Navigating the complex landscape of health and nutrition, the Nutrition Assessment Form serves as a critical tool, meticulously devised by Leigh Wagner, MS, RD, an Integrative Nutritionist. At the heart of improving one’s health and well-being, encompassing aspects such as lifestyle, family history, emotional health, and eating habits, this form offers a comprehensive view designed to capture the overall health habits and lifestyle of individuals. Newly designed for patients, it requests detailed personal information, including their preferred method of contact, living situation, and health goals, alongside a readiness assessment for adopting healthier habits. Furthermore, it dives into past medical history, family health background, and a meticulous symptoms questionnaire covering the last 30 days to gather a snapshot of the individual’s health which could reveal patterns and areas needing attention. This thorough approach not only facilitates an in-depth understanding for the nutritionist but also engages the individual in their health journey, making it a foundational step towards personalized nutrition and wellness planning.
| Question | Answer |
|---|---|
| Form Name | Nutrition Assessment Form |
| Form Length | 11 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 2 min 45 sec |
| Other names | nutritional assessment questionnaire forms, outpatient nutrition assessment form pdf, nutrition assesment sheet, nutrition assessment fome |
Leigh Wagner, MS, RD
Integrative Nutritionist
Email: lwagner@kumc.edu
One’s health and
New Patient Nutrition Assessment Form
First Name _______________________Middle Name_________________Last Name____________________
Address _______________________________ City ________________________State_____Zip:____________
Please indicate your preferred method of contact: |
home |
work |
cell |
||
Home |
|
Birth Date _____/_____/_____ Age __________ |
|||
Work Phone |
|
Email address: ___________________________ |
|||
Cell Phone |
Height: ___ ____ |
Weight: _______ Sex: _____ |
|||
|
|
Blood Type (Please circle): A / AB / B / O / Unk |
|||
Occupation _____________________________ |
Marital Status ____________________________ |
||||
Do you have children? Yes |
No |
Age of children____________________________ |
|||
Are you pregnant? Yes No |
Due Date_________ |
|
|
|
|
With whom do you live? (Include children, parents, relatives, and/or friends. Please include ages.) Example: Sarah, age 7, sister
____________________________________________________________________________________________
____________________________________________________________________________________________
Primary Care Provider __________________________ Date of last physical exam ______________________
Other doctors or practitioners you see __________________________________________________________
Would you like to receive
If yes, please sign ___________________________________________________________________________
1
Revised August 2011
Leigh Wagner, MS, RD
Integrative Nutritionist
Email: lwagner@kumc.edu
GOALS AND READINESS ASSESSMENT
I would like to visit with the dietitian, today because…
___________________________________________________________________________________________
___________________________________________________________________________________________
___________________________________________________________________________________________
My food and
___________________________________________________________________________________________
___________________________________________________________________________________________
___________________________________________________________________________________________
My overall, health goals are…
___________________________________________________________________________________________
___________________________________________________________________________________________
___________________________________________________________________________________________
If I could change three things about my health and nutritional habits, they would be…
1._____________________________________________________________________________________
_____________________________________________________________________________________
2._____________________________________________________________________________________
_____________________________________________________________________________________
3._____________________________________________________________________________________
_____________________________________________________________________________________
The biggest challenge(s) to reaching my nutrition goals is/are:
___________________________________________________________________________________________
___________________________________________________________________________________________
___________________________________________________________________________________________
In the past, I have tried the following techniques, diets, behaviors, etc. to reach my nutrition goals…
___________________________________________________________________________________________
___________________________________________________________________________________________
___________________________________________________________________________________________
On a scale of 1 (not willing) to 5 (very willing), please indicate your readiness/willingness to do the following:
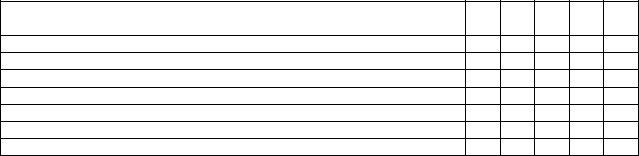
To improve your health, how ready/willing are you to… |
1 |
2 |
3 |
4 |
5 |
|
Significantly modify your diet
Take nutritional supplements each day
Keep a record of everything you eat each day
Modify your lifestyle (ex: work demands, sleep habits, physical activity)
Practice relaxation techniques
Engage in regular exercise/physical activity
Have periodic lab tests to assess your progress
2
Revised August 2011
Leigh Wagner, MS, RD
Integrative Nutritionist
Email: lwagner@kumc.edu
PAST MEDICAL AND SURGICAL HISTORY
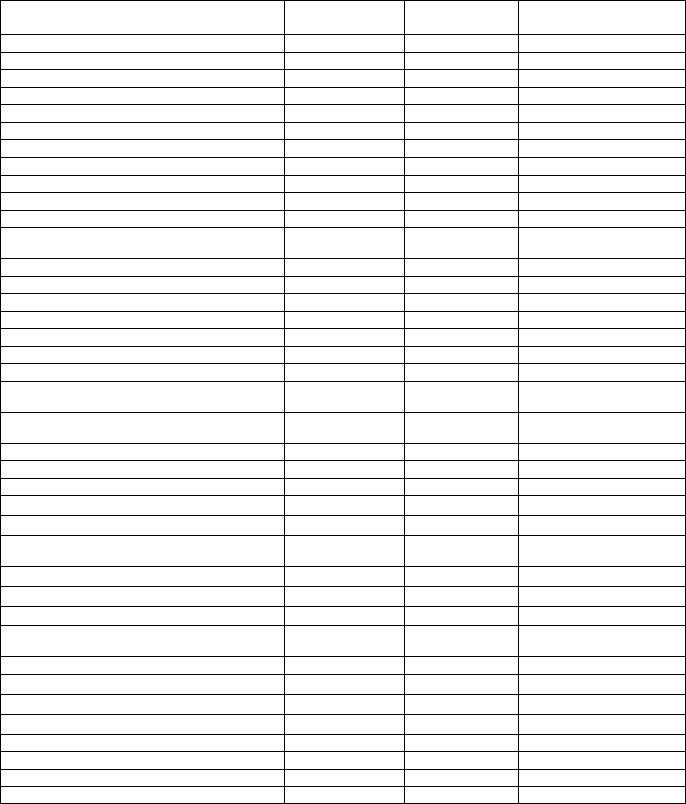
Please indicate whether you or your relatives* have been diagnosed with any of the following diseases or symptoms (specify which relative and the date of diagnosis). *Relatives include: parents, grandparents, siblings.
Illness/Disease/Symptom |
Self: |
Relative: |
Describe/Specify |
|
Age Diagnosed |
Age Diagnosed |
|
Allergies (please specify type of allergy)
Anemia
Anxiety or Panic Attacks
Arthritis (osteoarthritis or rheumatoid)
Asthma
Autoimmune condition (specify type)
Bronchitis
Cancer
Chronic Fatigue Syndrome
Crohn’s ′isease or Ulcerative Colitis
Depression
Diabetes (Specify: Type I, II, Prediabetes, Gestational Diabetes)
Dry, itchy skin, rashes, dermatitis
Eczema
Emphysema
Epilepsy, convulsions, or seizures
Eye Disease (please specify)
Fibromyalgia
Food Allergies or Sensitivities
Fungal Infection (athlete’s food, ringworm, other)
Gallbladder Disease/Gallstones (specify)
Gout
Heart attack/Angina
Heartburn
Heart disease (specify)
Hepatitis
High blood fats (cholesterol, triglycerides)
High blood pressure (hypertension)
Hypoglycemia (low blood sugar)
Intestinal Disease (specify)
Infammatory Bowel ′isease (Crohn’s or
Ulcerative Colitis)
Irritable bowel syndrome
Kidney disease/failure or Kidney stones
Lung disease (specify)
Liver disease
Mononucleosis
Osteoporosis
PMS
Polycystic Ovarian Syndrome
3
Revised August 2011

|
|
|
|
|
Leigh Wagner, MS, RD |
|
|
|
|
|
Integrative Nutritionist |
|
|
|
|
|
Email: lwagner@kumc.edu |
|
Illness/Disease/Symptom |
Self: |
Relative: |
|
Describe/Specify |
|
|
Age Diagnosed |
Age Diagnosed |
|
|
|
|
|
|
|
|
|
Pneumonia |
|
|
|
|
|
Prostate Problems |
|
|
|
|
|
Psychiatric Conditions |
|
|
|
|
|
Seizures or epilepsy |
|
|
|
|
|
Sinusitis |
|
|
|
|
|
Sleep apnea |
|
|
|
|
|
Stroke |
|
|
|
|
|
Thyroid disease (hypo- or hyperthyroid) |
|
|
|
|
|
Urinary Tract Infection |
|
|
|
|
|
Other (describe) |
|
|
|
|
|
Injuries |
Age |
|
Describe/Specify |
|
|
|
|
|
|
|
|
Back injury |
|
|
|
|
|
Broken (specify) |
|
|
|
|
|
Head injury |
|
|
|
|
|
Neck injury |
|
|
|
|
|
Other (describe) |
|
|
|
|
|
Diagnostic Studies |
Age at study |
|
Describe/Specify |
|
|
|
|
|
|
|
|
Barium Enema |
|
|
|
|
|
Bone Scan |
|
|
|
|
|
CAT Scan: Abdom., Brain, Spine (specify) |
|
|
|
|
|
Chest |
|
|
|
|
|
Colonoscopy or Sigmoidoscopy (specify) |
|
|
|
|
|
EKG |
|
|
|
|
|
Liver scan |
|
|
|
|
|
NMR/MRI |
|
|
|
|
|
Upper GI Series |
|
|
|
|
|
Other (describe) |
|
|
|
|
|
Operations |
Age at operation |
|
Describe/Specify |
|
|
|
|
|
|
|
|
Dental Surgery |
|
|
|
|
|
Gall Bladder |
|
|
|
|
|
Hernia |
|
|
|
|
|
Hysterectomy |
|
|
|
|
|
Tonsillectomy |
|
|
|
|
|
Other (describe) |
|
|
|
|
Please complete the following information concerning your family’s health history:
|
|
If Living |
If Deceased |
|
|
If Living |
If Deceased |
||
|
Age |
Health |
Age at |
Cause |
|
Age |
Health |
Age at |
Cause |
|
death |
|
death |
||||||
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
Father |
|
|
|
|
Spouse/Partner |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Mother |
|
|
|
|
Children |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Siblings |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4
Revised August 2011
Leigh Wagner, MS, RD
Integrative Nutritionist
Email: lwagner@kumc.edu
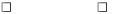
MEDICAL SYMPTOMS QUESTIONNAIRE
Rate each of the following symptoms based upon your typical health profile for the past 30 days. If you have been having recent or somewhat severe health symptoms, please indicate that you will fill out the questionnaire for the past 48 hours.
Past 30 days |
Past 48 hours |
Point Scale
0– Never or almost never have the symptom
1 – Occasionally have it, effect is not severe
2 – Occasionally have it, effect is severe
3 – Frequently have it, effect is not severe
4 – Frequently have it, effect is severe
HEAD
_______Headaches
_______Faintness
_______Dizziness
_______Insomnia
|
|
Total ______ |
EYES |
|
|
|
_______ Watery or itchy eyes |
|
|
_______ Swollen, reddened or sticky eyelids |
|
|
_______ Bags or dark circles under eye |
|
|
_______ Blurred or tunnel vision |
|
|
(does not include near or |
|
|
|
Total _______ |
EARS |
_______ Itchy ears |
|
|
_______ Earaches, ear infections |
|
|
_______ Drainage from ear |
|
|
_______ Ringing in ears, hearing loss |
Total _______ |
NOSE |
_______ Stuffy nose |
|
|
_______ Sinus problems |
|
|
_______ Hay fever |
|
|
_______ Sneezing attacks |
|
|
_______ Excessive mucus formation |
Total _______ |
MOUTH/THROAT |
|
|
|
_______ Chronic cough |
|
|
_______ Gagging, frequent need to clear throat |
|
|
_______ Sore throat, hoarseness, loss of voice |
|
|
_______ Swollen or discolored tongue, gums, lips |
|
|
_______ Canker sores |
Total _______ |
SKIN |
_______ Acne |
|
|
_______ Hives, rashes, dry skin |
|
|
_______ Hair loss |
|
|
_______ Flushing, hot flashes |
|
|
_______ Excessive sweating |
Total _______ |
HEART |
_______ Irregular or skipped heartbeat |
|
|
_______ Rapid or pounding heartbeat |
|
|
_______ Chest pain |
Total _______ |
5
Revised August 2011