DENIALS can be filled out online easily. Just use FormsPal PDF tool to accomplish the job without delay. The tool is consistently maintained by our team, getting cool features and growing to be better. This is what you'd have to do to begin:
Step 1: Hit the "Get Form" button above on this webpage to open our PDF editor.
Step 2: When you access the PDF editor, you will see the document made ready to be completed. Aside from filling out various blank fields, you may also perform other sorts of actions with the form, specifically putting on custom textual content, editing the initial textual content, inserting graphics, putting your signature on the form, and much more.
So as to finalize this PDF document, be certain to provide the information you need in each and every area:
1. The DENIALS involves particular information to be entered. Make sure the next blank fields are filled out:
2. Given that the last array of fields is complete, you need to add the required details in Medicaid pays only Medicare Part A, Medicaid pays only your Medicare, Medicaid pays for only limited, Retroactive Medicaid coverage is, If you receive Medicare Medicare, The State rules used to make this, DENIALS, Medicaid, Special AssistanceAdult Care Home, Special AssistanceInhome, is denied from to because, The State rules used to make this, HEARING RIGHTS If you disagree, number below within days to ask, and day is If you do not ask for a so that you can progress further.
People frequently get some things wrong when filling in Medicaid pays only your Medicare in this part. Be certain to re-examine everything you type in here.
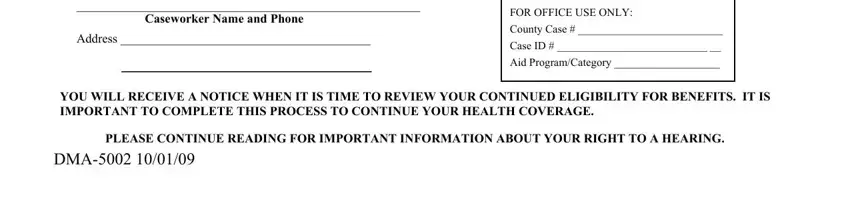
3. This third part will be easy - fill out all the empty fields in Caseworker Name and Phone, Address, FOR OFFICE USE ONLY, County Case, Case ID, Aid ProgramCategory, YOU WILL RECEIVE A NOTICE WHEN IT, PLEASE CONTINUE READING FOR, and DMA in order to complete the current step.
Step 3: When you have glanced through the details in the blanks, simply click "Done" to conclude your form. Make a 7-day free trial subscription with us and obtain instant access to DENIALS - download or edit inside your personal account. At FormsPal.com, we do our utmost to guarantee that all of your information is maintained private.