Working with PDF files online is definitely a piece of cake using our PDF tool. You can fill out bcbs ohio prior authorization form here and use several other functions available. We at FormsPal are committed to providing you the perfect experience with our tool by continuously introducing new features and upgrades. Our editor has become much more helpful with the newest updates! At this point, editing PDF files is simpler and faster than ever. Here's what you would want to do to get going:
Step 1: Hit the "Get Form" button above. It will open our pdf tool so that you could begin filling out your form.
Step 2: When you open the editor, there'll be the form made ready to be filled in. Apart from filling out various blanks, it's also possible to perform other sorts of things with the file, particularly adding custom textual content, editing the original textual content, adding images, putting your signature on the document, and much more.
It is actually straightforward to fill out the form with our detailed tutorial! Here's what you have to do:
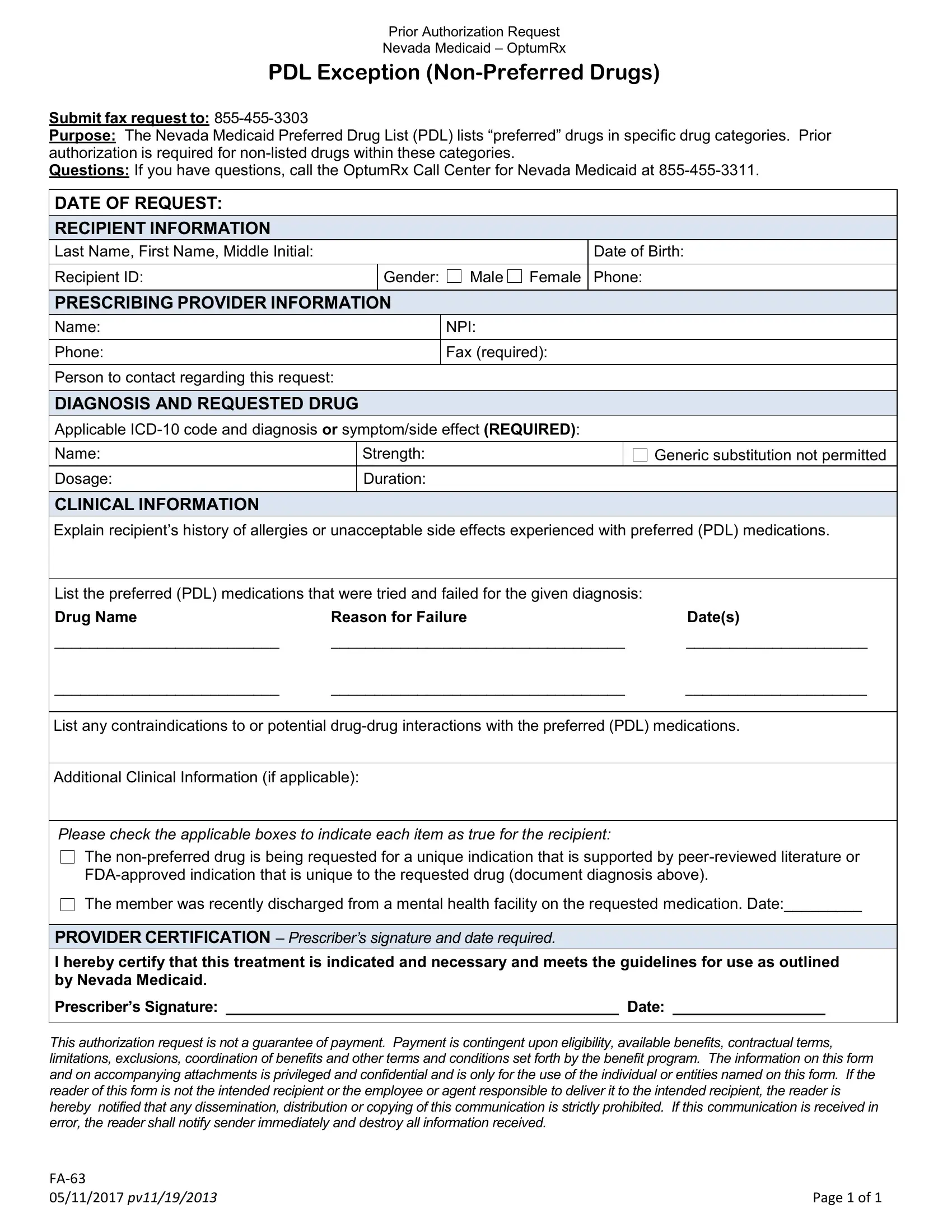
1. Whenever completing the bcbs ohio prior authorization form, make certain to include all essential blank fields within its relevant area. It will help hasten the process, allowing for your details to be processed promptly and properly.
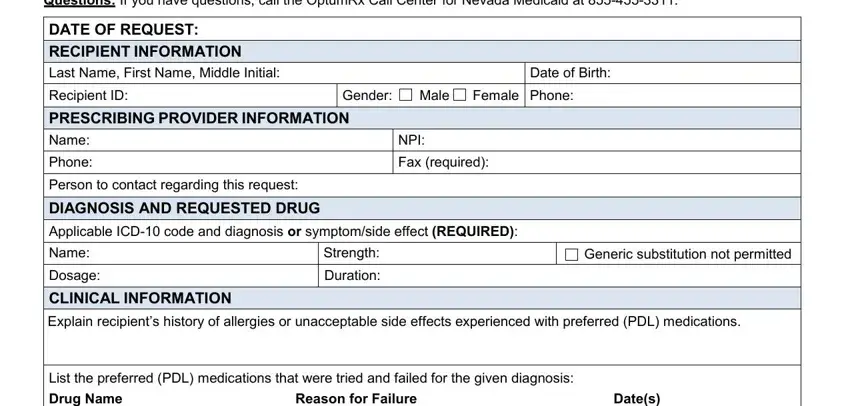
2. When the last segment is finished, you should insert the necessary specifics in Drug Name, Reason for Failure, Dates, List any contraindications to or, Additional Clinical Information if, Please check the applicable boxes, The nonpreferred drug is being, The member was recently discharged, PROVIDER CERTIFICATION, Date, and This authorization request is not so that you can move forward to the third step.
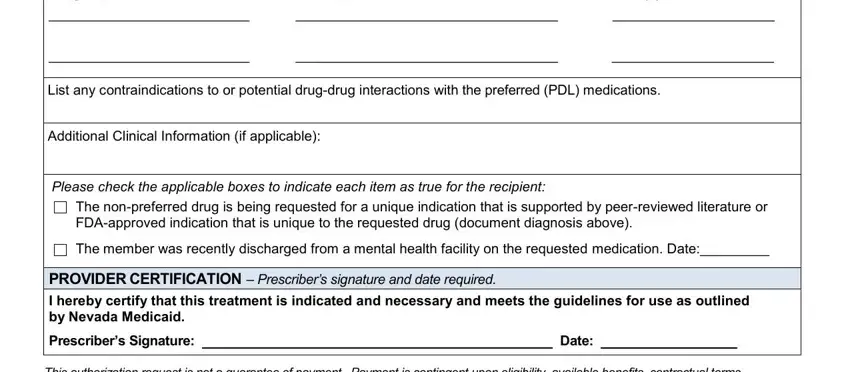
Many people often make mistakes when completing Please check the applicable boxes in this part. You should definitely review everything you type in here.
Step 3: Prior to moving forward, ensure that all blank fields were filled in the correct way. The moment you think it's all fine, click “Done." Right after creating afree trial account at FormsPal, it will be possible to download bcbs ohio prior authorization form or email it at once. The PDF form will also be available via your personal account menu with your every single edit. With FormsPal, you're able to complete documents without worrying about information breaches or entries being shared. Our secure software helps to ensure that your personal details are stored safely.