When families and individuals face the decision of transitioning into an assisted living facility, the Missouri Department of Health and Senior Services provides a structured pathway through the MO 580-2835 form. This document is a critical tool in assessing a potential resident's eligibility and needs for assisted living care. Divided into two main sections, pre-screening and resident assessment, the form offers a comprehensive review of a person's current living situation, health status, and daily living capabilities. Pre-screening touches on essential data like the person's name, address, and social security number, alongside initial inquiries into their ability to contribute to the assessment, mobility restrictions, and any behavior that could affect their fit for an assisted living environment. Following this, the resident assessment delves deeper, evaluating personal care needs, dietary requirements, mobility, mental and behavioral conditions, medical needs, and more. Integral to this process is the assessment's role in developing an individualized service plan, tailored to support the resident’s health and well-being within the facility. This thoughtful approach ensures that individuals are placed in an environment that not only meets their physical needs but also fosters a sense of community and belonging.
| Question | Answer |
|---|---|
| Form Name | Form Mo 580 2835 |
| Form Length | 4 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 1 min |
| Other names | from assisted mo, assessment assisted living printable, facility assessment mo, mo 580 2835 |
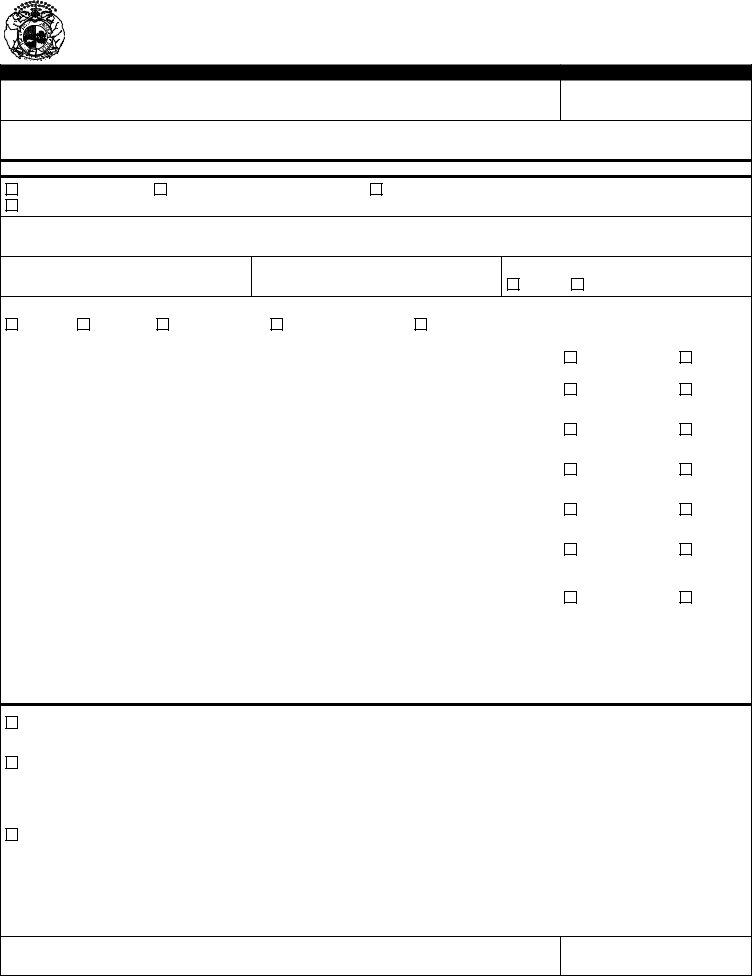
MISSOURI DEPARTMENT OF HEALTH AND SENIOR SERVICES
DIVISION OF REGULATION AND LICENSURE
SECTION FOR
PART I -
NAME (FIRST, MIDDLE, LAST)
SOCIAL SECURITY NUMBER
ADDRESS (STREET, CITY, STATE, ZIP)
PERSON IS CURRENTLY
Living Independently
Living in Residential Care Facility
Hospitalized
Other ______________________________________________________
COMMENTS
TELEPHONE
MARITAL STATUS
DOB
SEX
Male
Female
Single
Married
Never Married
Divorced/Separated
Widow(er)
Resident able to participate in providing above information? |
YES |
NO |
|
|
|
|
|
Resident |
YES |
NO |
|
Disqualify |
Qualify |
||
|
|||
|
|
|
|
Has the resident exhibited behaviors that present a reasonable likelihood of serious harm to self or |
YES |
NO |
|
others? |
Disqualify |
Qualify |
|
|
|||
|
|
|
|
Resident requires a physical restraint? |
YES |
NO |
|
Disqualify |
Qualify |
||
|
|||
|
|
|
|
Resident uses a medication as a chemical restraint? (medication not used to treat a medical |
YES |
NO |
|
condition) |
Disqualify |
Qualify |
|
|
|||
|
|
|
|
Resident requires more than one person to simultaneously physically assist with any activities of |
YES |
NO |
|
daily living other than bathing and/or transferring? |
Disqualify |
Qualify |
|
|
|||
|
|
|
|
Resident has a condition that requires skilled nursing services? If yes, please list: |
YES |
NO |
|
|
|||
|
|
|
TO BE DETERMINED BY PERSON DOING RESIDENT ASSESSMENT
Yes |
Resident meets criteria for admission to Assisted Living Facility. Proceed to complete a community based assessment using the |
|
attached or a form which has received prior approval from the Section for Long Term Care Regulation. |
Yes |
Resident meets criteria for admission to Assisted Living Facility which provides services to residents with a physical, cognitive or |
|
other impairment that prevents the resident from safely evacuating the facility with minimal assistance. Proceed to complete a com- |
|
munity based assessment using the attached or a form which has received prior approval from the Section for Long Term |
|
Care Regulation. |
No |
Resident is not eligible for admission to an Assisted Living Facility. |
INTERVIEWER NAME
DATE
MO |
PAGE 1 |
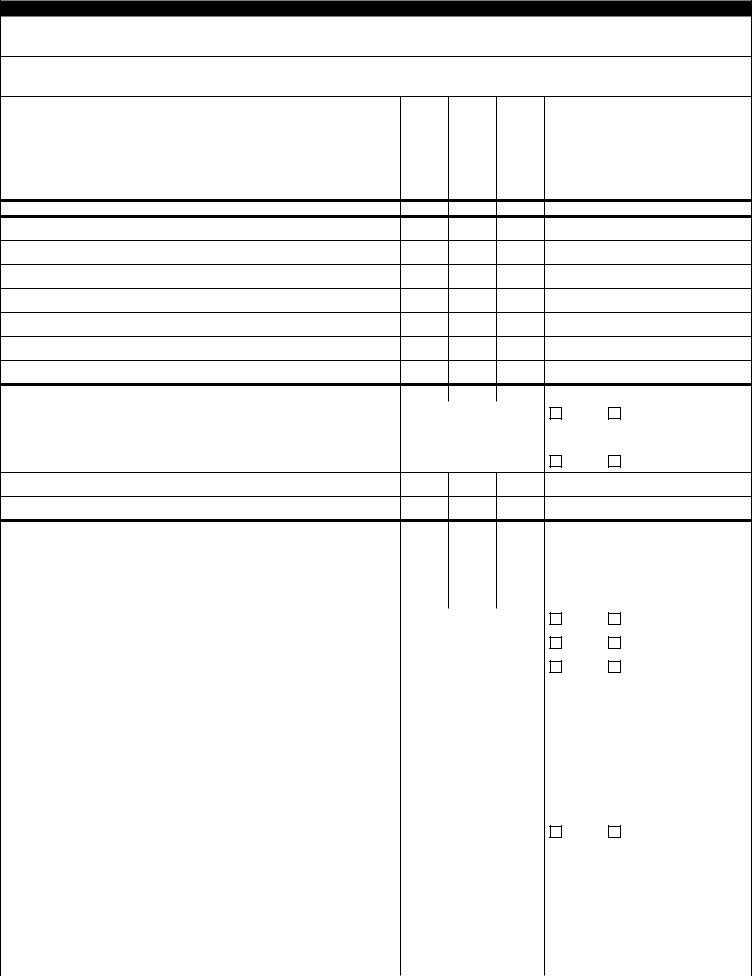
PART II - RESIDENT ASSESSMENT (COMPLETED WITHIN 5 DAYS OF ADMISSION TO ASSISTED LIVING FACILITY)
RESIDENT NAME
RESPONDENT NAME
PERFORMS INDEPENDENTLY |
SOME ASSISTANCE |
TOTALLY DEPENDENT |
COMMENTS |
|
|
|
PERSONAL CARE - Grooming/Bathing
Bathing
Dental/Mouth Care
Hair Care
Shaving
Toe/Fingernail Care
PERSONAL CARE - Toileting |
|
|
|
|
|
|
Bladder/Bowel Control |
|
|
|
|
Yes |
No |
|
|
|
|
|
|
|
Special Equipment Required (List: |
) |
|
|
|
|
|
|
|
|
|
|
|
|
Catheter/Ostomy |
|
|
|
|
Yes |
No |
|
|
|
|
|
|
|
DIETARY |
|
|
|
|
|
Eats Meals Daily |
|
|
|
|
|
|
|
|
|
|
|
Meal Preparation |
|
|
|
|
|
|
|
|
|
|
|
Chewing/Swallowing |
|
|
|
|
|
|
|
|
|
|
|
Recent Weight Loss/Gain |
|
|
|
Yes |
No |
|
|
|
|
|
|
Uses Feeding Tubes/Devices Calculated Diet Prescribed |
|
|
|
Yes |
No |
|
|
|
|
|
|
Special Diet Followed |
|
|
|
Yes |
No |
|
|
|
|
|
|
|
|
|
|
|
|
MOBILITY |
|
|
|
|
|
Ambulatory - Able to Get Around |
|
|
|
|
|
|
|
|
|
|
|
Transfer To/From Bed |
|
|
|
|
|
|
|
|
|
|
|
Transfer To/From Chair |
|
|
|
|
|
|
|
|
|
|
|
Transfer To/From Wheelchair |
|
|
|
|
|
|
|
|
|
|
|
Safely evacuates the facility with minimal assistance. |
|
|
|
Yes |
No |
|
|
|
|
||
|
|
|
|
|
|
HOUSEKEEPING |
|
|
|
|
|
Cleans Bedroom, Bathroom, Kitchen |
|
|
|
|
|
|
|
|
|
|
|
Laundry |
|
|
|
|
|
|
|
|
|
|
|
Make/Change Beds |
|
|
|
|
|
|
|
|
|
|
|
Empty Trash |
|
|
|
|
|
|
|
|
|
|
|
MO |
PAGE 2 |
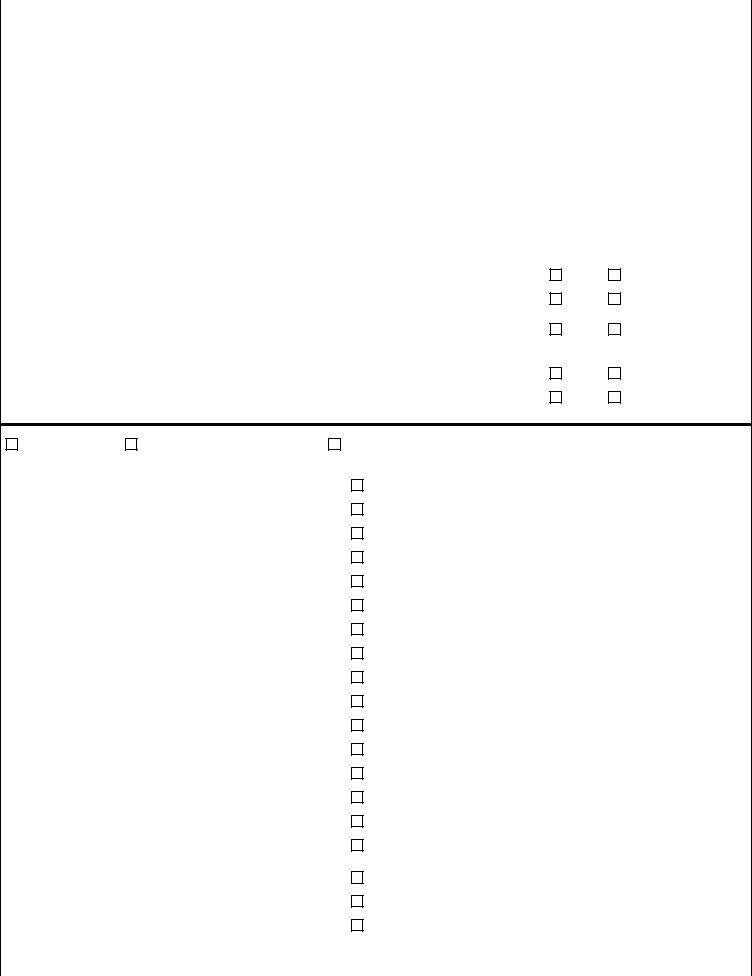
|
WELL ORIENTED |
SOME MEMORY LAPSE |
NEEDS ASSISTANCE |
|
COMMENTS |
|
|
|
|||
|
|
|
|
|
|
BEHAVIOR/MENTAL CONDITION |
|
|
|
|
|
Orientation to Date, Day, and Place |
|
|
|
|
|
|
|
|
|
|
|
Wanders or confusion |
|
|
|
|
|
|
|
|
|
|
|
Memory/Recall |
|
|
|
|
|
|
|
|
|
|
|
Judgment |
|
|
|
|
|
|
|
|
|
|
|
Follows Instructions |
|
|
|
|
|
|
|
|
|
|
|
Sociability |
|
|
|
|
|
|
|
|
|
|
|
Sad or Anxious Mood |
|
|
|
Yes |
No |
|
|
|
|
|
|
Socially Inappropriate/Disruptive Behavior |
|
|
|
Yes |
No |
|
|
|
|
|
|
Diagnosed or Treatment History for Mental Illness or Developmental |
|
|
|
Yes |
No |
Disability |
|
|
|
||
|
|
|
|
|
|
TRANSPORTATION |
|
|
|
|
|
Can drive self |
|
|
|
Yes |
No |
|
|
|
|
|
|
Can leave the facility with assistance |
|
|
|
Yes |
No |
|
|
|
|
|
|
MEDICAL NEEDS/SUPPORTS/MONITORING
RESIDENT CAN
Self Administer |
Needs Assistance taking meds |
Totally dependent |
|
|
|
|
|
|
|
|
|
Health Problems (Check All That Currently Apply) |
|
Prescription Meds |
Dosage |
Physician/Pharmacy |
|
Anemia |
|
|
|
|
|
|
|
|
|
|
|
Arthritis and other joint limitations or injuries |
|
|
|
|
|
|
|
|
|
|
|
Bowel/bladder problems |
|
|
|
|
|
|
|
|
|
|
|
Cancer, Leukemia or tumor |
|
|
|
|
|
|
|
|
|
|
|
Dementia (OBS, Alzheimer’s, Huntington’s, Pick’s) |
|
|
|
|
|
|
|
|
|
|
|
Diabetes |
|
|
|
|
|
|
|
|
|
|
|
Digestive disorders (ulcers, diverticulosis) |
|
|
|
|
|
|
|
|
|
|
|
Edema |
|
|
|
|
|
|
|
|
|
|
|
Effects of stroke (CVA, TIA, memory loss) |
|
|
|
|
|
|
|
|
|
|
|
Effects of osteoporosis or fractures |
|
|
|
|
|
|
|
|
|
|
|
Hardening of arteries (ASHD, poor circulation) |
|
|
|
|
|
|
|
|
|
|
|
Hearing impairment (H.O.H., deafness) |
|
|
|
|
|
|
|
|
|
|
|
Heart trouble (angina, CHF, MI) |
|
|
|
|
|
|
|
|
|
|
|
Hypertension |
|
|
|
|
|
|
|
|
|
|
|
Respiratory problems (asthma, emphysema, COPD) |
|
|
|
|
|
|
|
|
|
|
|
Skin problems (decubitus ulcer, lesions, rashes) |
|
NON PRESCRIPTION MEDICATIONS |
|
||
|
|
|
|
||
|
|
|
|
|
|
Surgery with residual effects (drainage, amputation, paralysis, |
|
|
|
|
|
pain, fatigue) |
|
|
|
|
|
|
|
|
|
|
|
Tremors (Parkinson’s) |
|
|
|
|
|
|
|
|
|
|
|
Visual impairment (cataracts, glaucoma, blindness) |
|
|
|
|
|
|
|
|
|
|
|
OTHER (PLEASE LIST:) |
|
|
|
|
|
|
|
|
|
|
|
MO |
PAGE 3 |
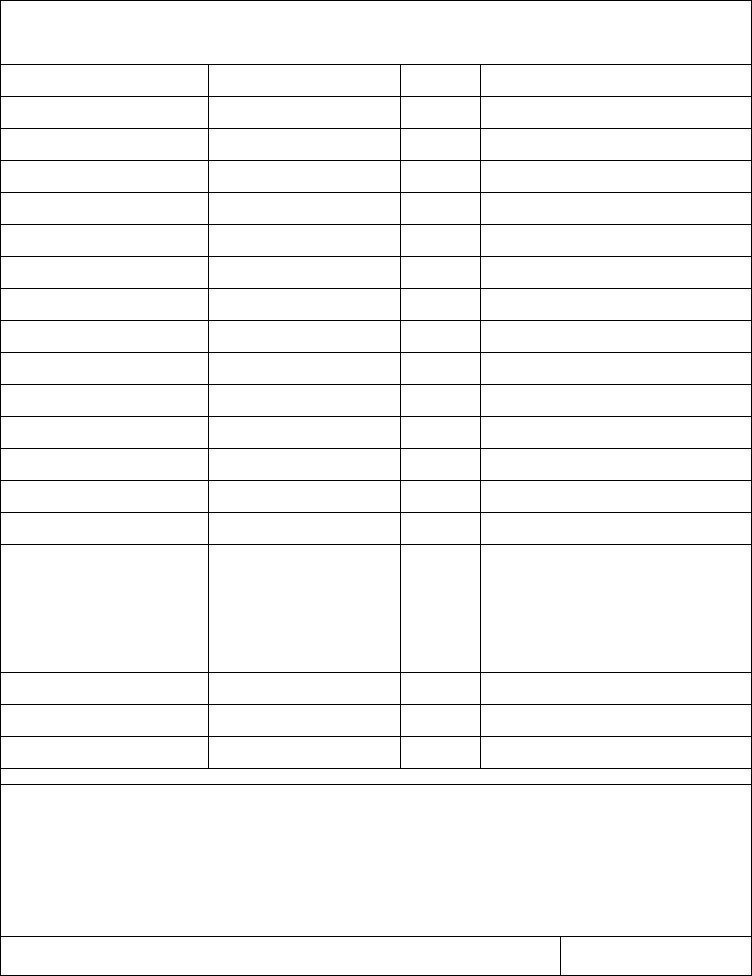
List all physicians/clinics and other health providers.
State the condition for which the health provider is being seen, the frequency of contact, and describe what is being done (the procedure to monitor the condition.
DOCTOR/CLINIC NAME
CONDITION
FREQUENCY
PROCEDURE
HOME HEALTH AGENCY NAME |
CONDITION |
FREQUENCY |
PROCEDURE |
|
|
|
|
|
|
|
|
|
|
|
|
OTHER HEALTH CARE PROVIDER |
CONDITION |
FREQUENCY |
PROCEDURE |
THIS ASSESSMENT FORM SHOULD BE USED TO DEVELOP THE INDIVIDUAL SERVICE PLAN FOR RESIDENT.
COMMENTS
INTERVIEWER NAME
DATE
MO |
PAGE 4 |