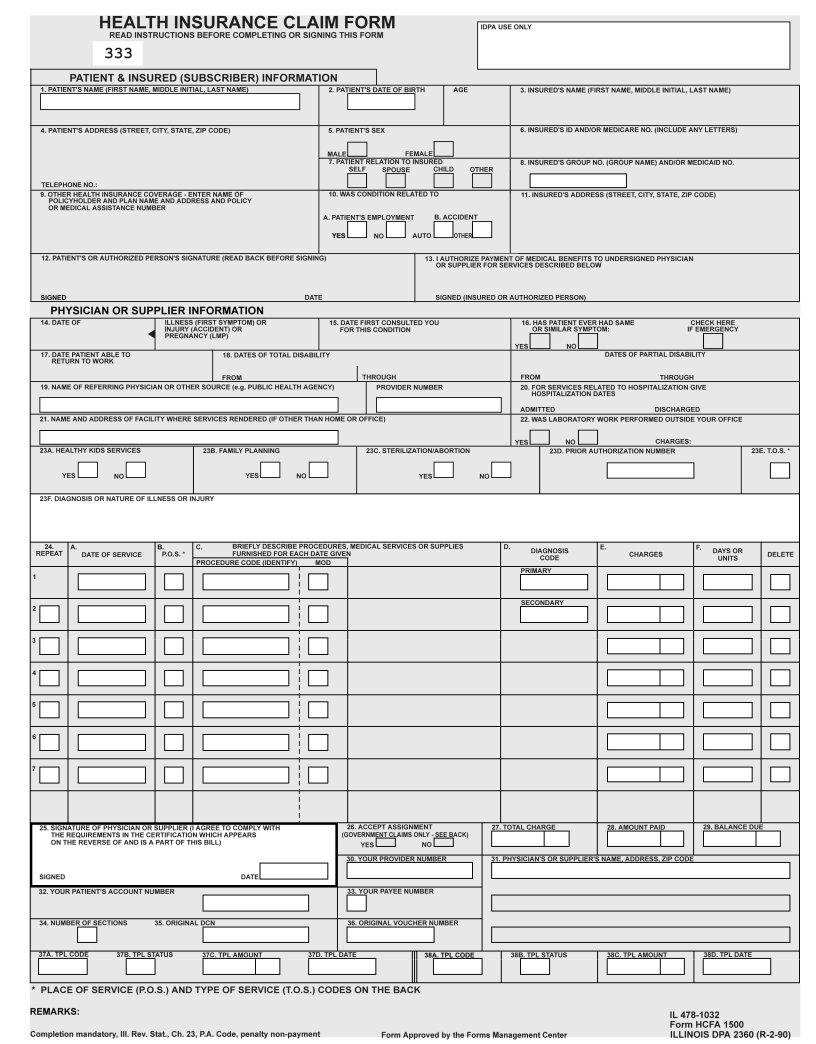
In navigating the complex terrain of health insurance claims, the DPA 2360 health insurance claim form emerges as a vital tool for medical providers, particularly those associated with school-based or linked health centers as outlined in the October 2002 IDPA Appendix S-1. This document serves not only as a billing instrument but also as a means to streamline the processing and reimbursement procedures for various medical services. Key instructions for completing the form range from ensuring legibility and avoiding the use of any form of punctuation to the meticulous process of entering service codes and patient information precisely within designated areas. The guidelines specify the usage of black ink, the avoidance of any handwriting unless absolutely necessary, and the requirement that all attachments must be properly aligned and attached without the use of staples to aid in efficient imaging processing. The stipulated conditions under which each section must be filled, encompassing both mandatory and optional entries, are delineated to facilitate the provider's task in claiming services rendered, whether they pertain to medical care, surgery, diagnostics, or family planning. Furthermore, it delves into specifics such as the formatting of dates, the detailing of service types via codes, and the accurate reporting of charges without deduction for third-party payments. The ultimate goal is to ensure that health centers are reimbursed accurately and promptly for the indispensable services they offer, thereby underscoring the critical nature of adhering to these technical guidelines in claim preparation.
| Question | Answer |
|---|---|
| Form Name | Idpa Form |
| Form Length | 10 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 2 min 30 sec |
| Other names | what is r16 override on idpa form, order form for idpa envelopes, idpa 2360 form, idpa technical form online |
Handbook for School Based/Linked Health Centers |
Chapter |
APPENDIX
TECHNICAL GUIDELINES FOR CLAIM PREPARATION FORM DPA 2360, HEALTH INSURANCE CLAIM FORM
Please follow these guidelines in the preparation of claims for imaging processing to assure the most efficient processing by the Department:
•Claims that are illegible will be returned to the provider.
•Claims with extreme print qualities, either light or dark, will not image.
•Use only one font style on a claim. Do not use bold print, italics, script, or any font that has connecting characters.
•Claims should be typed or
•Do not use punctuation marks, slashes, dashes or any special characters anywhere on the claim form.
•All entries must be within the specified boxes. Do not write in the margins.
•Red ink does not image. Use only black ink for entries on the billing form, attachments and provider signature.
•If corrections need to be made, reprinting the claim is preferred. Correction fluid should be used sparingly.
•Remove the
•Attachments containing a black border as a result of photocopying with the copier cover open cannot be imaged. Attachments must have a minimum one- half inch white border at the top and on the sides to ensure proper imaging of the document.
•For attachments containing gray areas, either as part of the original or as a result of
•Attachments should be
October 2002 |
IDPA Appendix |
Handbook for School Based/Linked Health Centers |
Chapter |
Appendix
The left hand column of the following instructions identifies mandatory and optional items for form completion as follows:
Required |
= |
Entry always required. |
Optional |
= |
Entry optional - In some cases failure to include an entry will |
|
|
result in certain assumptions by the Department and will |
|
|
preclude corrections of certain claim errors by the |
|
|
Department. |
Conditionally |
= |
Entries which are required only under certain circumstances. |
Required |
|
Conditions of the requirement are identified in the instruction |
|
|
text. |
COMPLETION |
ITEM EXPLANATION AND INSTRUCTIONS |
Required |
1. Recipient Name - Enter the participant's name exactly as it |
|
appears on the MediPlan Card or Temporary MediPlan Card |
|
or KidCare Card. Separate the components of the name |
|
(first, middle initial, last) in the proper sections of the name |
|
field. |
Conditionally |
2. Birthdate - Enter the month, day and year of birth of the |
Required |
participant as shown on the MediPlan Card or Temporary |
|
MediPlan Card or KidCare Card. An entry is required when |
|
charges are being billed when Form DPA 1411 does not |
|
contain a recipient number. Use the MMDDYY format. |
October 2002 |
IDPA Appendix |
Handbook for School Based/Linked Health Centers |
Chapter |
Required |
8. |
Recipient No. - Enter the nine digit number assigned to the |
|
|
individual as copied from the MediPlan Card or Temporary |
|
|
MediPlan or KidCare Card. Use no punctuation or spaces. |
|
|
Do not use the Case Identification Number. |
|
|
If the Temporary MediPlan Card does not contain the |
|
|
recipient number, enter the patient name and birthdate on |
|
|
the Provider Invoice and attach a copy of the Temporary |
|
|
MediPlan Card to the Provider Invoice. The Department will |
|
|
review the claim and determine the correct recipient number. |
|
|
See "Mailing Instructions" in this Appendix when a copy of |
|
|
the Temporary MediPlan Card is attached. |
Conditionally |
23a. |
Healthy Kids - If a provider completed a heathly kids |
Required |
|
screening or if diagnostic and treatment services were |
|
|
provided because of a Healthy Kids screening, enter an “X” |
|
|
in the “YES” BOX. |
Conditionally |
23b. Family Planning - If services were rendered for family |
|
Required |
|
planning purposes, enter an “X” in the “YES” box. |
Required |
23e. Type of Service - Enter the code corresponding to the |
|
|
|
type of service for which the charges submitted on the claim |
|
|
apply. |
|
|
Only one type of service can be included on a single claim. |
|
|
A separate claim must be prepared for each type of service |
|
|
for which charges are made. However, labs and |
|
|
not have to be separated out. Use T.O.S. 1 and bill together. |
|
|
The following codes are to be used. |
|
|
1 - Medical Care - Attending Physician |
|
|
2 - Surgery - Surgeon |
Optional |
23f. |
Diagnosis or Nature of Injury or Illness - Enter the |
|
|
diagnosis or nature of injury or illness description which |
|
|
describes the condition primarily responsible for the patient’s |
|
|
treatment. |
Optional |
24. |
Repeat Code - Usage not recommended. |
Required |
24a. Date of Service - Enter the date the service was |
|
|
|
performed. (Use the MMDDYY format). |
October 2002 |
IDPA Appendix |
Handbook for School Based/Linked Health Centers |
Chapter |
Required |
24b. |
Place of Service - Enter the appropriate code which |
|
|
identifies the place where the service was provided. |
|
|
3 or 11 - Office/Clinic |
Required |
24c. Procedure Code/Drug Item Number - When billing for |
|
|
|
services enter the appropriate |
|
|
procedure code. |
|
|
When billing for dispensed items, enter the |
|
|
code or |
|
|
dispensed in the description area (24C) |
Required |
24d. Primary Diagnosis - Enter the specific |
|
|
|
the primary diagnosis. Do not use a decimal or leave a blank |
|
|
space in the decimal point's position. |
|
|
Secondary Diagnosis: An entry in this field is optional. A |
|
|
second |
|
|
secondary diagnosis when appropriate. Do not use a |
|
|
decimal or leave a blank space in the decimal point's |
|
|
position. |
Required |
24e. Provider Charges - Enter the total charge for the service. |
|
|
|
Do not deduct any payment from a third party. |
Conditionally |
24f. |
Days/Units - A |
Required |
|
following: |
|
|
• When billing for multiples of the same lab test, indicate |
|
|
the number; (e.g., for 2 lab tests, enter 0002) |
|
|
• When billing for drug items dispensed, indicate the |
|
|
number; (e.g., for birth control pills, enter 0028). |
Optional |
Delete - When an error has been made that cannot be corrected, |
|
|
enter an “X” to delete the entire service section. Only “X” will be a |
|
|
valid character, all other will be ignored. |
|
Required |
25. |
Signature of Physician and Date Signed - The physician |
|
|
or authorized representative must sign the completed form |
|
|
in black or dark blue ink. Unsigned claims will be rejected. |
|
|
Only original signatures are accepted. Signatures must also |
|
|
be complete (no initials), legible and entered within the |
|
|
boundaries of this item. The signature should not overwrite |
|
|
the date field. Use MMDDYY format. |
October 2002 |
IDPA Appendix |
Handbook for School Based/Linked Health Centers |
Chapter |
Required |
27. |
Total Charge - Enter the sum of all charges shown in service |
|
|
sections 1 through 7 of item 24E. |
Required |
28. |
Amount Paid - Enter the total of all payments received from |
|
|
other sources. If no payment was received, enter 0.00. The |
|
|
entry must equal the sum of the amounts shown in fields 37C |
|
|
and 38C. |
Required |
29. |
Balance Due - Enter the difference between the total charge |
|
|
and amount paid. |
Required |
30. |
Your Provider Number - Enter the 12 digit provider number |
|
|
of the clinic exactly as it is shown on the Provider Information |
|
|
Sheet. |
Required |
31. |
Physician's or Supplier's Name, Address, Zip Code - |
|
|
Enter the clinic's name exactly as it is shown on the Provider |
|
|
Information Sheet. When an address is entered, the |
|
|
Department will attempt to correct claims that have been |
|
|
suspended due to provider name/number errors. When no |
|
|
address is entered, the Department will not attempt to make |
|
|
corrections. |
Conditionally |
32. |
Patient's Account Number - Providers may enter up to 10 |
Required |
|
characters used in your accounting system to identify the |
|
|
patient or transaction. This number will be included on your |
|
|
IDPA Remittance Advice. |
Required |
33. |
Payee Number - Enter the single digit number of the payee |
|
|
to whom payment is to be sent. Payees are listed |
|
|
numerically on the Provider Information Sheet. |
Required |
34. |
Number of Sections - Enter the total number of service |
|
|
sections in Item 24 which have been correctly completed. |
October 2002 |
IDPA Appendix |
Handbook for School Based/Linked Health Centers |
Chapter |
Conditionally |
37A. TPL Code - The TPL Code contained on the |
Required |
patient's MediPlan Eligibility Card (MEC) is to be entered in |
|
this field. If payment was received from a third party |
|
resource not listed on the MEC, enter the appropriate TPL |
|
Code as listed in Chapter 100, General Appendix 9. If none |
|
of the TPL codes that are listed in Chapter 100, General |
|
Appendix 9 are applicable to the source of payment, enter |
|
Code “999" and enter the name of the payment source in |
|
field 9, Other Health Insurance Coverage. If there is more |
|
than one source of other payments to report, the additional |
|
payments are to be shown in Sections |
|
Spenddown - Refer to Chapter 100, Item 133 for a full |
|
explanation of Spenddown policy. If the client has a |
|
Spenddown obligation, they will either be responsible for the |
|
total amount of the charge or will present the provider with a |
|
Form DPA 2432 (SPLIT BILLING TRANSMITTAL FOR |
|
MANG SPENDDOWN PROGRAM). When a Form DPA |
|
2432 is necessary, the Form DPA 2360 should be |
|
completed as follows: |
|
If Form DPA 2432, Split Billing Transmittal, shows a |
|
recipient liability greater than $0.00 the invoice should be |
|
coded as follows: |
|
37A; 906 |
|
37B; 01 |
|
37C; The actual recipient liability as shown on Form |
|
DPA 2432. |
|
37D; The issuance date on the bottom right hand corner |
|
of the DPA 2432. This is in MMDDYY format. |
|
If Form DPA 2432, Split Billing Transmittal, shows a recipient |
|
liability of $0.00 the invoice should be coded as follows: |
|
37A; 906 |
|
37B; 04 |
|
37C; 0 00 |
|
37D; The issuance date on the bottom right hand corner |
|
of the DPA 2432. This is in MMDDYY format. |
October 2002 |
IDPA Appendix |
Handbook for School Based/Linked Health Centers |
Chapter |
37B. TPL Status - A
01 - TPL Adjudicated - total payment shown: TPL Status Code 01 is to be entered when payment has been received from the patient or patient's third party resource. The amount of payment received must be entered in the TPL amount box.
02 - TPL Adjudicated - patient not covered: TPL Status 02 is to be entered when advised by the third party resource that the patient was not insured at the time goods or services were provided.
03 - TPL Adjudicated - service not covered: TPL Status Code 03 is to be entered when advised by the third party resource that goods or services provided are not covered.
04 - TPL Adjudicated - spenddown met: TPL Status Code 04 is to be entered when the patient's Form 2432, (Split Billing transmittal), shows $0.00 liability.
05 - Patient not covered: TPL Status Code 05 is to be entered when a patient informs the provider that the third party resource identified on the Medical Eligibility Card is not in force.
06 - Services not covered: TPL Status Code 06 is to be entered when the provider determines that the identified resource is not applicable to the service provided.
07 - Third Party Adjudication Pending: TPL Status Code 07 may be entered when an invoice has been submitted to the third party and 30 days have elapsed since the third party was billed and reasonable
10 - Deductible not met: TPL Status Code 10 is to be entered when the provider has been informed by the third party resource that
October 2002 |
IDPA Appendix |
Handbook for School Based/Linked Health Centers |
Chapter |
37C. TPL Amount - If there is no TPL amount, enter 0 00. Enter the amount of payment received from the third party resource. A dollar amount entry is required if TPL Status Code 01 was entered in the “Status” box.
37D. TPL Date - A TPL date is required when any status code is shown in Item 37B. Use the following date for the specific TPL status codes;
01 = Third Party Adjudication Date or the date from the DPA 2432
02 = Third Party Adjudication Date
03 = Third Party Adjudication Date
04 = Date from DPA 2432
05 = Date of Service
06 = Date of Service
07 = Date of Service
10 = Third Party Adjudication Date
Conditionally |
38A. |
(See 37A above) |
Required |
38B. |
(See 37B above) |
|
38C. |
(See 37C above) |
|
38D. |
(See 37D above) |
October 2002 |
IDPA Appendix |
Handbook for School Based/Linked Health Centers |
Chapter |
MAILING INSTRUCTIONS
The Provider Invoice is a
The
Routine claims are to be mailed to the Department in
Claims with attachments must be mailed to the Department in the
To order the envelopes mentioned in this topic, refer to Chapter 100, General Appendix 10.
October 2002 |
IDPA Appendix |