This step-by-step process guarantees a thorough approach to reporting incidents, crucial for improving healthcare safety.
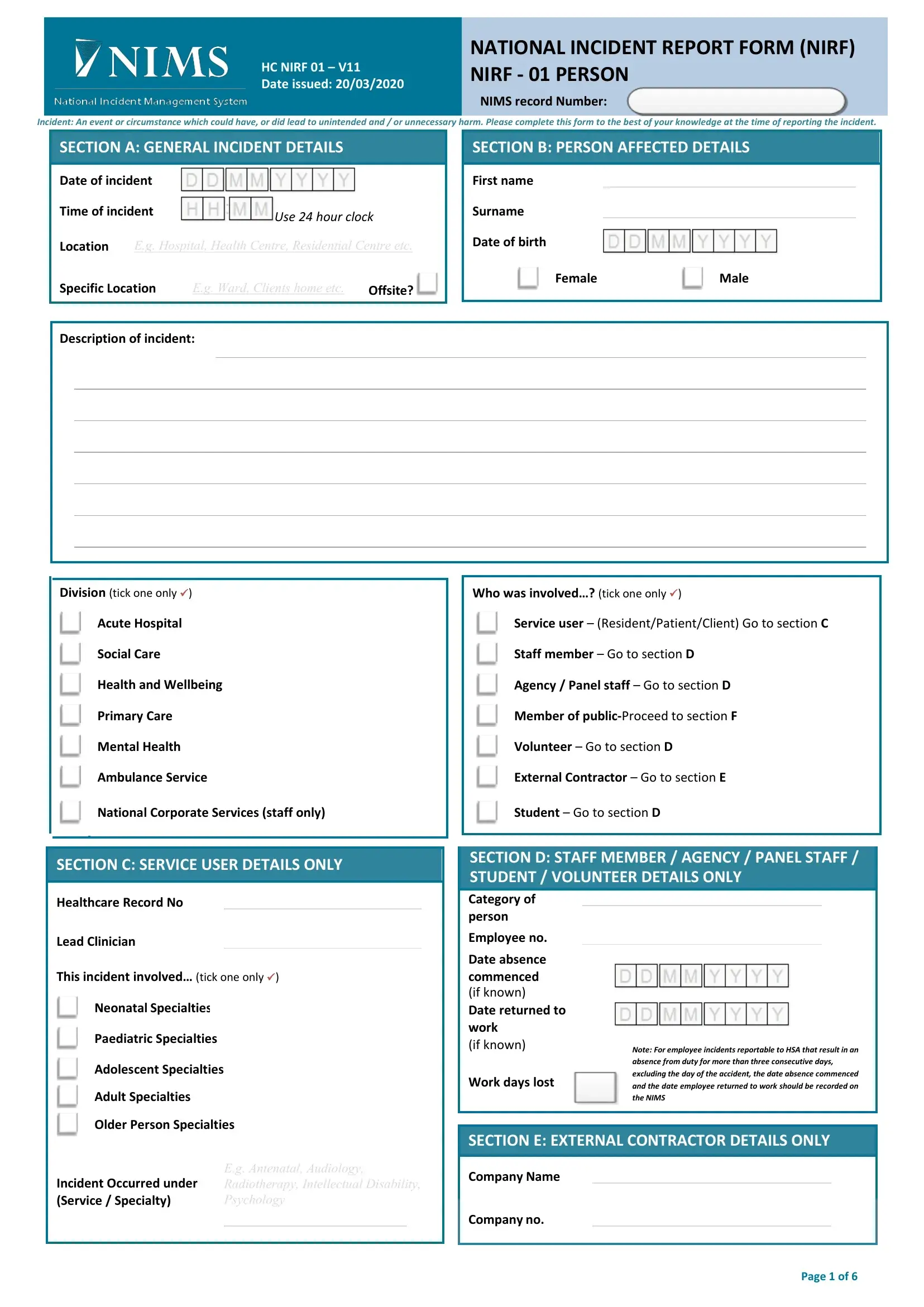
1. Fill in General Incident Details
Begin by providing the date and time of the incident using a 24-hour clock format. Specify the general location, such as the hospital or health center, and the specific location, like the ward or patient's home, where the incident occurred.
2. Person Affected Details
Identify the person affected by the incident. Enter their first name, surname, and date of birth. Specify the gender and division they belong to — such as Acute Hospital, Social Care, etc. Indicate the category of the person involved, whether a service user, staff member, volunteer, or external contractor, directing to the appropriate subsequent section based on their role.
3. Describe the Incident
Provide a detailed description of the incident. This should include what happened, the sequence of events, and any immediate factors contributing to the incident.
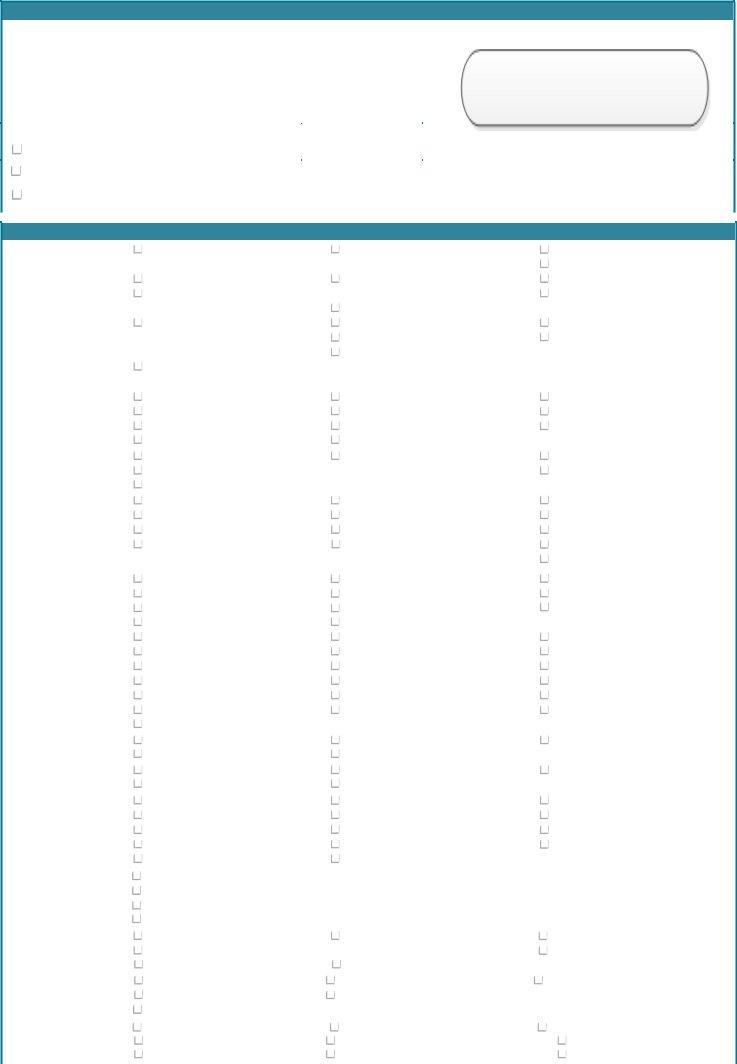
4. The Outcome at the Time of the Incident
Record the immediate outcomes of the incident. This includes whether it was a near miss, resulted in no injury, required first aid, or led to more severe consequences such as long-term disability or death. Specify the body part affected if there was an injury.
5. Specify the Type of Injury
If applicable, detail the type of injury sustained. Options include specific injuries related to birth, blood-specific injuries, diagnosed diseases, and general injuries.
6. Identify the Type of Hazard
Indicate what type of hazard led to the incident, whether clinical care, medication issues, equipment failure, or environmental conditions.
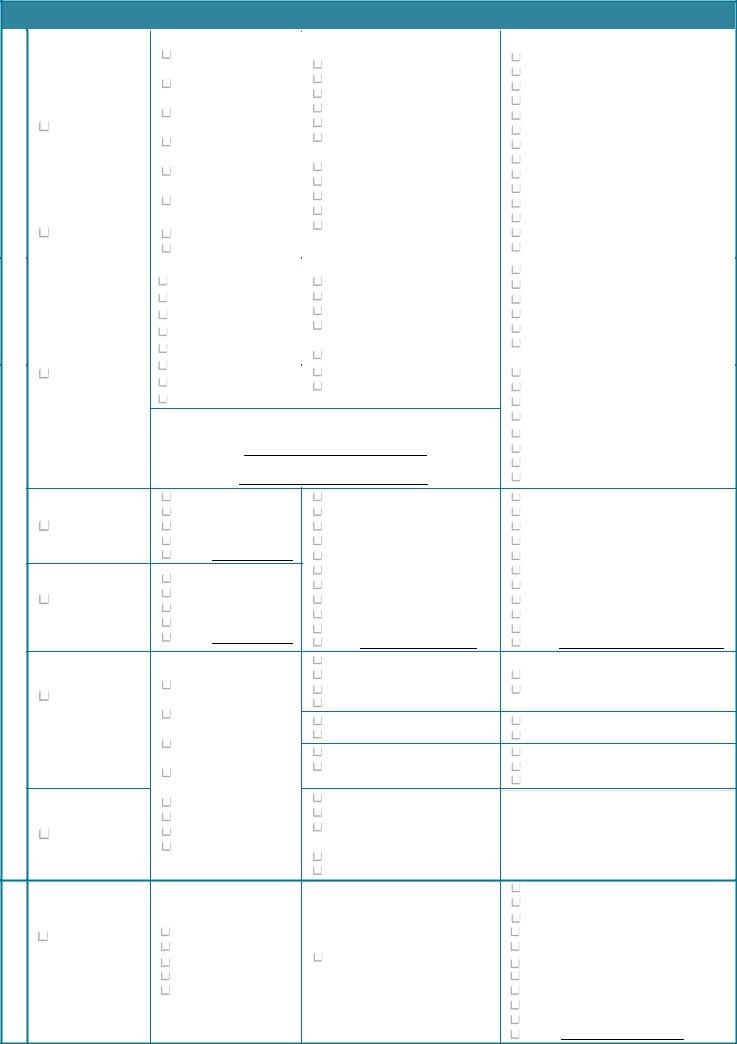
7. Report Immediate Actions Taken
Note any immediate actions that were taken in response to the incident. This could include medical treatment provided, safety measures implemented, or other emergency responses.
8. Reporter and Witness Details
The person who identifies the incident should fill out their details and those of any witnesses. This includes names, contact information, and the role of the person reporting the incident.
9. Management Review
The line or department manager reviews the completed form, verifies open disclosure, and indicates whether the incident needs to be reported to external regulators or agencies.
10. Quality and Patient Safety Office Review
Finally, the Quality and Patient Safety Office must determine if the incident qualifies as a Serious Reportable Event (SRE) and complete its form section.