Medi-Cal providers who find themselves discontented with the decision on a claim's processing or payment, the opportunity for a reevaluation is extended through the submission of a Medi-Cal Appeal Form— a critical component within the Partnership HealthPlan of California (PHC) Medi-Cal Provider Manual designed to navigate disputes effectively. This structured appeal process mandates that each appeal is furnished with the provider's signature and strictly pertains to claims associated with a singular PHC member, ensuring a focused and organized review. Critical to the appeal's potential success is the inclusion of comprehensive supporting documentation, ranging from corrected claim copies, Remittance Advice reports, relevant identification or Medicare cards, and detailed correspondence that chronicles the timeline and nature of the initial claim and follow-up attempts. It's paramount that these documents are clear and legible to facilitate a thorough examination and review. The claim appeals are bound by a strict 90-day submission window following a CIF denial, with adherence to this timeframe being crucial for consideration. Moreover, the appeal submission process is detailed, indicating the need for precision in completing the form to avoid delays or outright denial. PHC's commitment to responsiveness is highlighted by their structured timetable in acknowledging and resolving appeals, promising acknowledgment within 15 working days and resolution communication within 45 working days of receipt. This structured pathway reflects an adherence to transparency and fairness in the appeals process, providing a lifeline for providers seeking redress for claim grievances.
| Question | Answer |
|---|---|
| Form Name | Medi Cal Appeal Form |
| Form Length | 4 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 1 min |
| Other names | medi cif form, california medical appeal, medi cal cif form pdf, medi cif |
PARTNERSHIP HEALTHPLAN OF CALIFORNIA
CLAIMS DEPARTMENT
VIII.B. Second Level Provider Claims Appeal – PHC
The PHC
An Appeal may be submitted using the
Supporting Documentation:
Necessary documentation should be submitted with each appeal to allow for a thorough review of the appeal. It is very important that all supporting documentation be legible. Include applicable attachments such as:
*Claim copy, corrected if necessary
*Copy of PHC Remittance Advice (RA) Report
*Copy of POE printouts or
*Copy of Medicare EOMB
*Copy of Other Coverage EOBs/RAs or denials
*Copy of all CIFs, Claims Inquiry letters, CIF Response Letters, or other dated correspondence to and from PHC to document timely
*Copy of TAR or RAF
*Copy of manufacturer's invoice or catalog page
*Copy of the PCP prescription
*Copy of report for "By Report" procedures
*Copy of completed Sterilization Consent Form
Appeal submission timelines:
CIF denials for timeliness cannot be appealed.
A provider may submit a "Claim Appeal" within 90 days of the CIF denial. Failure to submit an appeal within the
PHC will acknowledge an Appeal within 15 working days of receipt of the appeal and will respond with an Appeal Response Letter indicating the outcome of the appeal review within 45 working days. If the appealed claim is approved for adjustment, it will appear on a future RA. The claim will continue to be subject to claim processing criteria.
PARTNERSHIP HEALTHPLAN OF CALIFORNIA
CLAIMS DEPARTMENT
Verification of Timely Submission:
The only acceptable documentation to verify timely submission of a claim is a copy of an PHC RA, Claims Inquiry Acknowledgement (CIF), Claims Inquiry Response Letter, or any dated correspondence from PHC containing a CCN with a Julian date falling within the six- month billing limit for the claim submission. A copy of the CIF alone without the accompanying Claims Inquiry Acknowledgement/Response Letter does not prove timely
Submit all Appeals to:
Partnership HealthPlan of California
Attn: Claims Department/Appeals
P.O. Box 1368
Suisun City, CA
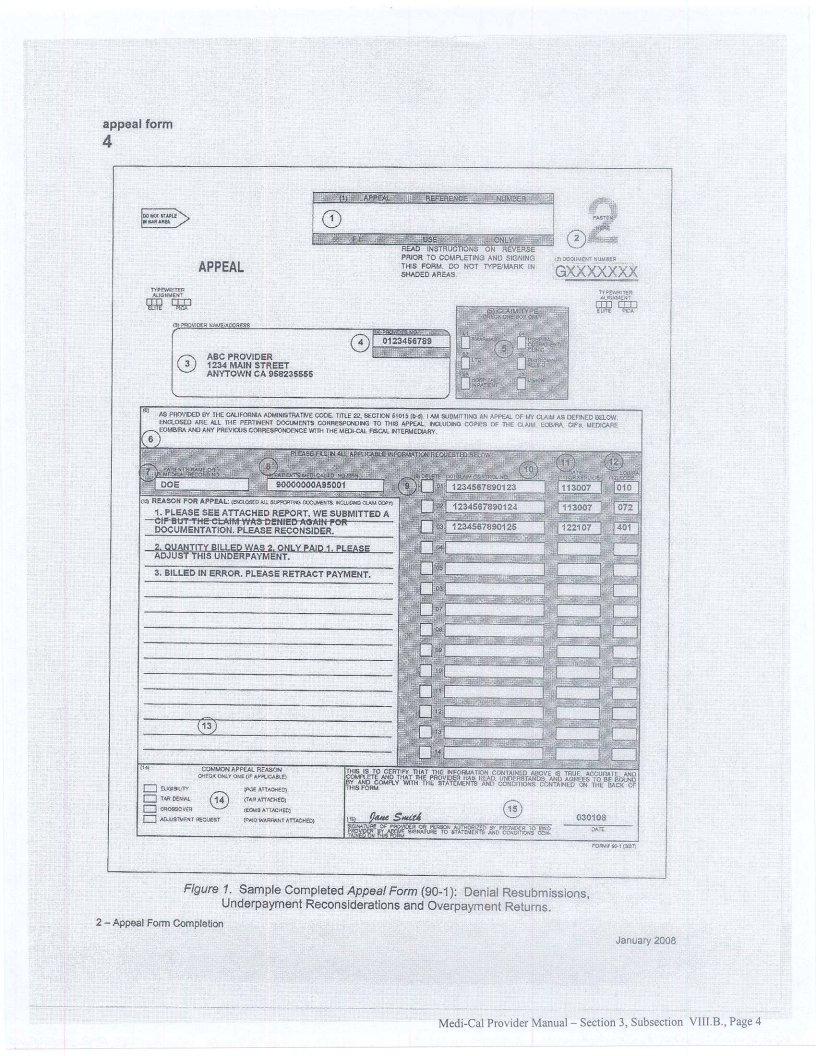
Instructions on completing the Appeal Form:
Each numbered item below refers to an area on the
Item Description
1.Appeal Reference Number. For PHC use only.
2.Document Number. The
3.Provider Name/Address. Enter the following information: Provider Name, Street Address, City, State, and ZIP code.
4.Provider Number (Required Field). Enter your provider number/National Provider Identifier (NPI). Without the correct provider number, appeal acknowledgement may be delayed.
5.Claim Type. Enter an "X" in the box indicating the claim type. Only one box may be checked.
6.Statement of Appeal. For information purposes only.
7.Patient's Name. Enter up to the first 10 letters of the patient's last name.
8.Patient's
9.Delete. Enter an "X" to delete the corresponding line.
PARTNERSHIP HEALTHPLAN OF CALIFORNIA
CLAIMS DEPARTMENT
10.Claim Control Number (Required Field if Appealing a Previously Adjudicated Claim). Enter the
11.Date of Service. In
12.EOB/RA Code. When appealing a claim, enter the PHC Adj Rsn/Remark for the claim line (e.g., 45, N14, 96, 4).
13.Reason for Appeal. Indicate your reason for filing an appeal. Be as specific as possible. In order for the examiners to properly research the complaint, all supporting documentation must be included.
14.Common Appeal Reasons. Check one of these boxes if applicable. Include a copy of the claim and supporting documentation (e.g., POE, TAR, EOMB). This box is for your convenience only. Leave Box 13 blank if this box is used.
15.Signature. This provider or an authorized representative must sign the Appeal Form. A sample of the
For further information on how to complete a