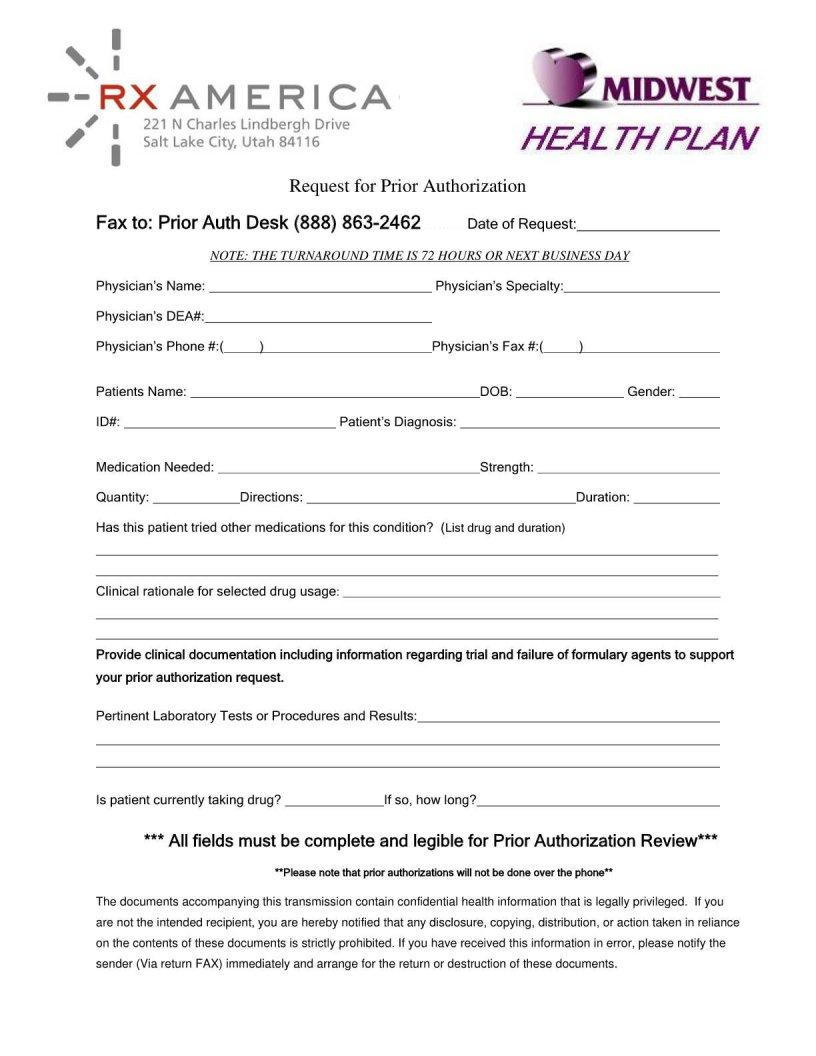
In the landscape of healthcare, the process of securing approval for certain medical services or prescriptions before receiving them is a critical step for patients and healthcare providers alike. This is where the Midwest Prior Authorization form comes into play, serving as a fundamental tool to streamline this procedure. It essentially serves as a bridge between healthcare providers and insurance companies, ensuring that the proposed services or medications are covered under the patient's insurance plan before any financial commitment is made. The form requires detailed information about the patient, the medical provider, and the specific service or medication for which authorization is being requested, providing a clear pathway for reviewing and approving the necessity and coverage of the said service. This method not only helps in managing healthcare costs but also aids in preventing unnecessary procedures, thereby fostering a more efficient and cost-effective healthcare system. Understanding the intricacies of this form, from its structure to its pivotal role in the prior authorization process, is essential for all parties involved in the delivery and receiving of healthcare services.
| Question | Answer |
|---|---|
| Form Name | Midwest Prior Authorization Form |
| Form Length | 1 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 15 sec |
| Other names | authorization, hap midwest prior authorization form, Auth, authorizations |