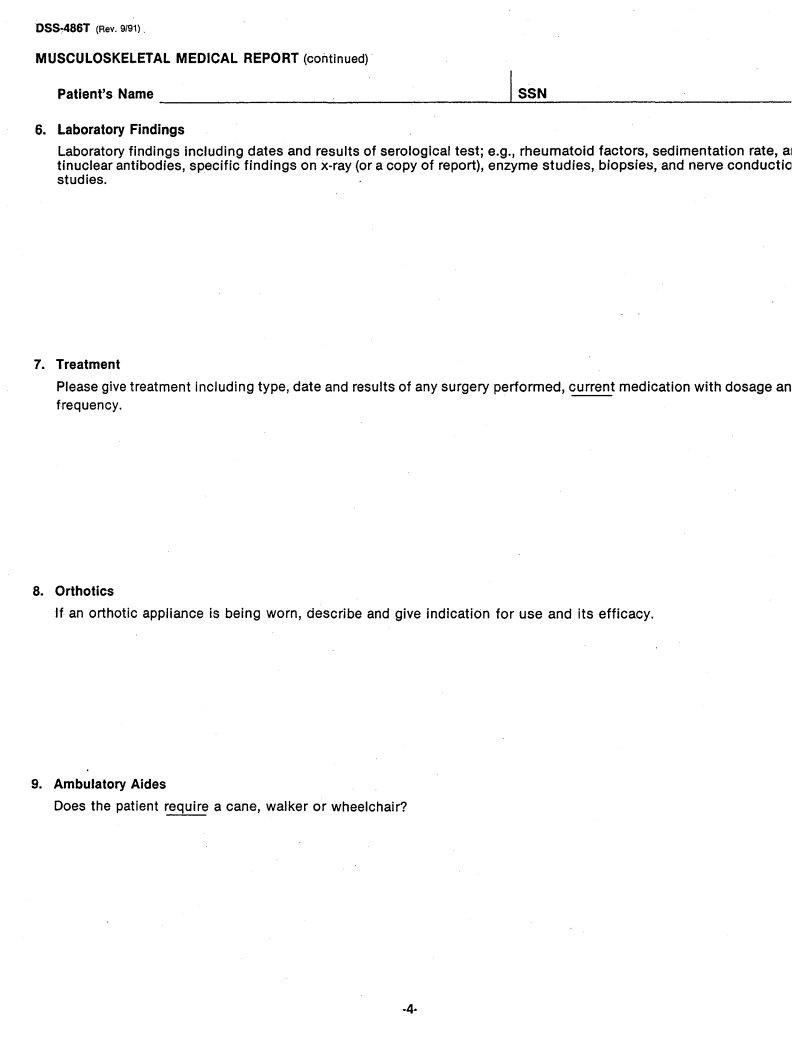
MUSCULOSKELETAL MEDICAL REPORT (continued)
Patient's Name |
1 |
SSN |
|
6.Laboratory Findings
Laboratory findings including dates and results of serological test; e.g., rheumatoid factors, sedimentation rate, al tinuclear antibodies, specific findings on
7.Treatment
Please give treatment including type, date and results of any surgery performed, current medication with dosage an frequency.
8.Orthotics
If an orthotic appliance is being worn, describe and give indication for use and its efficacy.
9.Ambulatory Aides
Does the patient require a cane, walker or wheelchair?
DSS.4Cl6T (Rev. 9/91)
|
MUSCULOSKELETAL MEDICAL REPORT |
|
Spinal Disorders |
Patient's Name |
I SSN |
1.Diagnosis
2. Dalles of Treatment |
First |
Last |
Frequency |
_ |
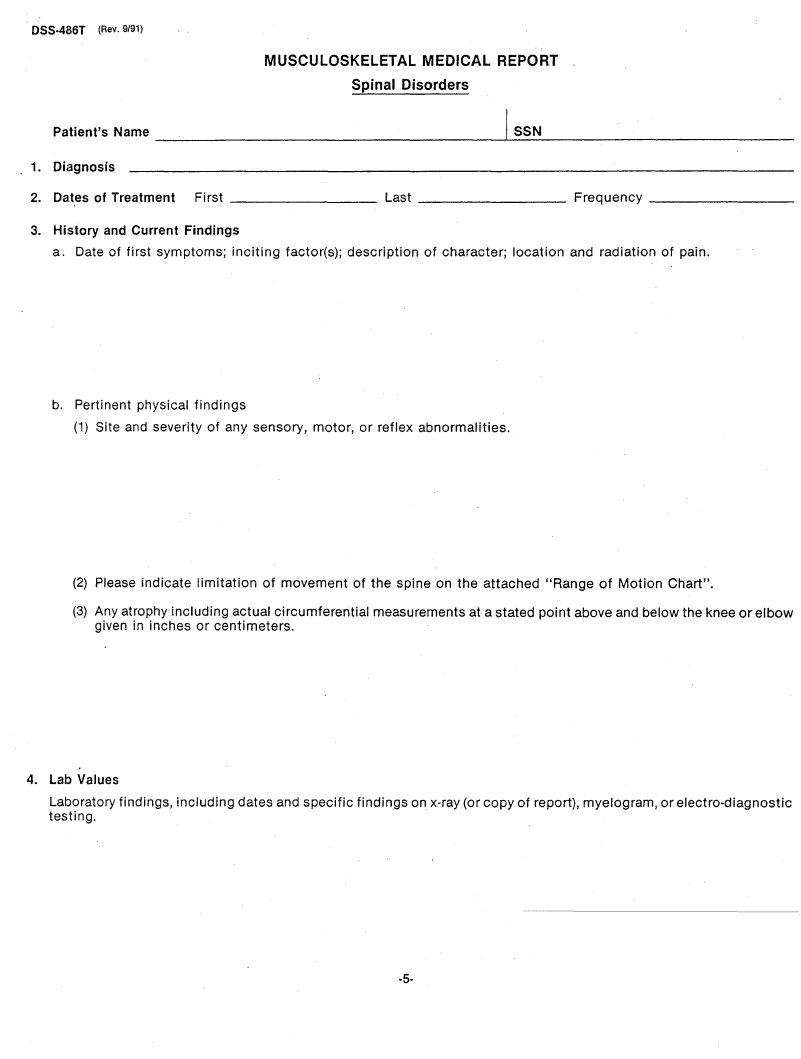
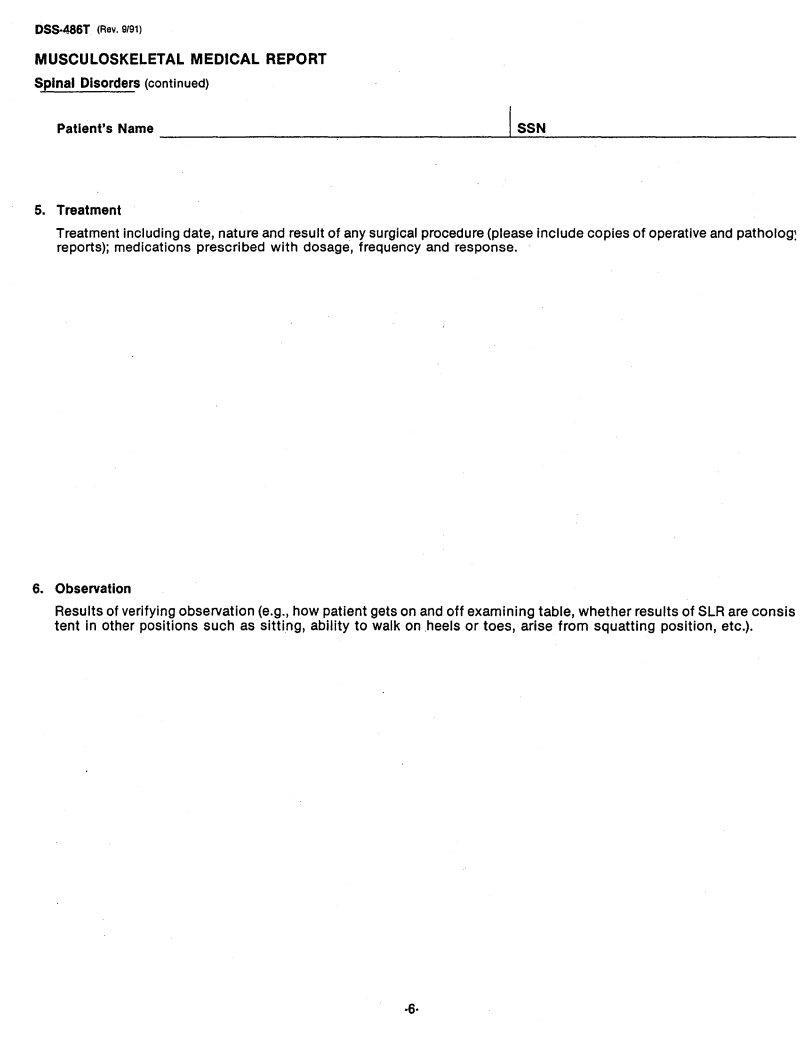
3.History and Current Findings
a. Date of first symptoms; inciting factor(s); description of character; location and radiation of pain.
b. Pertinent physical findings
(1) Site and severity of any sensory, motor, or reflex abnormalities.
(2)Please indicate limitation of movement of the spine on the attached "Range of Motion Chart".
(3)Any atrophy including actual circumferential measurements at a stated point above and below the knee or elbow given in inches or centimeters.
4.Lab Values
Laboratory findings, including dates and specific findings on
·5·
DSS·486T (Rev. 9191)
MUSCULOSKELETAL MEDICAL REPORT
Spinal Disorders (continued)
Patient's Name |
1 SSN |
5.Treatment
Treatment including date, nature and result of any surgical procedure (please include copies of operative and patholog~ reports); medications prescribed with dosage, frequency and response.
6.Observation
Results of verifying observation (e.g., how patient gets on and off examining table, whether results of SLR are consis tent in other positions such as sitting, ability to walk on .heels or toes, arise from squatting position, etc.).
·6·
055·486T (Rev. 9/91)
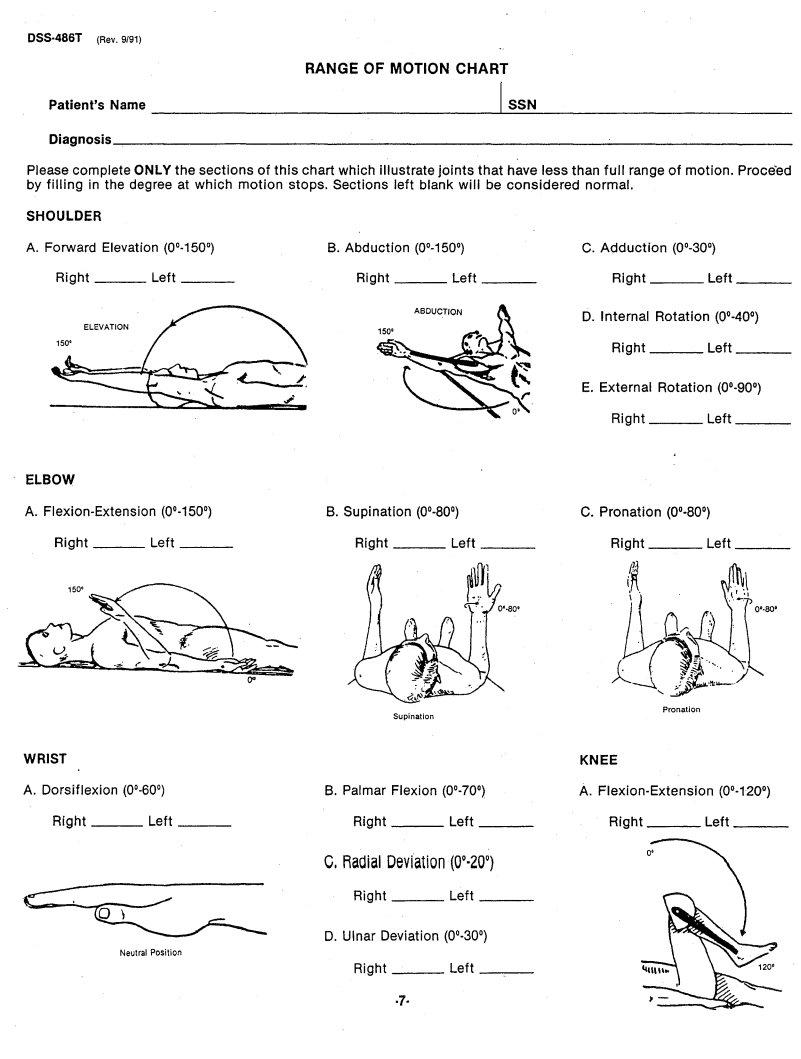
RANGE OF MOTION CHART
Patient's Name |
I_S_S_N |
_ |
|
Diagnosis |
|
|
_ |
Please complete ONLY the sections of this chart which illustrate joints that have less than full range of motion. Proce'ed by filling in the degree at which motion stops. Sections left blank will be considered normal.
SHOULDER |
|
|
|
|
|
|
|
|
A. Forward Elevation |
B. Abduction |
|
|
|
|
|||
Right |
Left |
_ |
Right |
Left |
_ |
Right |
Left |
_ |
ABDUCTION
D. Internal Rotation
Right Left _
E. External Rotation
Right Left _
ELBOW |
|
|
|
|
|
|
|
|
A. |
|
B. Supination |
|
C. Pronation |
|
|||
Right |
Left |
_ |
Right |
Left |
_ |
Right |
Left |
_ |
Pronation
Supination
WRIST |
|
|
|
|
|
KNEE |
|
|
A. Dorsiflexion |
|
B. Palmar Flexion |
|
A. |
||||
Right |
Left |
_ |
Right |
Left |
_ |
Right |
Left |
_ |
C. Radial Deviation |
(00'200) |
|
Right |
Left |
_ |
D. Ulnar Deviation |
|
|
Neutral Position |
|
|
Right |
Left |
_ |
·7·
DSS·486T (Rev. 9191)
RANGE OF MOTION CHART (Continued)
Patient's |
Name |
|
|
|
ISSN |
|
|
|
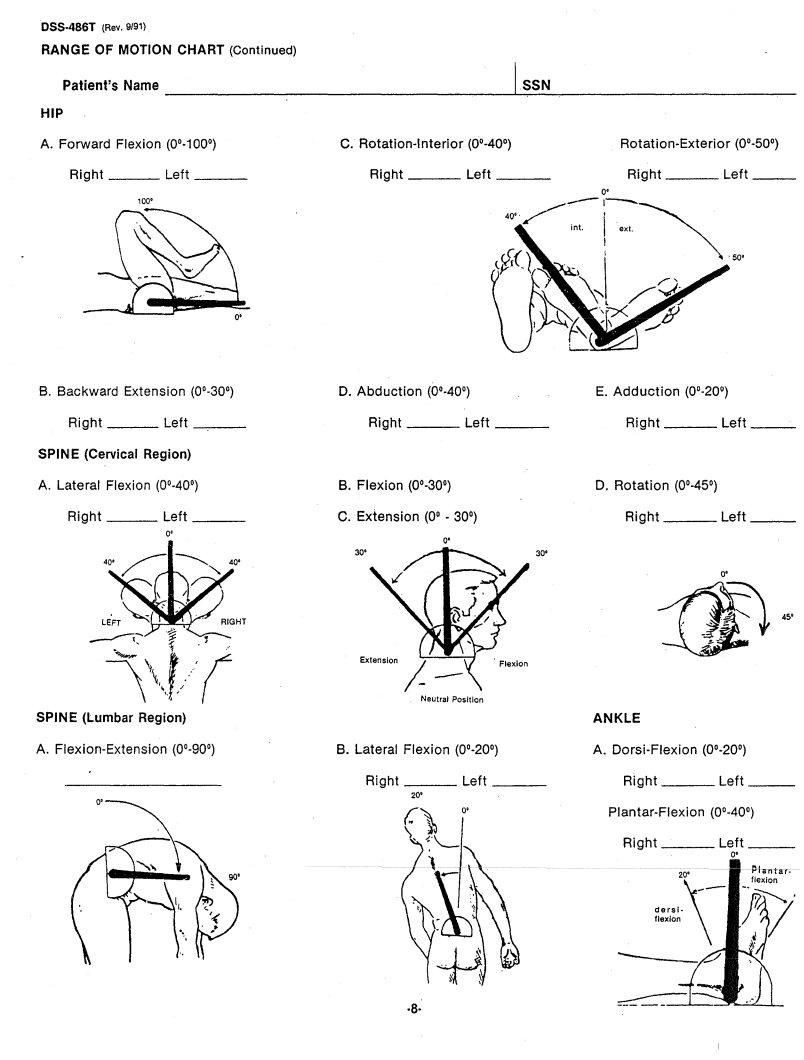
HIP |
|
|
|
|
|
|
|
|
A. Forward |
Flexion (0°·100°) |
|
C. |
|
|
|||
Right |
Left |
_ |
Right |
Left |
_ |
Right |
Left |
_ |
|
100' |
|
|
|
|
|
|
|
B. Backward Extension |
|
|
|
|
|
|
|
Right |
Left |
_ |
Right |
Left |
_ |
Right |
Left __ |
SPINE (Cervical |
Region) |
|
|
|
|
|
|
A. Lateral Flexion |
|
B. Flexion |
|
|
|
||
Right |
Left |
_ |
C. Extension |
(0° - 30°) |
|
Right |
Left~_ |
|
O' |
|
|
0' |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
30' |
|
|
|
|
|
|
|
|
|
0' |
45'
SPINE (Lumbar Region) |
|
|
|
ANKLE |
|
|
|
|
|||
A. |
B. Lateral Flexion |
|
A. |
|
|
||||||
|
|
Right |
Left |
_ |
|
Right |
|
|
Left |
_ |
|
|
|
20' |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
Right |
|
|
Left |
_ |
|
|
|
|
|
|
|
|
|
|
|
a' |
|
|
|
|
|
|
|
|
|
|
|
|
"'.1 ... |
|
|
|
|
|
20' |
|
• flexionf'"T |
||||
|
|
|
|
|
|
|
dersl· |
\ |
- |
|
|
|
|
|
|
|
|
- |
flexion |
|
|
||
·8·---
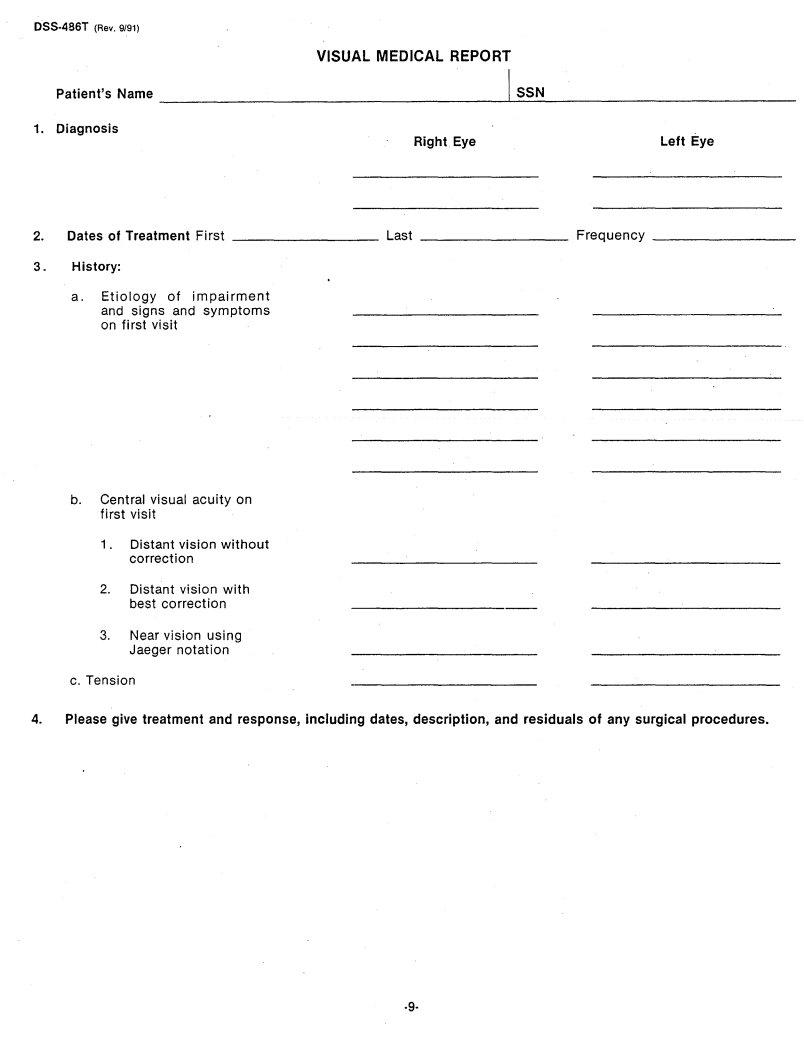
DSS·486T (Rev. 9/91) |
|
|
|
VISUAL MEDICAL REPORT |
|
|
|
Patient's Name |
I |
SSN |
|
1. Diagnosis |
|
|
|
Right Eye |
|
|
Left Eye |
2. |
Dates of Treatment First |
Last |
_ Frequency |
_ |
3.History:
a.Etiology of impairment and signs and symptoms on first visit
b.Central visual acuity on first visit
1.Distant vision without correction
2.Distant vision with best correction
3.Near vision using Jaeger notation
c.Tension
4.Please give treatment and response, including dates, description, and residuals of any surgical procedures .
.g.
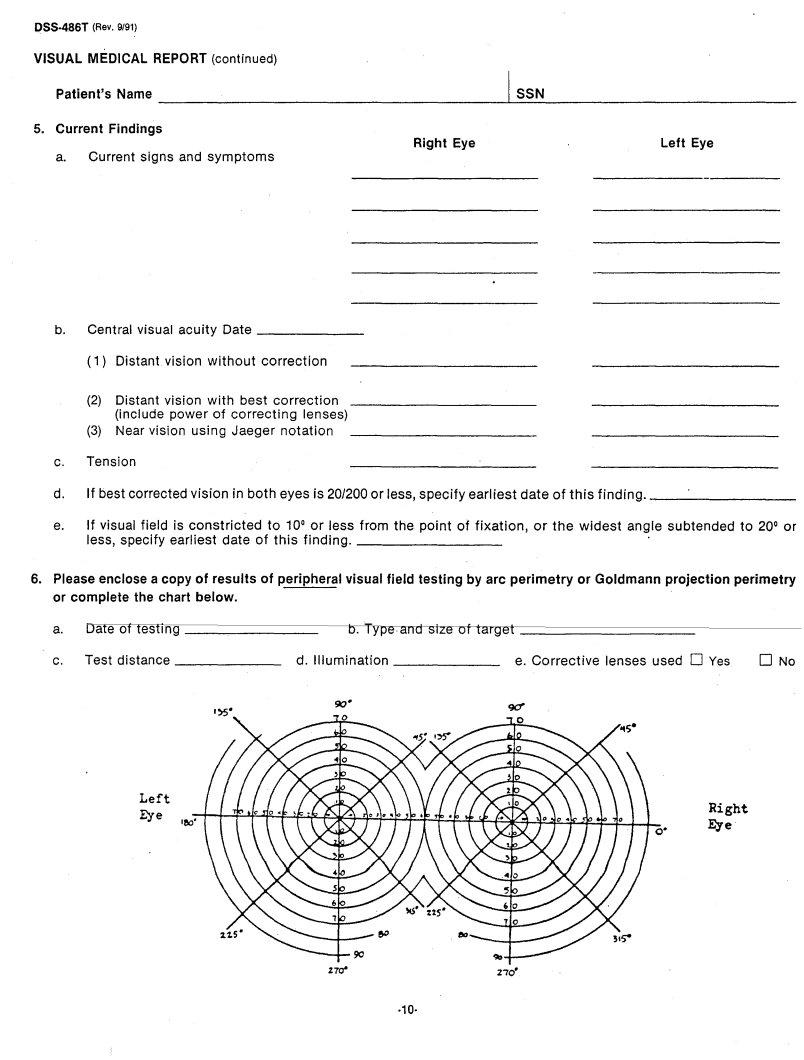
DSS·4.86T |
(Rev. 9/91) |
|
|
VISUAL |
MEDICAL REPORT (continued) |
|
|
Patient's |
Name |
1 SSN |
|
5. Current |
Findings |
|
|
|
|
Right Eye |
Left Eye |
a.Current signs and symptoms
b. |
Central visual acuity Date |
_ |
(1)Distant vision without correction
(2)Distant vision with best correction (include power of correcting lenses)
(3)Near vision using Jaeger notation
c. Tension
d. |
If best corrected vision in both eyes is 20/200 or less, specify earliest date of this finding. |
_ |
e.If visual field is constricted to 10° or less from the point of fixation, or the widest angle subtended to 20° or
less, specify earliest date of this finding. |
_ |
6.Please enclose a copy of results of peripheral visual field testing by arc perimetry or Goldmann projection perimetry or complete the chart below.
a. |
LJate of testing |
|
_ |
b. Type |
and size of target |
_ |
|
c. |
Test distance |
_ |
d. |
Illumination |
_ e. Corrective |
lenses used 0 Yes |
o No |
Left
Eye |
|
|
Right |
180· |
|
Eye |
|
|
|
||
|
|
O· |
|
|
|
|
·10·
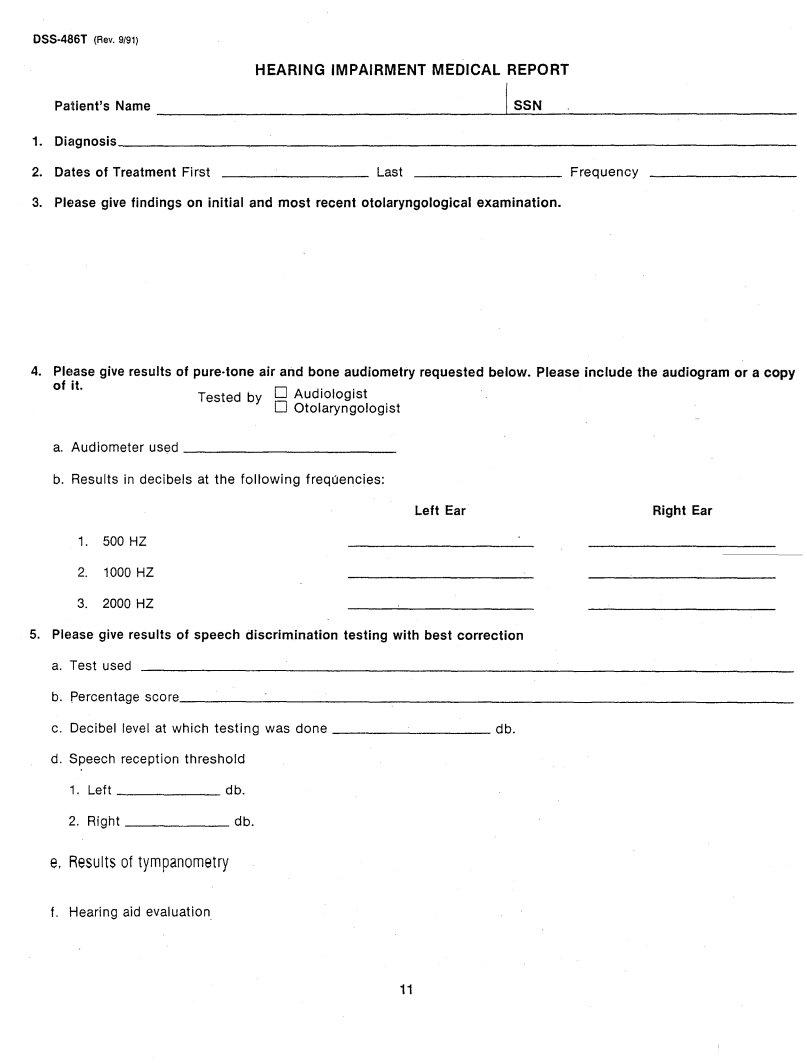
|
HEARING |
IMPAIRMENT MEDICAL |
REPORT |
|
Patient's Name |
|
I SSN |
1. |
Diagnosis |
|
_ |
2. |
Dates of Treatment First |
Last _________ |
Frequency |
3.Please give findings on initial and most recent otolaryngological examination.
4.PIElase give results of pure·tone air and bone audiometry requested below. Please include the audiogram or a copy
of |
it. |
|
|
0 A |
d' I . t |
|
|
Tested |
by |
u |
loogls |
|
|
|
|
o Otolaryngologist |
|
a. Audiometer |
used |
|
|
_ |
|
b. |
Results in |
decibels at the |
following frequencies: |
||
Left Ear |
Right Ear |
1.500 HZ
2.1000 HZ
3.2000 HZ
5.PIElase give results of speech discrimination testing with best correction
a. Test used
b. |
percentage score |
|
_ |
||
c. |
Decibel |
level at which testing was done |
db. |
||
d. Speech |
reception |
threshold |
|
||
|
1. |
Left |
|
db. |
|
|
2. |
Right |
|
db. |
|
e.Results of tympanometry
f.Hearing aid evaluation
11
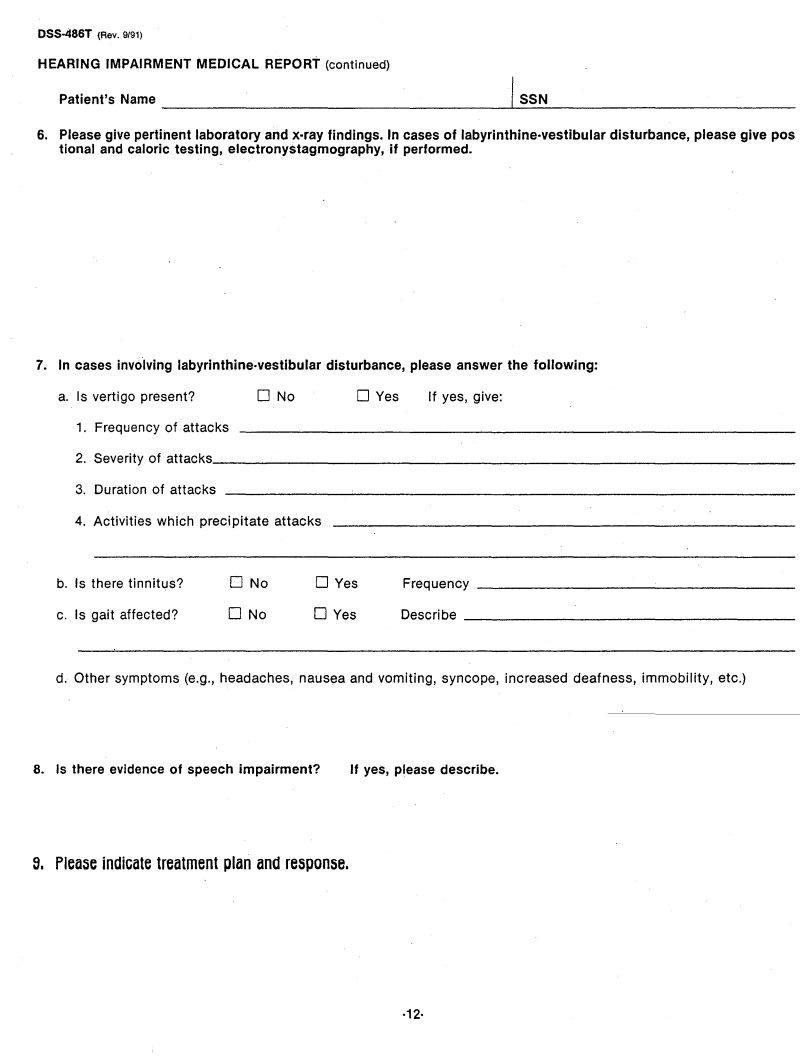
|
|
HEARING IMPAIRMENT MEDICAL REPORT (continued) |
|
Patient's Name |
~ISSN |
6.Please give pertinent laboratory and
7. In cases involving labyrinthine·vestibular disturbance, please answer the following:
a. Is vertigo present? |
o No |
DYes |
If yes, give: |
|
1. |
Frequency of attacks |
|
|
|
2. |
Severity of attacks |
|
|
_ |
3.Duration of attacks
4.Activities which precipitate attacks
b. Is there tinnitus? |
o No |
DYes |
Frequency |
_ |
|
|
|||
c. Is gait affected? |
o No |
DYes |
Describe |
_ |
|
|
d. Other symptoms (e.g., headaches, nausea and vomiting, syncope, increased deafness, immobility, etc.)
8. Is there evidence of speech impairment? |
If yes, please describe. |
9. Please indicate treatment plan and response.
·12·
|
|
|
|
|
||
|
|
RESPIRATORY MEDICAL REPORT |
|
|||
|
Patient's Name |
|
|
I_S_S_N |
_ |
|
1. |
Diagnosis |
|
|
|
|
_ |
2. |
Dates of Treatment First |
_________ |
Last _________ |
Frequency |
||
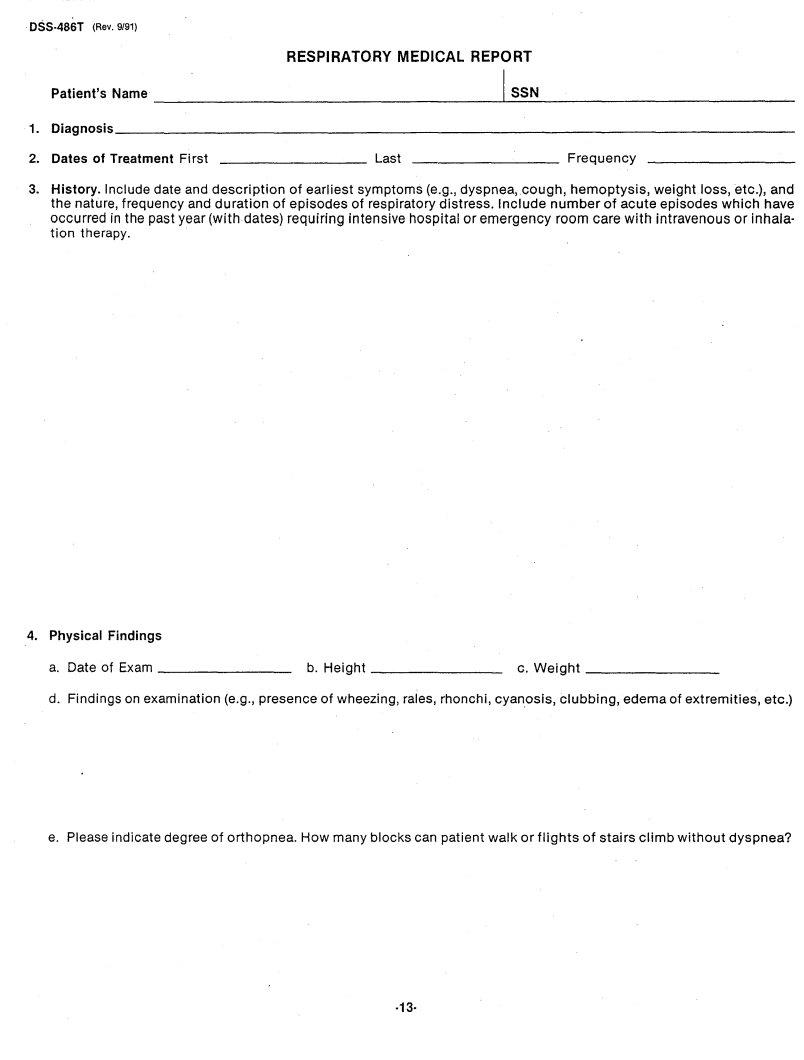
3.History. Include date and description of earliest symptoms (e.g., dyspnea, cough, hemoptysis, weight loss, etc.), and the nature, frequency and duration of episodes of respiratory distress. Include number of acute episodes which have occurred in the past year (with dates) requiring intensive hospital or emergency room care with intravenous or inhala- tion therapy.
4. Physical Findings
a. Date of Exam |
_ b. Height |
_ c. Weight |
_ |
d. Findings on examination (e.g., presence of wheezing, rales, rhonchi, cyanosis, clubbing, edema of extremities, etc.)
e. Pleaseindicate degree of orthopnea. How many blocks can patient walk or flights of stairs climb without dyspnea?
·13·
DSS.486T (Rev. 9/91)
RESPIRATORY MEDICAL REPORT (continued)
Patient's Name |
, |
SSN |
|
|
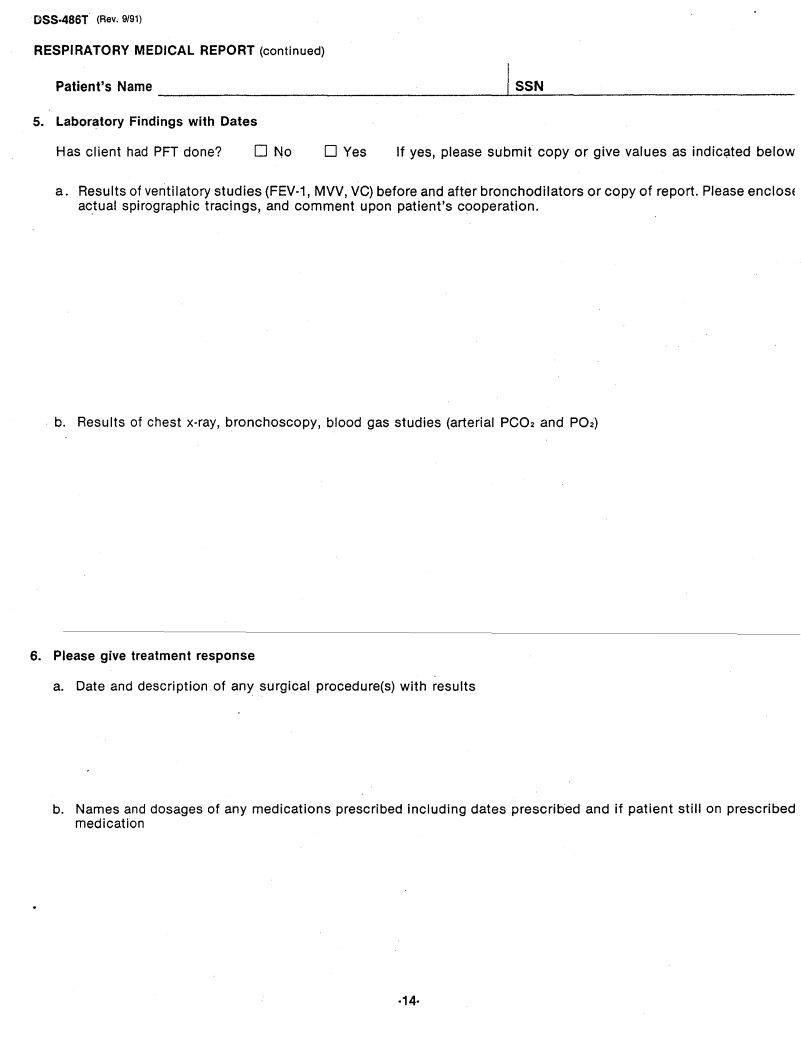
5.Laboratory Findings with Dates
Has client had PFT done? |
o No |
DYes |
If yes, please submit copy or give values as indic~ted below |
a.Results of ventilatory studies
b.Results of chest
6.Please give treatment response
a. Date and description of any surgical procedure(s) with results
b.Names and dosages of any medications prescribed including dates prescribed and if patient still on prescribed medication
·14·
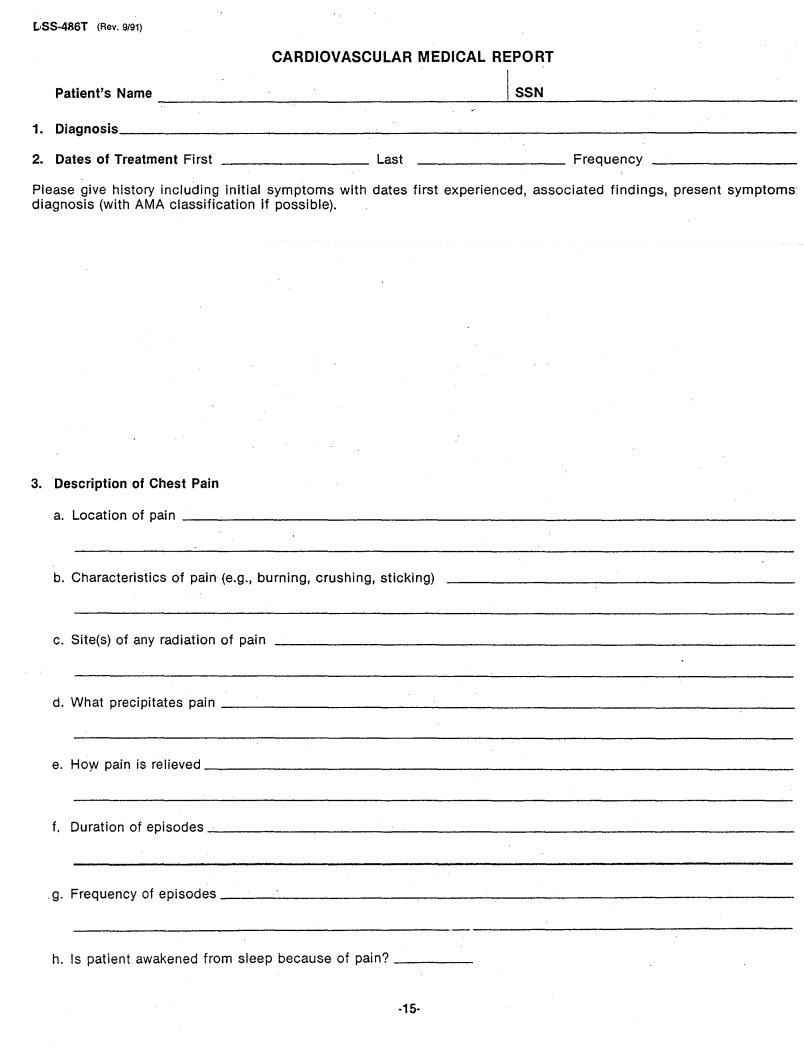
CARDIOVASCULAR MEDICAL REPORT
|
Patient's Name |
|
|
I_S_S_N |
_ |
1. |
Diagnosis |
|
|
|
_ |
2. |
Dates of Treatment First |
_________ |
Last _________ |
Frequency |
|
|
|
|
|
||
Please give history including initial symptoms with dates first experienced, associated findings, present symptoms diagnosis (with AMA classification if possible).
3. Description of Chest Pain |
|
a. Location of pain |
_ |
b. Characteristics of pain (e.g., burning, crushing, sticking) |
|
c. Site(s) of any radiation of pain |
|
d. What precipitates pain |
_ |
e. HoY' pain is relieved |
_ |
f. Duration of episodes |
_ |
.g. Frequency of episodes |
_ |
h. Is patient awakened from sleep because of pain? |
_ |
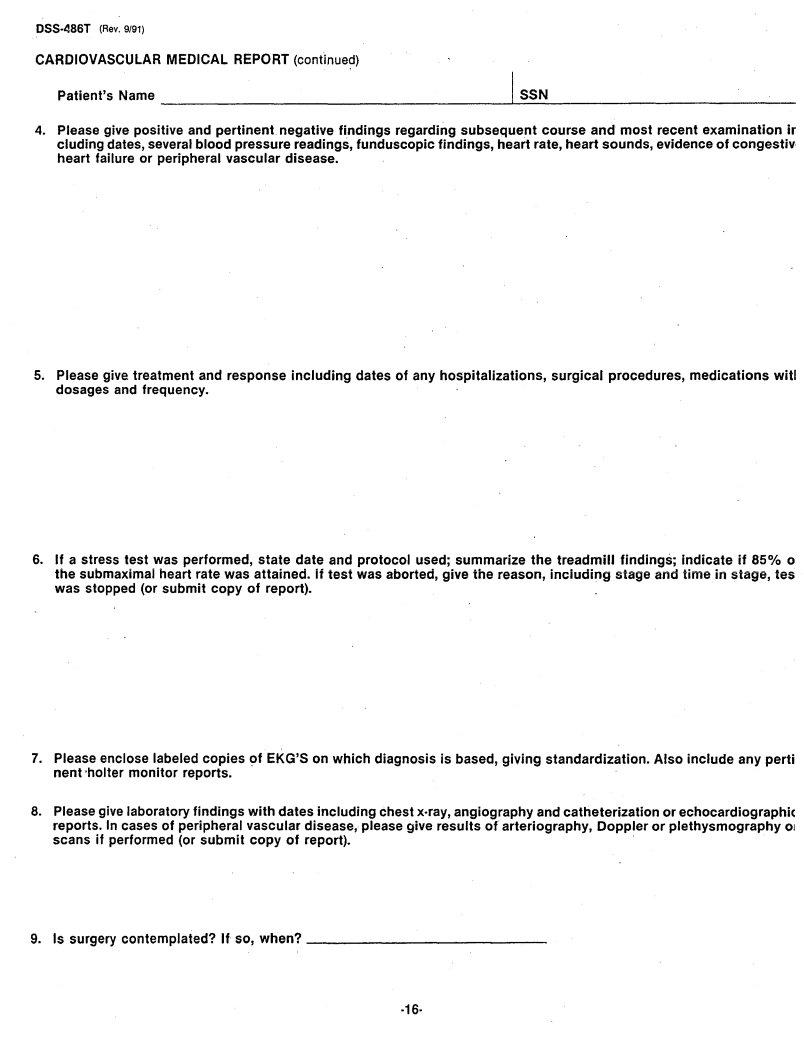
CARDIOVASCULAR MEDICAL REPORT (continued)
Patient's Name |
1 |
SSN |
|
4.Please give positive and pertinent negative findings regarding subsequent course and most recent examination ir eluding dates, several blood pressure readings, funduscopic findings, heart rate, heart sounds, evidence of congestiv heart failure or peripheral vascular disease.
5.Please give.treatment and response including dates of any hospitalizations, surgical procedures, medications wit! dosages and frequency.
6.If a stress test was performed, state date and protocol used; summarize the treadmill findings; indicate if 85% 0 the submaximal heart rate was attained. if test was aborted, give the reason, inciuding stage and time in stage, tes was stopped (or submit copy of report).
7.Please enclose labeled copies of EKG'S on which diagnosis is based, giving standardization. Also include any perti nent 'holter monitor reports.
8.Pleasegive laboratory findings with dates including chest
9. Is surgery contemplated? If so, when? |
_ |
DSS·486T (Rev. 9/91) |
|
|
|
|
|
||
|
|
|
DIGESTIVE |
'MEDICAL |
REPORT |
|
|
|
Patient's |
Na~e ~~~~~~~~~~~~~~~~~~~~I~S~S~N~~~~~~~~~~~~~~~ |
|
|
|||
1. |
Diagnosis~~~~~_~_~~~_~ |
__ |
~_~~ |
__ |
~~~~~_~~~_~~_~~~~~ |
|
|
2. |
Dates of |
Treat~ent First |
|
Last |
|
Frequency _~_~~~ |
__ |
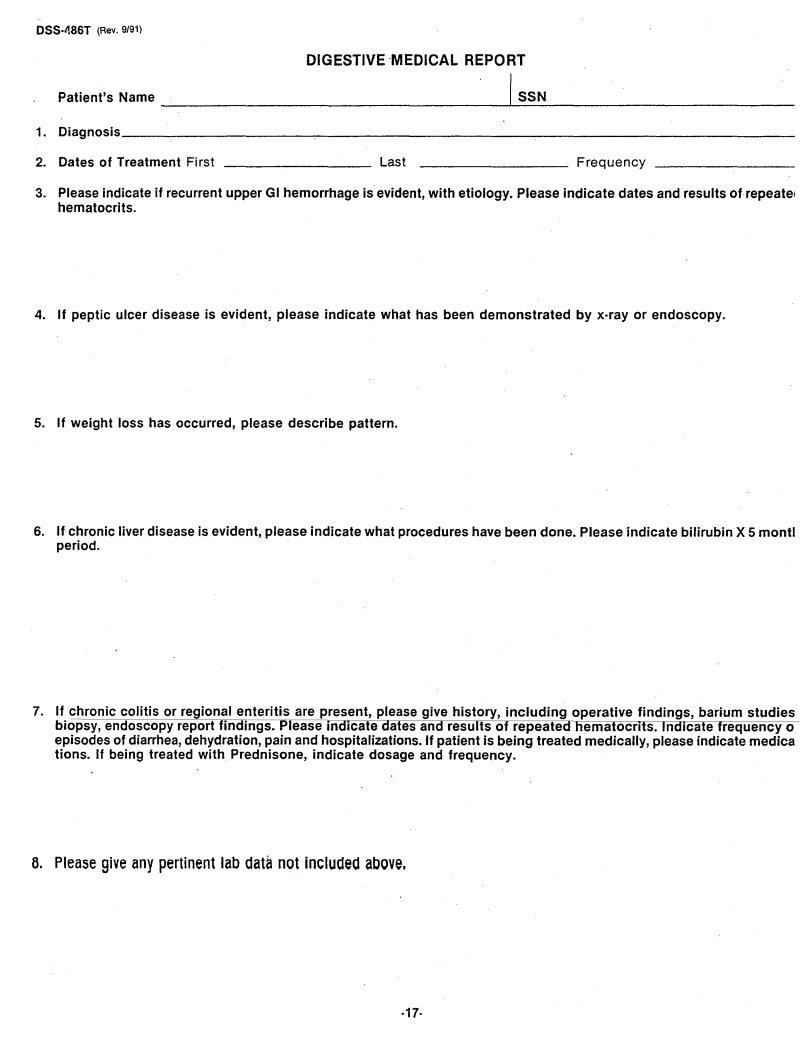
3.Please indicate if recurrent upper GI hemorrhage is evident, with etiology. Please indicate dates and results ofrepeate' he~atocrits.
4.If peptic ulcer disease is evident, please indicate what has been demonstrated by x·ray or endoscopy.
5.If weight loss has occurred, please describe pattern.
6.If chronic liver disease is evident, please indicate what procedures have been done. Please indicate bilirubin X 5 montl period.
7.If chronic colitis or regional enteritis are present, please give history, including operative findings, bariu~ studies biopsy, endoscopy report findings. Please indicate dates and results of repeated hematocrits. Indicate frequency 0 episodes of diarrhea, dehydration, pain and hospitalizations. If patient is being treated medically, please indicate ~edica tions. If being treated with Prednisone, indicate dosage and frequency.
6.Please give any pertinent lab data not included above.
·17·
OSS.4B6T (Rev. 9/91)
GENITO·URINARY MEDICAL REPORT
|
Patient's Name |
|
I_S_S_N |
_ |
1. |
Diagnosis |
|
|
_ |
2. |
Dates of Treatment First |
_ Last |
Frequency |
_ |
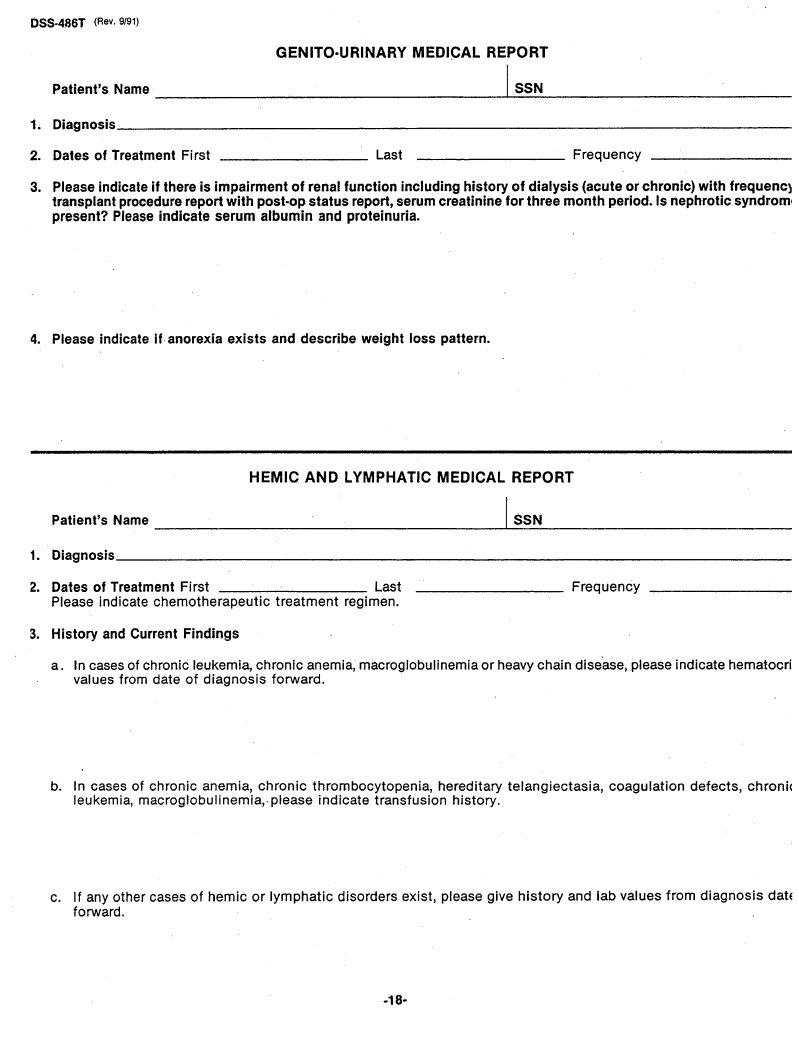
3.Please indicate if there is impairment of renal function including history of dialysis (acute or chronic) with frequencl transplant procedure report with post·op status report, serum creatinine for three month period. Is nephrotic syndroml present? Please indicate serum albumin and proteinuria.
4. Please indicate if· anorexia exists and describe weight loss pattern.
HEMIC AND LYMPHATIC MEDICAL REPORT
|
Patient's Name |
|
I SSN |
1. |
Diagnosis |
|
_ |
2. |
Dates of Treatment First |
Last _________ |
Frequency |
Please indicate chemotherapeutic treatment regimen.
3.History and Current Findings
a.In cases of chronic leukemia, chronic anemia, macroglobulinemia or heavy chain dise'ase, please indicate hematocri values from date of diagnosis forward.
b. In cases of chronic anemia, chronic thrombocytopenia, hereditary telangiectasia, coagulation defects, chronic leukemia, macroglobulinemia,- please indicate transfusion history.
c.If any other cases of hemic or lymphatic disorders exist, please give history and lab values from diagnosis datE forward.
9/91) |
|
|
|
|
|
||
|
|
SKIN |
DISORDERS |
MEDICAL REPORT |
|
||
|
Patient's |
Name |
|
|
I_S_s_N |
_ |
|
1. |
Diagnosis |
|
|
|
|
|
_ |
2. |
Dates of Treatment First |
Last |
_________ |
|
|
Frequency |
|
3. |
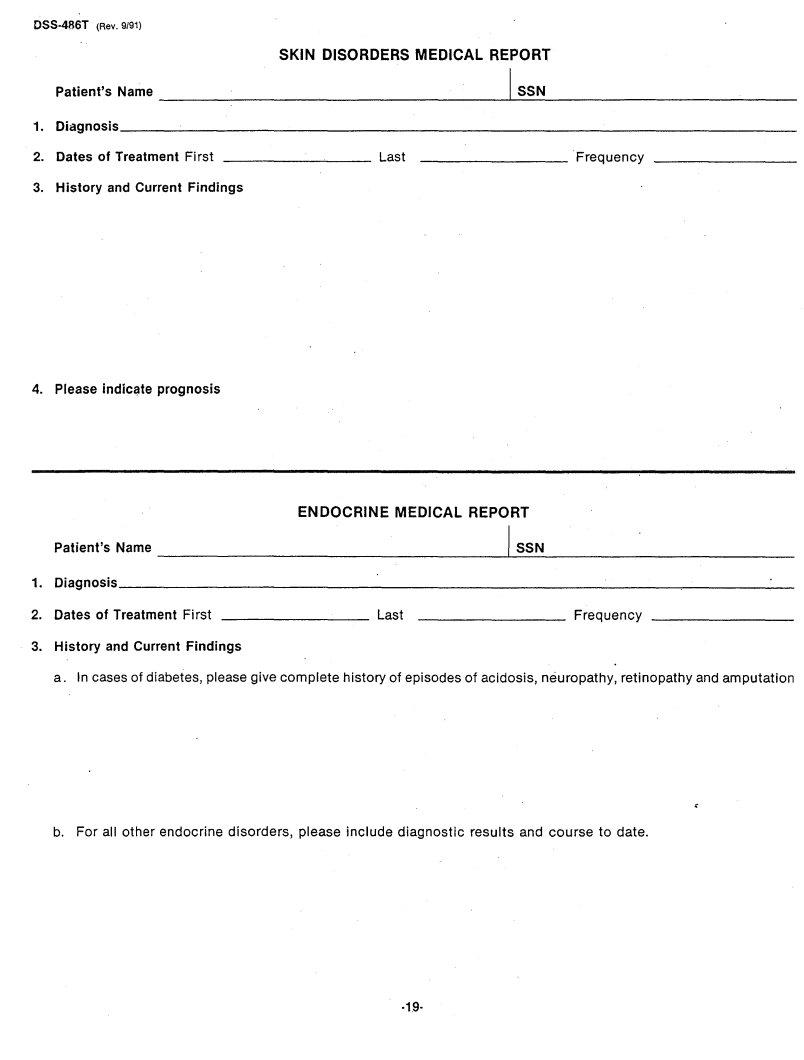
History and Current Findings |
|
|
|
|
|
|
4. Please indicc;lteprognosis
|
|
ENDOCRINE MEDICAL |
REPORT |
|
||
|
Patient's Name |
|
|
I~S_S_ |
N |
_ |
1. |
Diagnosis |
|
|
|
|
|
2. |
Dates of Treatment First ________ |
Last |
|
|
|
Frequency |
3.History and Current Findings
a. In cases of diabetes, please give complete history of episodes of acidosis, neuropathy, retinopathy and amputation
b. For all other endocrine disorders, please include diagnostic results and course to date.
·19·
MULTIPLE BODY SYSTEMS MEDICAL REPORT
|
Patient's Name |
|
ISSN |
1. |
Diagnosis |
|
_ |
2. |
Dates of Treatment First· |
Last ________ |
Frequency |
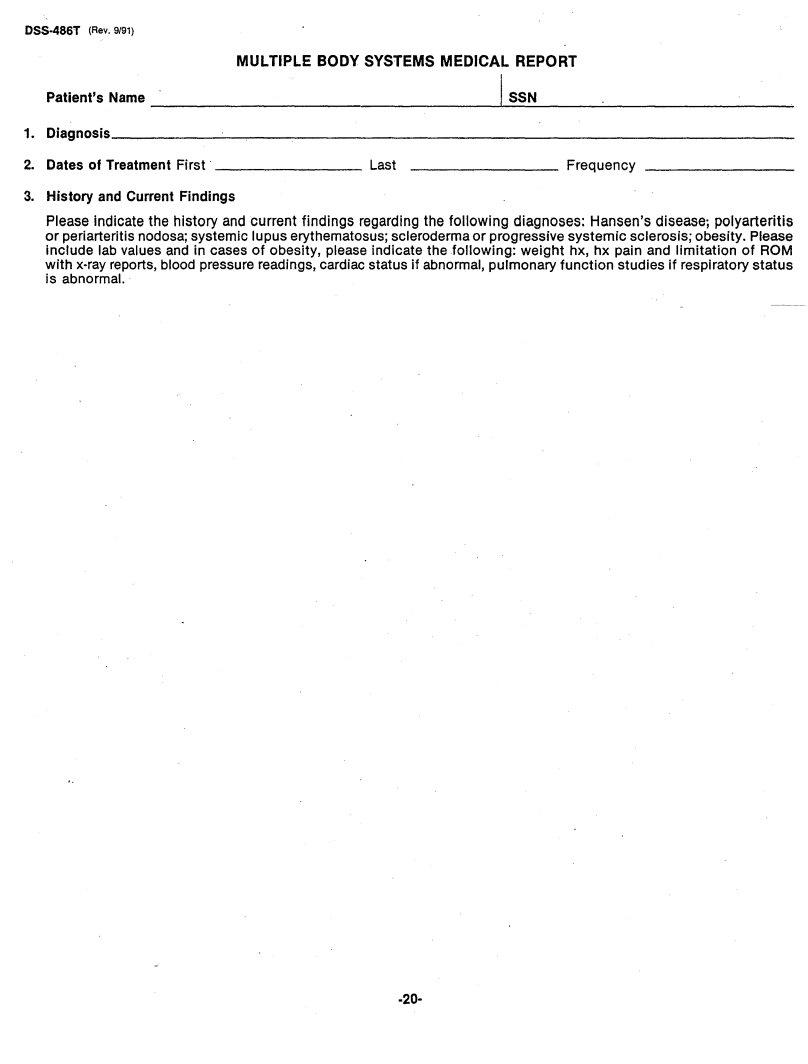
3.History and Current Findings
Please indicate the history and current findings regarding the following diagnoses: Hansen's disease; polyarteritis or periarteritis nodosa; systemic lupus erythematosus; scleroderma or progressive systemic sclerosis; obesity. Please include lab values and in cases of obesity, please indicate the following: weight hx, hx pain and limitation of ROM with
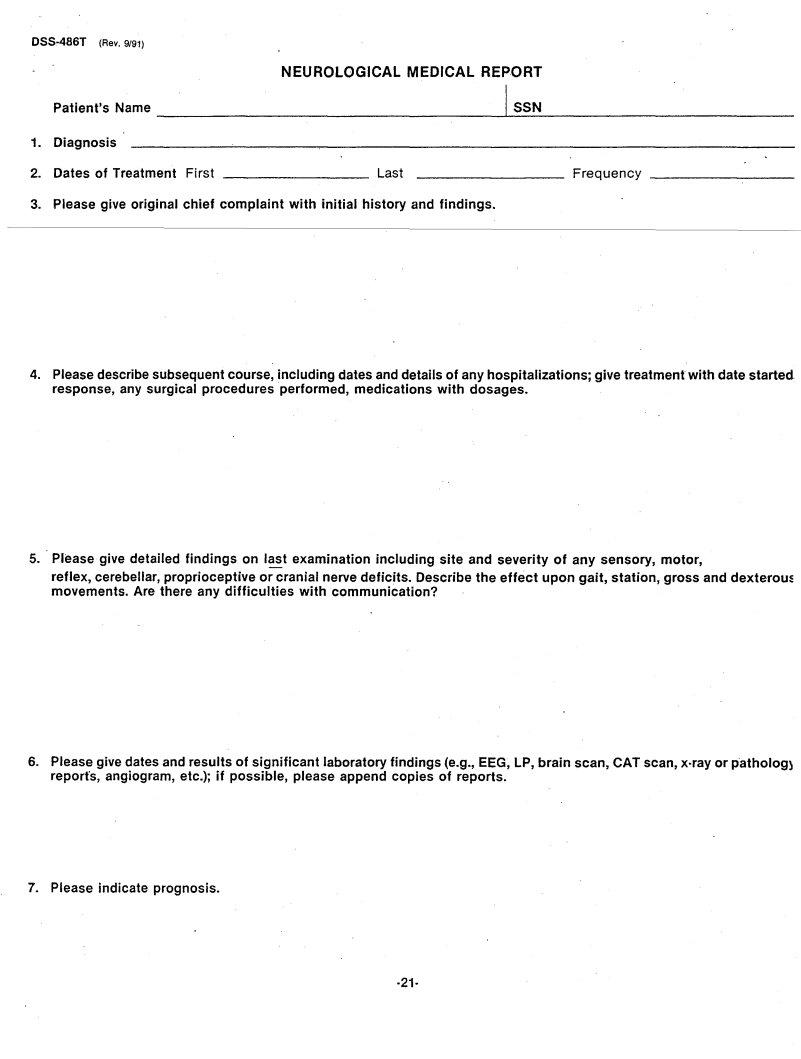
NEUROLOGICAL MEDICAL REPORT
Patient's Name |
I_S_S_N |
_ |
1.Diagnosis
2. Dates of Treatment First _________ |
Last _________ |
Frequency |
_ |
3.Please give original chief complaint with initial history and findings.
4.Please describe subsequent course, including dates and details of any hospitalizations; give treatment with date started. response, any surgical procedures performed, medications with dosages.
5.Please give detailed findings on last examination including site and severity of any sensory, motor,
reflex, cerebellar, proprioceptive or cranial nerve deficits. Describe the effect upon gait, station, gross and dexteroul: movements. Are there any difficulties with communication?
6.Please give dates and results of significant laboratory findings (e.g., EEG, LP, brain scan, CAT scan, x·ray or patholog) report's, angiogram, etc.); if possible, please append copies of reports.
7.Please indicate prognosis.
·21-

055·486T (Rev. 9/91)
PSYCHIATRIC MEDICAL REPORT
Patienfs Na~e ~~~~~~~~~~~~~~~~~~~~I~S~S~N~~~~~~~~~~~~~~
1.Dibgnosis (including history, withdate(s) of hospitalization(s), findings on initial comprehensive mental status ex am, diagnosis according to APA terminology per DSM III. If dx of MR is given, please indicate 1.0. test results anc name of test administered.)
2. Dates of Treatment First _________ |
Last _~~~~~~ |
__ Frequency |
3. Clinical Course (including type of treat.ment, names and dosages of any drugs prescribed, response to treatment]
4. Date ( |
) and description of ~ost recent mental status exam to include a full description of th! |
following, together with examples: |
|
a. Attitude, |
appearance, behavior |
b. Speech, thought organization, thought content
c. Mood and affect
·22·
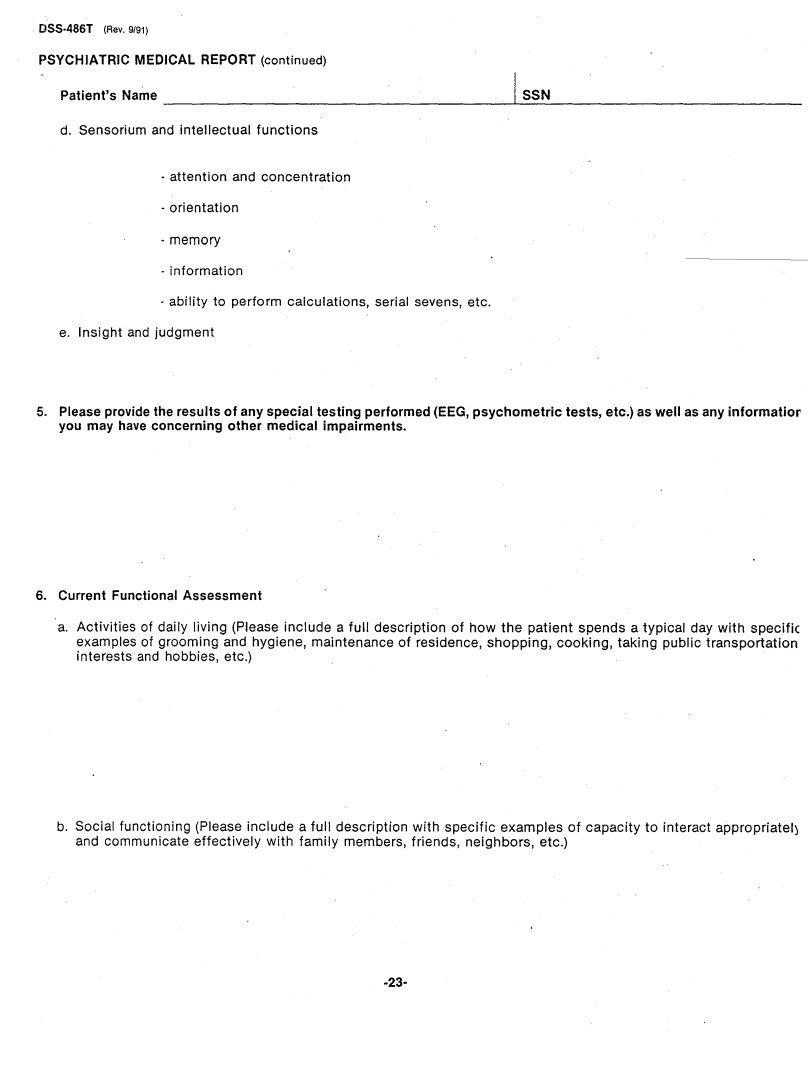
OSS·486T (Rev. 9/91) |
|
PSYCHIATRIC MEDICAL |
REPORT (continued) |
Patient's Name |
I SSN |
d. Sensorium and intellectual functions
·attention and concentration
·orientation
·memory
-information
"ability to perform calculations, serial sevens, etc. e. Insight and judgment
5.Please provide the results of any special testing performed (EEG,psychometric tests, etc.) as well as any informatior you may have concerning other medical impairments.
6.Current Functional Assessment
a.Activities of daily living (Please include a full description of how the patient spends a typical day with specifiC examples of grooming and hygiene, maintenance of residence, shopping, cooking, taking public transportation interests and hobbies, etc.)
b. Social functioning (Please include a full description with specific examples of capacity to interact appropriatel) and communicate effectively with family members, friends, neighbors, etc.)
rSYCHIATRIC MEDICAL REPORT (continued)
Patient's Name |
, SSN |
7.Ability to Function in a Work Setting. Please describe in detail any difficulties in work or
8. If suicidal features are present, describe in detail, and include whatever management steps have been taken.
9. Other Comments
·24·
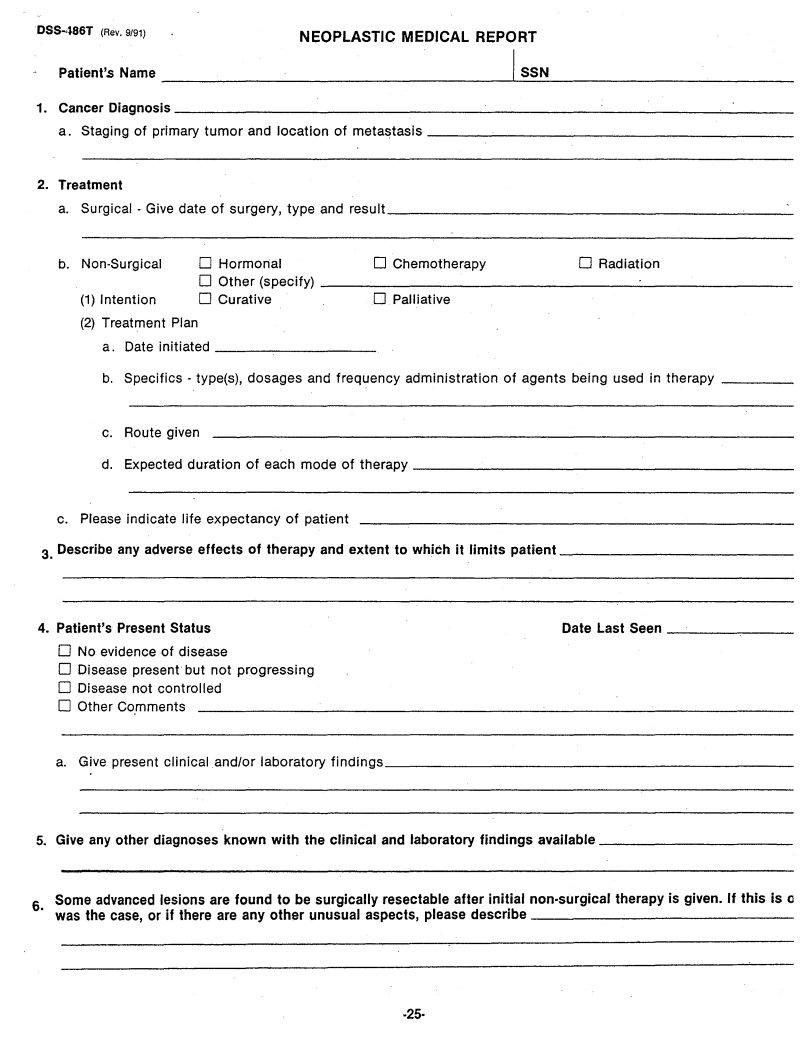
NEOPLASTIC MEDICAL REPORT
|
Patient's |
Name |
|
|
|
|
|
|
|
I |
SSN |
|
||
1. |
Cancer Diagnosis |
|
|
|
|
|
|
|
|
|
_ |
|||
|
a. |
Staging |
of primary tumor |
and location |
of |
metastasis |
|
|
|
_ |
||||
2. |
Treatment |
|
|
|
|
|
|
|
|
|
|
|
||
|
a. |
Surgical |
- Give date of surgery, type and |
result |
|
|
|
_ |
||||||
|
b. |
o Hormonal |
|
|
0 Chemotherapy |
|
o Radiation |
|
||||||
|
|
|
|
|
o Other |
(specify) |
|
|
|
|
~ |
_ |
||
|
|
(1) Intention |
o Curative |
|
|
0 Palliative |
|
|
|
|
||||
|
|
(2) Treatment Plan |
|
|
|
|
|
|
|
|
|
|||
|
|
a. |
Date initiated |
|
|
|
|
_ |
|
|
|
|
||
|
|
b. |
Specifics |
- type(s), |
dosages |
and frequency administration |
of |
agents being used in therapy |
_ |
|||||
|
|
c. |
Route given |
|
|
|
|
|
|
|
|
|
||
|
|
d. |
Expected |
duration |
of |
each |
mode of therapy |
|
_ |
|||||
|
c. Please indicate life expectancy of patient |
|
|
|
|
|
||||||||
3. Describe |
any adverse effects |
of therapy and extent to which it |
limits |
patient |
_ |
|||||||||
4. |
Patient's |
Present Status |
|
|
|
|
|
|
|
Date Last Seen |
_ |
|||
|
o No evidence of disease |
|
|
|
|
|
|
|
|
|
||||
|
o Disease present but not progressing |
|
|
|
|
|
|
|||||||
|
o Disease not controlled |
|
|
|
|
|
|
|
|
|
||||
|
o Other Comments |
|
|
|
|
|
|
|
|
|
|
|||
|
a. |
Give present clinical and/or |
laboratory |
findings |
|
|
|
_ |
||||||
5. |
Give any other diagnoses known with |
the |
clinical and laboratory |
findings available |
_ |
|||||||||
|
Some advanced lesions are found to be surgically resectable after initial |
|||||||||||||
6. |
was the case, or if there are any other |
unusual aspects, please |
describe |
_ |
||||||||||