The Adult Care Home Personal Care Physician Authorization and Care Plan is a comprehensive document designed to ensure that residents of adult care homes receive the personalized care they need and deserve. At the core of this form is the resident's health assessment, which evaluates everything from medication needs, mental health and social history, to the finer points of daily living assistance requirements. These include mobility, nutrition intake, skin care, and more. Critical to the form is the need for detailed communication between the care facility and the resident's physician, ensuring that all medical diagnoses and the necessary personal care services are accurately documented and authorized. Besides medical aspects, the form also touches on important areas such as the resident's ability to perform daily living activities (ADLs), which covers eating, toileting, and grooming, among others. Each task is carefully assessed to determine the level of assistance required, demonstrating a thorough planning process aimed at providing tailored care. This process not only ensures the resident's health and safety but also respects their dignity and independence as much as possible. The ultimate goal is to create a supportive environment where residents can maintain the highest quality of life.
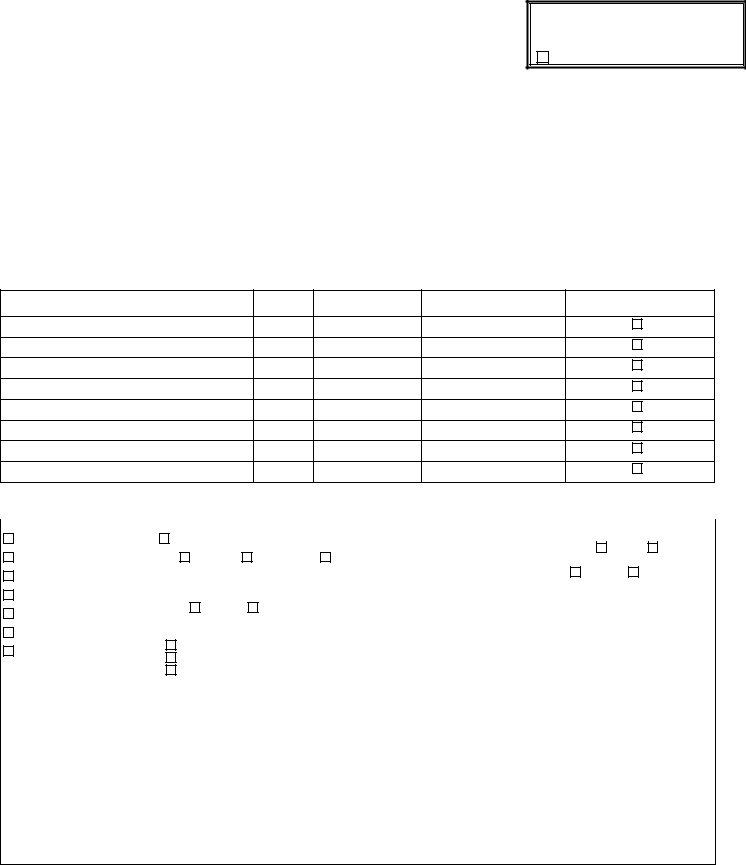
| Question | Answer |
|---|---|
| Form Name | Form Personal Care |
| Form Length | 5 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 1 min 15 sec |
| Other names | personal physician authorization, printable inservices for caregivers, care physician authorization, form personal care |
ADULT CARE HOME
PERSONAL CARE PHYSICIAN AUTHORIZATION AND CARE PLAN
Assessment Date ___/___/___
Reassessment Date ___/___/___
Significant Change___/___/___
RESIDENT INFORMATION
(Please Print or Type)
RESIDENT _________________________________________ SEX (M/F) ____ DOB ____/____/____ MEDICAID ID NO. __________________________
FACILITY ____________________________________________________________________________________________________________________________
ADDRESS ___________________________________________________________________________________________________________________________
___________________________________________________________________PHONE ___________________ PROVIDER NUMBER __________________
DATE OF MOST RECENT EXAMINATION BY RESIDENT’S PRIMARY CARE PHYSICIAN ______/______/______
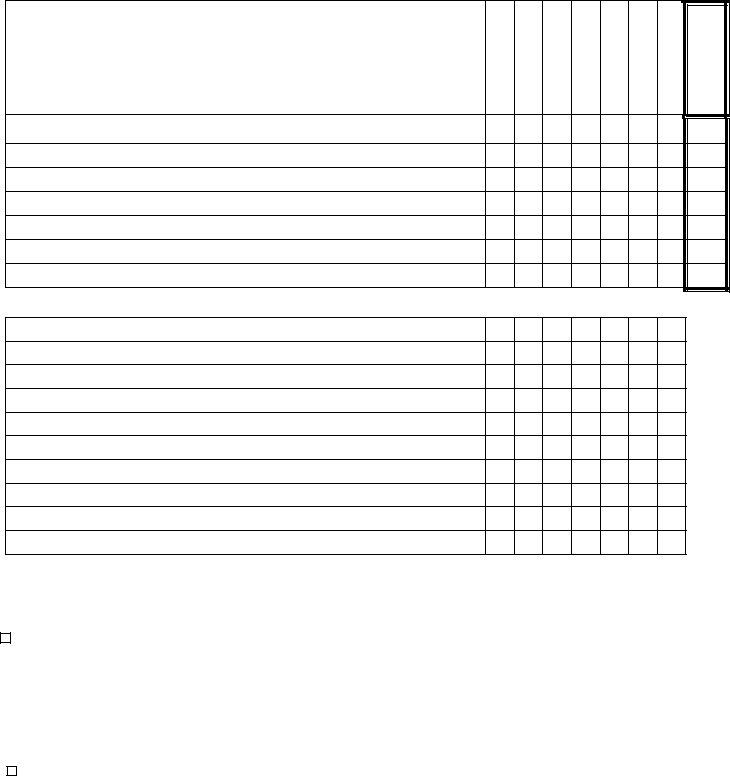
ASSESSMENT
1. MEDICATIONS – Identify and report all medications, including
Name
Dose
Frequency
Route
() If
2.MENTAL HEALTH AND SOCIAL HISTORY: (If checked, explain in “Social/Mental Health History” section)
Wandering |
Injurious to: |
|
|
Is the resident currently receiving Mental Health, DD, or |
||
|
|
Substance Abuse Services (SAS)? |
YES |
NO |
||
|
|
|
|
|||
Verbally Abusive |
Self |
Others |
Property |
|
|
|
Physically Abusive |
|
|
|
Has a referral been made? |
YES |
NO |
Is the resident currently receiving |
|
|
|
|
||
|
|
|
|
|
||
Resists care |
medication(s) for mental illness/behavior? |
If YES: |
|
|
||
Suicidal |
YES |
NO |
|
|
|
|
|
|
|
Date of Referral _________________ |
|
||
|
|
|
|
|
||
Homicidal |
Is there a history of: |
|
Name of Contact Person _____________________________ |
|||
Disruptive Behavior/ |
Substance Abuse |
|
||||
Developmental Disabilities (DD) |
|
|
|
|||
|
Agency ______________________________________________ |
|||||
Socially Inappropriate |
Mental Illness |
|
|
|||
|
|
|
|
|
||
|
|
|
|
|
|
|
Social/Mental Health History: ________________________________________________________________________________________________
______________________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________________
Resident __________________________________
3.AMBULATION/LOCOMOTION: No Problems Limited Ability Ambulatory w/ Aide or Device(s)
|
Has device(s): |
Does not use |
Needs repair or replacement |
|
|
|
|
|
||
4. |
UPPER EXTREMITIES: |
No Problems |
Limited Range of Motion |
Limited Strength |
Limited |
|||||
|
Specify affected joint(s) _________________________________________________________________ |
Right |
Left |
Bilateral |
||||||
|
Other impairment, specify __________________________________________________________________________________________________ |
|||||||||
|
_______________________________________________________________________________________________________________________________ |
|||||||||
|
Device(s) Needed ____________________________________________ Has device(s): |
Does not use |
Needs repair or replacement |
|||||||
5. |
NUTRITION: |
Oral |
Tube (Type) ______________________________________ Height __________________ Weight __________________ |
|||||||
|
Dietary Restrictions: ___________________________________________________________________________________________________________ |
|||||||||
|
________________________________________________________________________________________________________________________________ |
|||||||||
|
________________________________________________________________________________________________________________________________ |
|||||||||
|
________________________________________________________________________________________________________________________________ |
|||||||||
|
Device(s) Needed _______________________________________________________________________________________________________________ |
|||||||||
|
Has device(s): |
Does not use |
Needs repair or replacement |
|
|
|
|
|
||
6. RESPIRATION: |
Normal |
Well Established Tracheostomy |
Oxygen |
Device(s) Needed _____________________________________________ Has device(s):
Shortness of Breath
Does not use |
Needs repair or replacement |
7.SKIN: Normal Pressure Areas Decubiti Other _______________________________________________________________
Skin Care Needs ______________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________________
8. |
BOWEL: |
Normal |
Occasional Incontinence (less than daily) |
Daily Incontinence |
|||
|
Ostomy: Type ______________________________________________________________ |
||||||
9. |
BLADDER: |
|
Normal |
Occasional Incontinence (less than daily) |
Daily Incontinence |
||
|
Catheter: Type _________________________________________________________________ |
||||||
10. |
ORIENTATION: |
Oriented |
Sometimes Disoriented |
Always Disoriented |
|||
YES
YES
NO
NO
11. |
MEMORY: |
Adequate |
Forgetful – Needs Reminders |
Significant Loss – Must Be Directed |
|||
12. |
VISION: |
Adequate for Daily Activities |
|
Limited (Sees Large Objects) |
Very Limited (Blind); Explain___________________ |
||
|
Uses: |
Glasses |
Contact Lens |
Needs repair or replacement |
|
||
|
Comments ___________________________________________________________________________________________________________________ |
||||||
|
______________________________________________________________________________________________________________________________ |
||||||
13. |
HEARING: |
Adequate for Daily Activities |
Hears Loud Sounds/Voices |
Very Limited (Deaf); Explain _________________ |
|||
|
Uses Hearing Aid(s) |
Needs repair or replacement |
|
|
|||
|
Comments ___________________________________________________________________________________________________________________ |
||||||
14. SPEECH/COMMUNICATION METHOD: |
Normal |
Slurred |
Weak |
Other Impediment |
|||
Gestures |
Sign Language |
Writing |
Foreign Language Only ________________________ |
||||
Assistive Device(s) (Type _____________________________________) |
Has device(s): Does not use |
||||||
No Speech
Other None
Needs repair or replacement
Resident _______________________________________
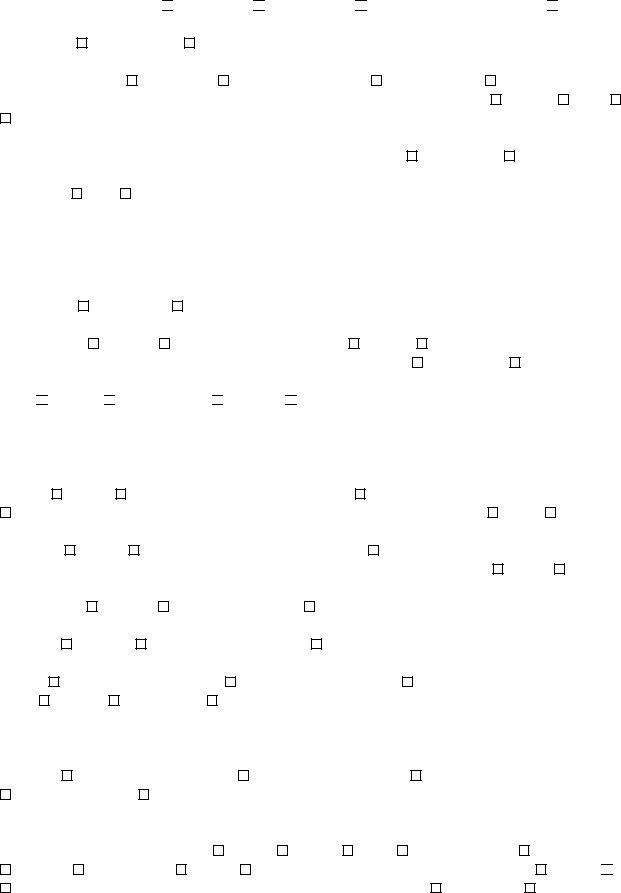
CARE PLAN
15.IF THE ASSESSMENT INDICATES THE RESIDENT HAS MEDICALLY RELATED PERSONAL CARE NEEDS REQUIRING ASSISTANCE, SHOW THE PLAN FOR PROVIDING CARE. CHECK OFF THE DAYS OF THE WEEK EACH ADL TASK IS PERFORMED AND RATE EACH ADL TASK BASED ON THE FOLLOWING PERFORMANCE CODES: 0 - INDEPENDENT,
1 - SUPERVISION, 2 - LIMITED ASSISTANCE, 3 - EXTENSIVE ASSISTANCE, 4 - TOTALLY DEPENDENT. (PLEASE REFER TO
YOUR ADULT CARE HOME PROGRAM MANUAL FOR MORE DETAIL ON EACH PERFORMANCE CODE.)
ACTIVITIES OF DAILY LIVING (ADL) |
|
|
|
WEDNESDAY |
|
|
|
DESCRIBE THE SPECIFIC TYPE OF ASSISTANCE NEEDED BY THE RESIDENT AND |
SUNDAY |
MONDAY |
TUESDAY |
THURSDAY |
FRIDAY |
SATURDAY |
|
PROVIDED BY STAFF, NEXT TO EACH ADL: |
|
|
|
|
|
|
|
EATING
TOILETING
AMBULATION/LOCOMOTION
BATHING
DRESSING
GROOMING/PERSONAL HYGIENE
TRANSFERRING
OTHER: (Include Licensed Health Professional Support (LHPS) Personal Care Tasks, as listed in Rule 42C .3703, and any other special care needs)
PERFORMANCE CODE
ASSESSOR CERTIFICATION
I certify that I have completed the above assessment of the resident’s condition. I found the resident needs personal care services due to the resident’s medical condition. I have developed the care plan to meet those needs.
Resident/responsible party has received education on Medical Care Decisions and Advance Directives prior to admission.
__________________________________________ |
______________________________________________ |
____________________ |
Name |
Signature |
Date |
PHYSICIAN AUTHORIZATION
I certify that the resident is under my care and has a medical diagnosis with associated physical/mental limitations warranting the provision of the personal care services in the above care plan.
The resident may take therapeutic leave as needed.
_________________________________________ |
_____________________________________________ |
_____________________ |
Name |
Signature |
Date |
INSTRUCTIONS FOR COMPLETING THE REVISED ADULT CARE HOME PERSONAL CARE PHYSICIAN AUTHORIZATION AND CARE PLAN
The block in the upper right hand corner of the form denotes the type of assessment that is completed: Include Assessment date, Reassessment date, or Significant Change. Refer to the glossary in the Adult Care Home Services manual for the definition of significant change.
RESIDENT INFORMATION: In the Resident Information area include the resident’s name as it appears on the blue Medicaid ID card. Complete all information.
DATE OF MOST RECENT EXAMINATION: Includes a yearly physical by the resident’s attending physician.
ASSESSMENT:
1.MEDICATIONS: List the name of each medication, include
2.MENTAL HEALTH AND SOCIAL HISTORY: Identify by checking the appropriate box. Review records from discharging facility to monitor if there was any indication about history of injury to self, property, or others. Include meds for mental illness/behavior, and include if there is a history of Mental Illness, Developmental Disabilities, or Substance Abuse.
•Is the resident currently receiving Mental Health (MH), Developmental Disabilities (DD), or Substance Abuse Services (SAS)? If a referral has been made for an evaluation, indicate the date of referral, name of contact person at the agency, and the agency name.
•Social/Mental Health History: Include any history that can be gathered from assessment by the resident, family, friends, etc. that provide information about the resident’s preferences, activities and living status. This is also an area that needs to identify any Mental Health history such as institutionalization, out patient, compliance history, police record, etc.
TOP OF SECOND PAGE: RESIDENT_________________: Place name as on Medicaid ID card in this blank.
3.AMBULATION/LOCOMOTION: Check applicable block and list devices needed.
4.UPPER EXTREMITIES: Check applicable box and list devices needed.
5.NUTRITION: Check appropriate box. Indicate height and weight. Include any restrictions to diet, i.e. NAS, soft, etc.
6.RESPIRATION: Check appropriate box. Indicate any devices needed.
7.SKIN: Check appropriate box. Explain in detail treatment necessary and include any MD orders for skin care.
8.BOWEL: Check appropriate box. Indicate if the resident is independent of activity. Explain what resident needs from staff.
9.BLADDER: Check appropriate box. Indicate if the resident is independent of activity. Explain what residents need from staff.
10.ORIENTATION: Check appropriate box.
11.MEMORY: Check appropriate box.
12.VISION: Check appropriate box. Expand on concerns in comments area.
13.HEARING: Check appropriate box. Expand on concerns in comments area.
14.SPEECH/COMMUNICATION METHOD: Check appropriate box.
TOP OF THIRD PAGE: RESIDENT__________________: Place name as on Medicaid ID card in this
blank.
CARE PLAN:
15.Refer to the Adult Care Home Services manual for more detail on Performance Codes.
ACTIVITIES OF DAILY LIVING: Include a description of the specific type of assistance provided by staff next to each ADL and code the activity in the Performance Code area. In Other, list any Licensed Health Professional Support tasks as well as any special care needs in this area.
ASSESSOR CERTIFICATION: Check box for Medical Care Decisions and Advance Directives education. Signature of assessor certifies that the care plan is developed based on assessment findings.
PHYSICIAN AUTHORIZATION: The form is forwarded to the attending physician. The physician’s authorization certifies that the individual is under the physician’s care and has a medical diagnosis that warrants the provision of personal care services as indicated in the care plan. The physician prints his/her name, signs, and dates the form. The physician also may indicate and provide standing orders for an individual to take therapeutic leave by checking the block.