We have applied the hard work of the best developers to create the PDF editor you are going to apply. The app will assist you to fill out the tb 354 document with no trouble and don’t waste valuable time. Everything you need to do is try out the next quick rules.
Step 1: Click the orange button "Get Form Here" on the following web page.
Step 2: Now you should be within the file edit page. It's possible to add, change, highlight, check, cross, add or erase fields or words.
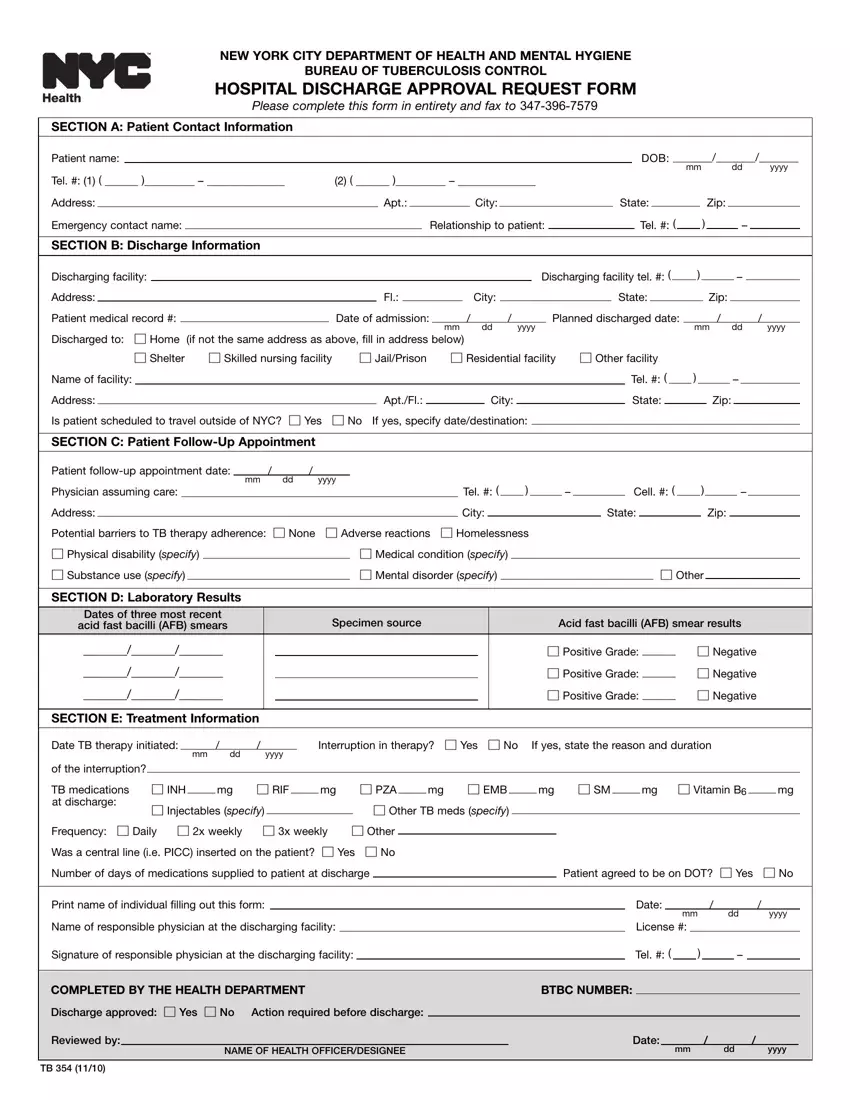
For every single area, fill out the data asked by the software.
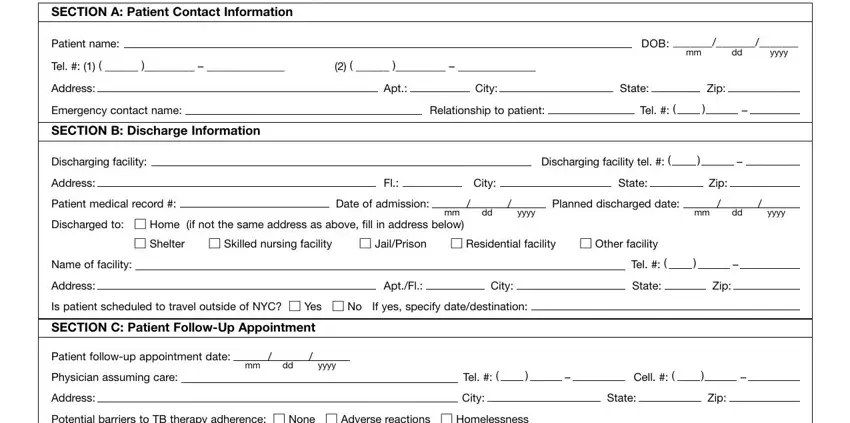
In the Address City State Zip Potential, cid Medical condition specify cid, SECTION D Laboratory Results, Dates of three most recent acid, SECTION E Treatment Information, Specimen source, Acid fast bacilli AFB smear results, cid Positive Grade cid Negative, cid Positive Grade cid Negative, cid Positive Grade cid Negative, Date TB therapy initiated, mm dd yyyy, of the interruption TB medications, cid Injectables specify cid Other, and Frequency cid Daily cid x weekly field, type in your information.
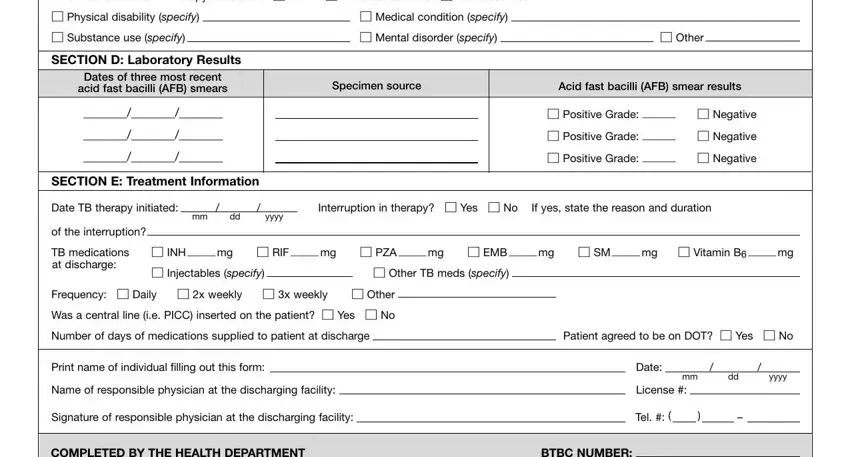
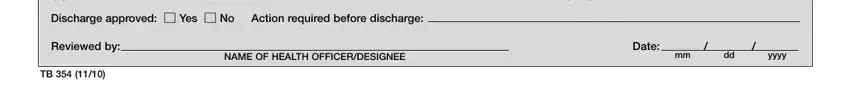
Identify the important data in the COMPLETED BY THE HEALTH DEPARTMENT, BTBC NUMBER, Discharge approved cid Yes cid No, Reviewed by, NAME OF HEALTH OFFICERDESIGNEE, Date, and mm dd yyyy box.
Step 3: Choose the "Done" button. It's now possible to transfer your PDF form to your electronic device. In addition, you can send it by means of electronic mail.
Step 4: To protect yourself from any hassles as time goes on, you should make no less than two or three copies of the document.