This PDF editor was created to be as clear as it can be. Once you comply with these steps, the procedure for filling out the head to toe assessment pdf file is going to be simple and easy.
Step 1: Initially, choose the orange button "Get Form Now".
Step 2: Now you are on the document editing page. You can edit, add information, highlight particular words or phrases, place crosses or checks, and insert images.
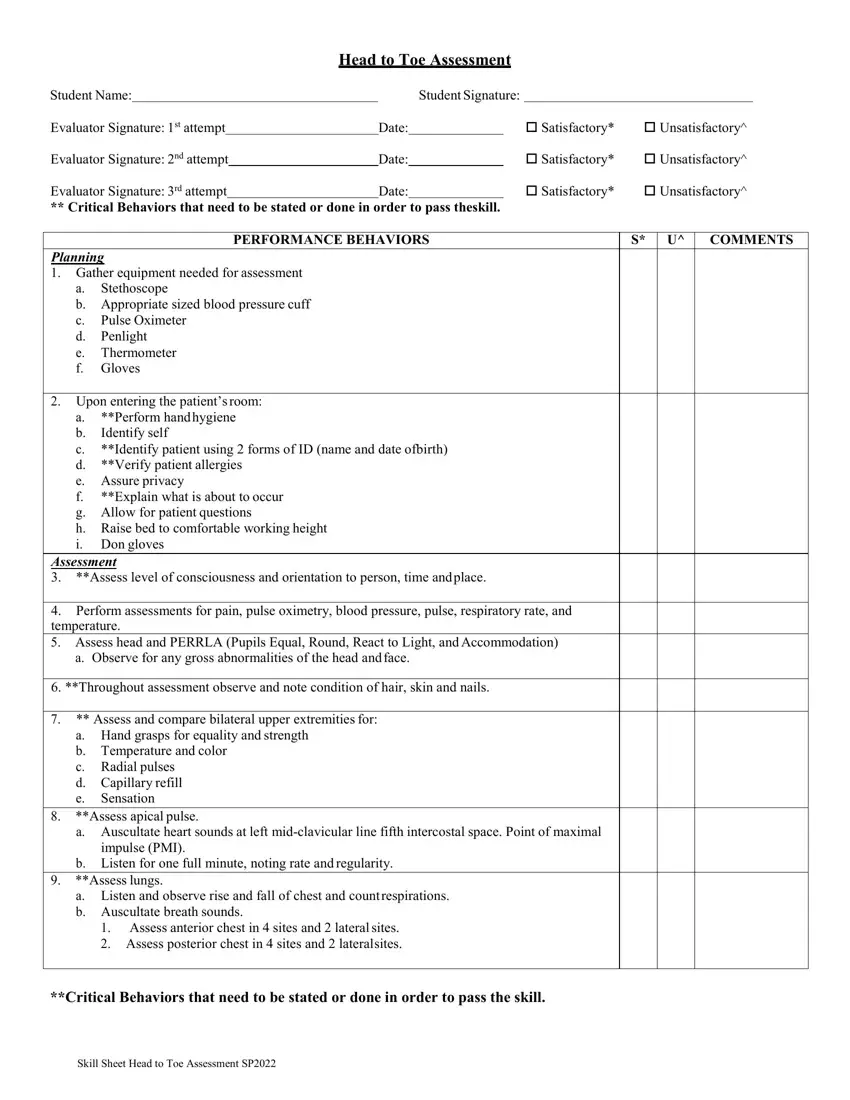
Create the next parts to complete the document:
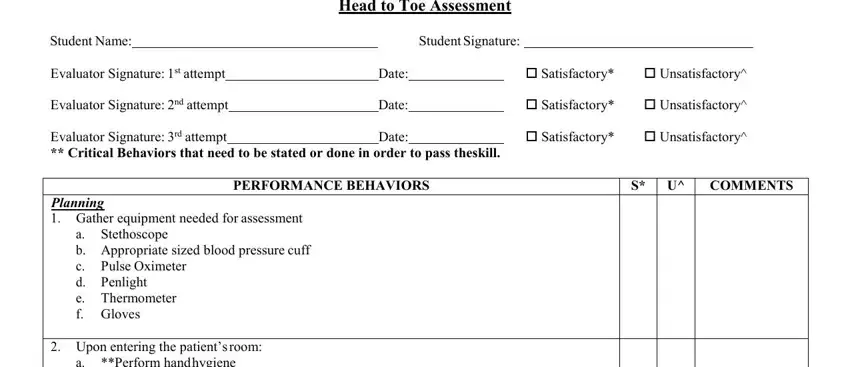
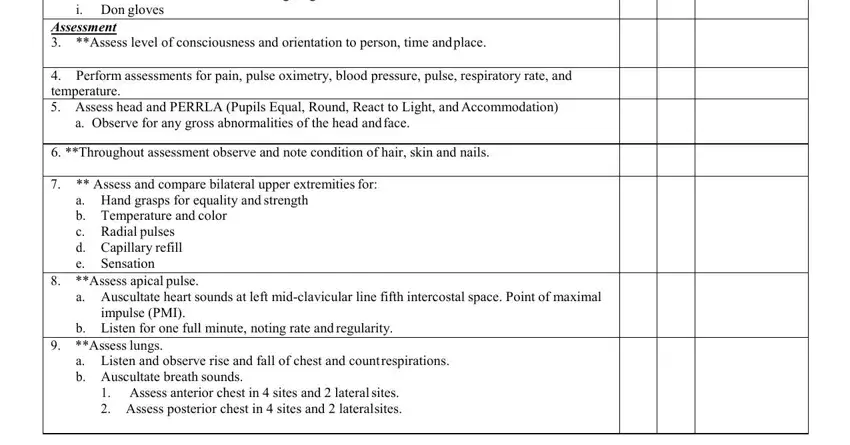
Make sure you type in the necessary data in the Upon entering the patients room a, Assessment Assess level of, Perform assessments for pain, a Observe for any gross, Throughout assessment observe and, Assess and compare bilateral, a Hand grasps for equality and, Assess apical pulse, a Auscultate heart sounds at left, impulse PMI, b Listen for one full minute, Assess lungs, a Listen and observe rise and fall, and Assess anterior chest in sites field.
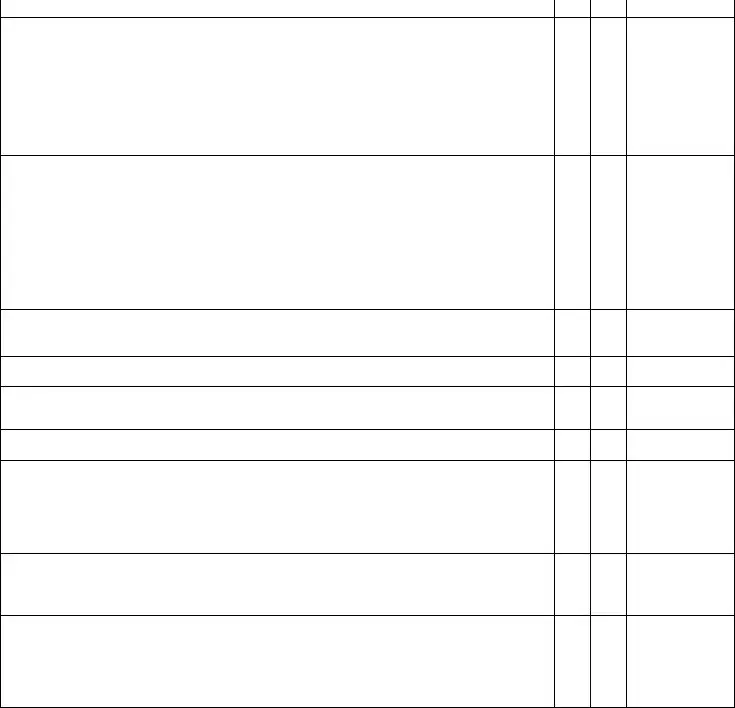
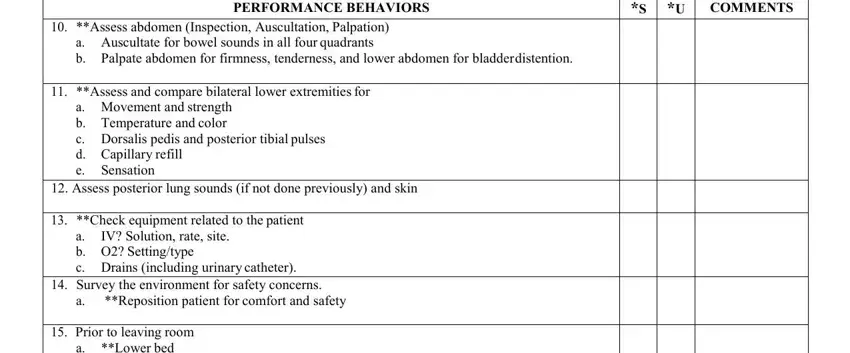
Focus on the most essential details of the PERFORMANCE BEHAVIORS, COMMENTS, Assess abdomen Inspection, Assess and compare bilateral, a Movement and strength b, Assess posterior lung sounds if, Check equipment related to the, IV Solution rate site, a b O Settingtype c Drains, Reposition patient for comfort and, and Prior to leaving room a Lower bed field.
The Prior to leaving room a Lower bed, Evaluation Document assessment, and S Satisfactory U Unsatisfactory field will be the place to put the rights and obligations of either side.
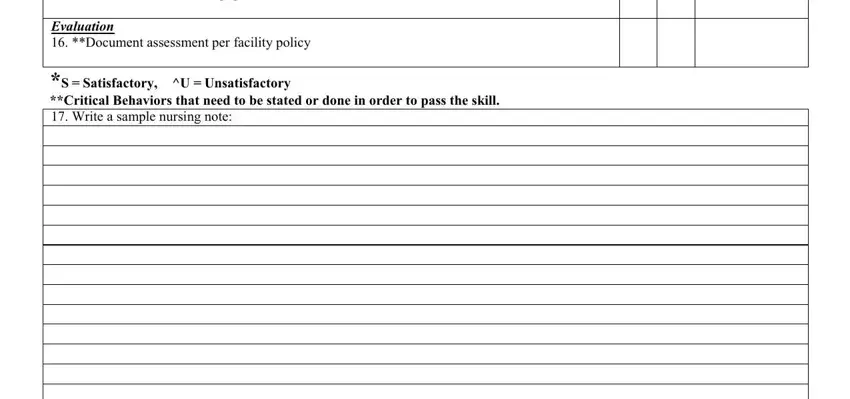
Finish by reading the following fields and completing them accordingly: Skill Sheet Head to Toe Assessment.
Step 3: Press the button "Done". The PDF file is available to be exported. You can download it to your computer or send it by email.
Step 4: Ensure you keep away from future worries by generating minimally two copies of the document.