The Past Medical History Form serves as a comprehensive tool designed to gather detailed information about a patient's medical background, crucial for physical therapy and treatment planning. Utilized by Momentum Physical Therapy, this form captures essential data starting with the basics, like the patient's name, work status, and the date of injury or onset of symptoms. It delves deeper by examining whether the symptoms are a result of work-related injuries, accidents, or other causes. Importantly, the form inquires about previous occurrences of similar symptoms, surgeries related to the condition, and if the symptoms are associated with specific incidents such as falls or athletic activities. A significant portion is dedicated to identifying any existing or past conditions that may impact the therapy, ranging from chronic diseases like diabetes and heart disease to possible allergic reactions and physical ailments such as hernias or recent fractures. The form is also sensitive to lifestyle factors and other health indicators, asking about pregnancy, past surgeries, cancer, and even habits like smoking. Additionally, it prompts the patient to disclose any medications they're currently taking, ensuring that the therapy plan accommodates all aspects of the patient's health. To ensure all-rounded care, it asks for emergency contact information and encourages patients to disclose any other relevant medical history that might not be covered by the form's questions. Furthermore, it employs a unique key to pinpoint the location and nature of symptoms, enhancing the therapist’s understanding of the patient’s condition. This elaborate form ends with spaces for the patient, their guardian (if applicable), and the therapist's signatures, underscoring the collaborative approach between the patient and healthcare providers in managing and understanding the patient’s health.
| Question | Answer |
|---|---|
| Form Name | Past Medical History Form |
| Form Length | 2 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 30 sec |
| Other names | physical past medical form, physician history forms, therapy past medical sample, physical therapy past medical form |
Momentum Physical Therapy
PAST MEDICAL HISTORY FORM
Patient Name:
Are you presently working?
Date of injury / onset: |
/ |
Yes
/
Date:
No |
Date of next physician’s visit: |
Have you ever had these symptoms before?
/ /
Yes No
Check which apply to your symptoms: |
|
|
Work related injury |
Recurrence of previous injury |
|
Motor vehicle accident |
Injury related to lifting |
|
Cause unknown |
Athletic / recreational injury |
|
Have you had a related surgery? |
Yes |
No |
Injury related to falling Other: _________________
Do you have, or have you had any of the following? |
|
|
|
Yes |
No |
Yes |
No |
Diabetes |
|
Allergies to Aspirin |
|
Chest Pain / Angina |
|
Allergies to Heat |
|
High Blood Pressure |
|
Allergies / Poor tolerance to Cold |
|
Heart Disease |
|
Other Allergies |
|
Heart Attack |
|
Hernia |
|
Heart Palpitations |
|
Seizures |
|
Pacemaker |
|
Metal Implants |
|
Headaches |
|
Dizziness / Fainting |
|
Kidney Problems |
|
Recent Fractures |
|
Are you pregnant? |
|
Surgeries |
|
Cancer |
|
Skin Abnormalities |
|
Osteoporosis |
|
Sexual Dysfunction |
|
Bowel / Bladder Abnormalities |
|
Nausea / Vomiting |
|
Urine Leakage |
|
Ringing in your ears |
|
Asthma / Breathing Difficulties |
|
Rheumatoid Arthritis |
|
Liver / Gallbladder Problems |
|
Special Diet Guidelines |
|
Smoking |
|
Hypoglycemia |
|
Stroke/CVA |
|
Other:_______________________ |
|
If yes on any of the above, please briefly explain and give approximated date:
Is there any other information regarding your past medical history that we should know about?
Are you presently taking Medication? |
Yes |
No |
If yes, please list what medications and for what condition:
1 of 2
In the rare instance of an emergency, whom should we contact?
Name:
Phone Number:
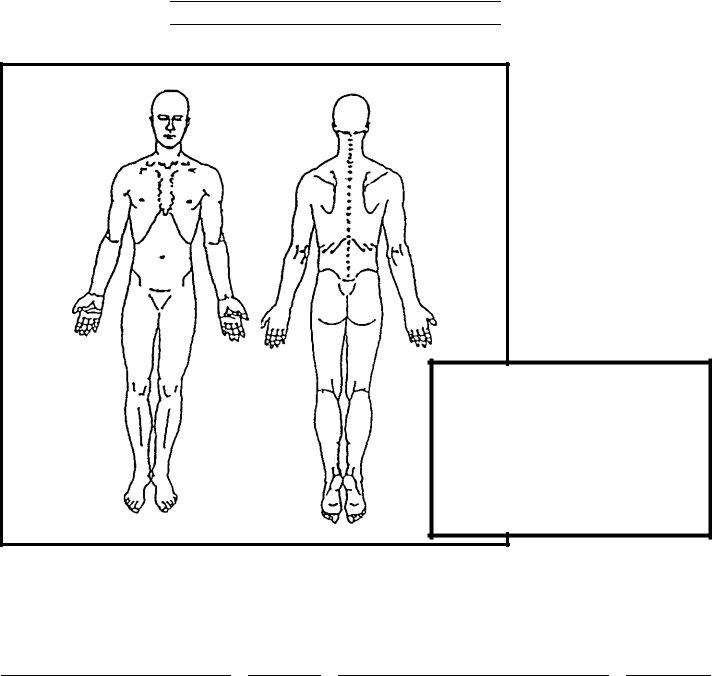
Please indicate below where your symptoms are located.
KEY: |
|
Numbness |
======== |
Pins & Needles |
ooooooo |
Burning Pain |
xxxxxxxx |
Stabbing Pain |
/ / / / / / / / |
|
|
If you are having pain, please rate the intensity of your pain on a scale of 0 to 10, with 0 being no pain and 10 being the worst pain possible: ___________________.
Patient’s Signature |
Date |
Signature of Guardian if patient is a minor |
Date |
||
|
/ |
/ |
|
|
|
Therapist Signature |
|
Date |
|
|
|
2 of 2