In the fast-paced world of emergency medical services, the Emergency Medical Technician Decision Tree Flow Chart stands as a crucial tool that guides first responders through the complexity of scene assessment and patient care. This form is designed to enhance quick and accurate decision-making in various situations, ensuring that Emergency Medical Technicians (EMTs) can swiftly evaluate a scene for safety, determine the nature and mechanism of an illness or injury, and identify the need for additional resources. It facilitates a systematic approach to trauma and medical patient assessment, incorporating steps to assess a patient's mental status, airway, breathing, circulation, and more, depending on the scenario's demands. Not only does the form guide in the initial assessment, but it also directs EMTs through focused history and physical exams, detailed physical exams based on the patient’s symptoms, and ongoing assessment to monitor changes in the patient's condition. With sections tailored to both trauma and medical emergencies, this decision tree emphasizes the importance of continuous reassessment and prioritizes effective communication and documentation between all parties involved in emergency care. Aimed at ensuring patient safety and enhancing care outcomes, this decision tree serves as a vital resource in emergency medical education and practice.
| Question | Answer |
|---|---|
| Form Name | Emergency Decision Tree Form |
| Form Length | 1 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 15 sec |
| Other names | emt initial assessment flowchart, medical emergencies flow charts printable, decision tree in an emergency, emt flow chart |
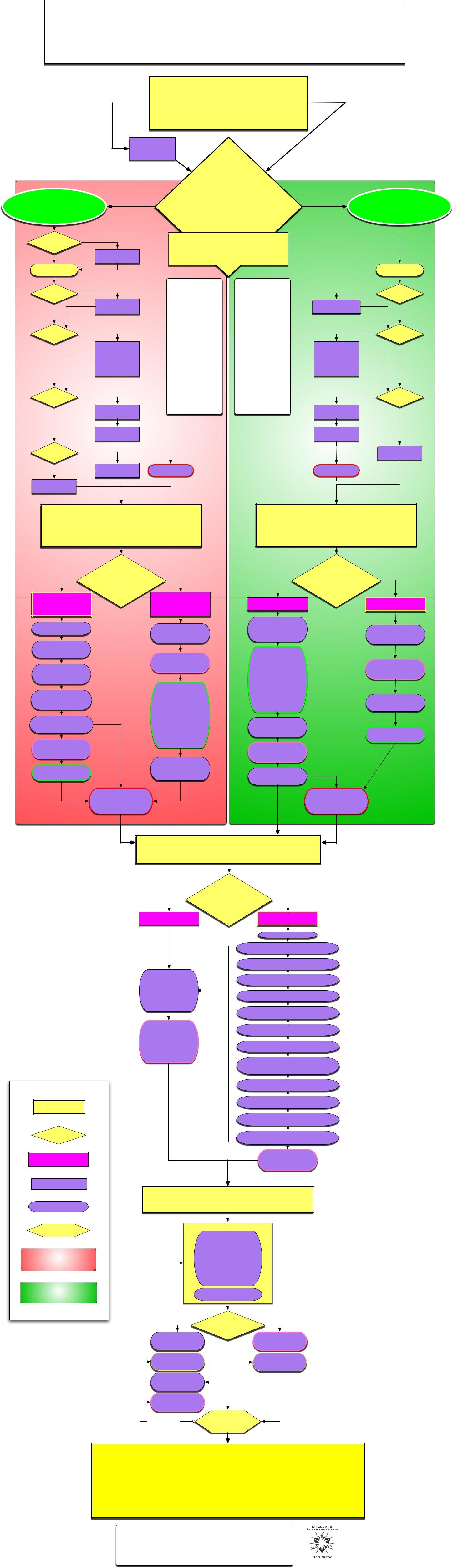
Emergency Medical Technician
Decision Tree Flow Chart
UNSAFE!
1 - SCENE
1)Take the necessary Body Substance Isolation precautions
2)Assure Scene Safety for rescuer, patient, and bystanders
3)Determine Mechanism of Injury or Nature of Illness
4)Establish Number of Patients
5)Need for Additional Resources
SAFE
TRAUMA
Patient
Control Scene
Move Patients
Correct Hazzard
2 -
INITIAL
MOI PATIENT ASSESSMENT
MED MEDICAL Patient
Suspect
Spinal Injury?
NO
Assess Mental Status (AVPU)
Assess
Airway
O
P
E
N
Assess
Breathing
A
D
E
Q
U
A
T
E
Assess
Circulation
P
U
L
S
E
Assess
Bleeding
NONE
ASSESS SKINS
P.M.S.
YES
Establish
Stabilization
CLOSED
Perform Jaw-
thrust Manuver
INADEQUATE
Begin Positive
Pressure
Ventilation with Supplemental Oxygen
NO PULSE
BEGIN CPR
APPLY AED
BLEEDING
CONTROL
BLEEDING
Form General Impression: Mechanism of Injury?
Look, Feel Skins, Listen Breathing, L.O.C.
DECIDE: TRAUMA, MEDICA, BOTH ?
(A,B,Cs, Bleed and Shock)
DECAP BTLS: |
SAMPLE: |
Deformity |
Signs and Symptoms, |
Evisceration |
Allergies, Medications, |
Contusion |
Past History, Last Oral |
Abrasion |
Intake, Environment |
Penetration |
|
Burns |
OPQRST: |
Tenderness |
Onset, Provocation, |
Lacerations |
Quality of pain, |
Swelling |
Radiation and Severity |
|
of pain, Time |
PMS: |
(Interventions) |
Pulse/Capalary Refil |
|
Motor Function |
PRBELLS: |
Sensation |
Pulse, Respiration, |
|
Blood Pressure, Eyes, |
PEARL: |
Lung Sounds, LOC, |
Pupils Equal And |
Skins |
Reactive to Light |
|
|
LOC: |
JVD: |
Level of |
Jugular Vein Distention |
Consciousness |
TRANSPORT
CLOSED
INADEQUATE
Begin Positive
Pressure
Ventilation with Supplemental Oxygen
NO PULSE
BEGIN CPR
APPLY AED
TRANSPORT
Assess Mental Status (AVPU)
Assess
Airway
O
P
E
N
Assess
Breathing
A
D
E
Q
U
A
T
E
Assess
Circulation
P
U
L
S
E
ASSESS SKINS
EYES
3 - Focused History and Physical Exam
3 - Focused History and Physical Exam
UNCONSCIOUS
or Obvious Injury RECONSIDER THE MECHANISM
OF INJURY
Significant MOI,
Mutiple Injuries, or
Altered Mental Status
Continue Inline
Stabilization
Continually
Reassess Mental
Status
Perform RAPID
Trauma
Assessment
Consider Advance
Life Support
Resources?
Reconsider PUAHA
Transport Decision?
Take Baseline
Vital Signs:
PRBELLS
Record SAMPLE
History:
TRANSPORT
ALERT &
Uninjured
No significant MOI,
Single injury, or
Alert Mental Status
Perform Focused
History and
Physical Exam
Take Baseline
Vital Signs:
PRBELLS
Record History:
Signs and
Symptoms,
Alergies,
Medications, Past
Mediacl History,
Last Oral Intake,
and any
Envioronmental
Conditions.
Perform Needed
Components of a
Detailed Physical
Exam
LOC 3+ |
CONSIDER |
|
|
|
|
|
|
MENTAL STATUS |
|
|
|
Responsive
Assess Complaints
Signs and
Symptoms (OPQRST)
Record History:
Signs and
Symptoms,
Alergies,
Medications, Past
Mediacl History,
Last Oral Intake,
and any
Envioronmental
Conditions.
Perform a Focused
Medical
Assessment
Take Baseline
Vital Signs:
PRBELLS
Consider Transport |
YES |
Decision? |
|
TRANSPORT
NO
Altered
Unresponsive
Perform a RAPID
Medical
Assessment
Take Baseline
Vital Signs:
PRBELLS
Position Patient
Record SAMPLE
History:
4 - Detailed Physical Exam
KEY
# Section
Decision
?
Symptom
ACTION
Alert
Responsive
Perform
Components of
Detailed Physical Exam based on patients's Injuries and Complaints
Reassess
Vital Signs:
Pulse, Respiration,
Blood Pressure,
Eyes, LOC, Last
Oral Intake, Skins
RECONSIDER Declining
MENTAL STATUS
Unresponsive
Position Patient
Assess the HEAD:
Feel for soft spots, DECAPBTLS
Assess the EARS:
Look for Fluid
Assess the FACE:
Look for Asymmetry: DECAPBTLS
Assess the EYES:
PEARL, Colors, Symmetry
Assess the NOSE:
Fluid, Symmetry, Air flow
Assess the MOUTH:
Teeth, Tung, Lips, Throat
Assess the NECK:
JVD, Tracheal Deviation,
Assess the CHEST:
Paradoxical Movement,
DECAPBTLS
Assess the ABDOMEN:
Assess the PELVIS:
Asymmetrical movement, Genitals
Assess the EXTREMITIES:
PMS, DECAPBTLS, Asymmetry
Assess the POSTERIOR BODY:
Spinal line, DECAPBTLS
Reassess
Vital Signs:
PRBELLS
Procedure
Loop
TRAUMA AREA
MEDICAL AREA
5 - Ongoing Assessment
REPEAT INITIAL ASSESSMENT
REASSESS:
General Impression,
Mental Status, Airway,
Breathing Rate and
Quality, Circulation;
Pulse Rate and
Quality, Skin Color,
Temperature,
Condition, Bleeding.
Reestablish
Patient Priority
Worse |
Change in |
Stable |
|
Patient Condition? |
|
Repeat Focused |
|
Reassess |
History and |
|
|
|
Vital Signs |
|
Physical Exam |
|
|
|
|
|
Provide |
|
Reassess |
Emergency Care |
|
Emergency Care |
Assess |
|
|
Effectiveness of |
|
|
Emergency Care |
|
|
Reassess |
|
|
Vital Signs |
|
|
|
REPEAT |
|
Every 5 min. |
Ongoing |
|
|
Assessment |
|
6 - Communication and Documentation
During your call you will communicate, at important points, with dispatch and with medical direction as well as with the staff of the medical facility to which you transport the patient. You must also communicate clearly with other EMS personnel, the patient, and others at the scene. A failure of clear communication - both in what they communicate to you or in what you communicate to others - can have a significant effect upon the quality of assessment and care you and others provide.
In addition a significant portion of the value of patient assessment and care is lost if what you have learned about the patient's condition and the care you have given are not clearly and adequately documented in written reports.
EMERGENCY MEDICAL TECHNITION DECISION TREE
AND
A PRODUCT OF LIFEGUARD ADVENTURES.COM, COPYRIGHT 2007
1666 GARNET, #619, SAN DIEGO, CA 92109
(619)