Any time you intend to fill out aide curriculum virginia, you won't need to install any sort of programs - simply give a try to our PDF tool. FormsPal team is dedicated to providing you the perfect experience with our editor by continuously presenting new functions and enhancements. Our editor is now a lot more helpful thanks to the latest updates! So now, editing PDF documents is a lot easier and faster than ever before. Here is what you'll need to do to begin:
Step 1: Firstly, open the pdf editor by pressing the "Get Form Button" in the top section of this page.
Step 2: After you access the file editor, you'll notice the form prepared to be filled out. Besides filling out different blank fields, you might also perform many other things with the Document, such as adding custom words, changing the original textual content, inserting graphics, placing your signature to the form, and much more.
It will be easy to complete the document using this detailed guide! Here's what you want to do:
1. You should fill out the aide curriculum virginia correctly, hence pay close attention when filling in the sections comprising these fields:
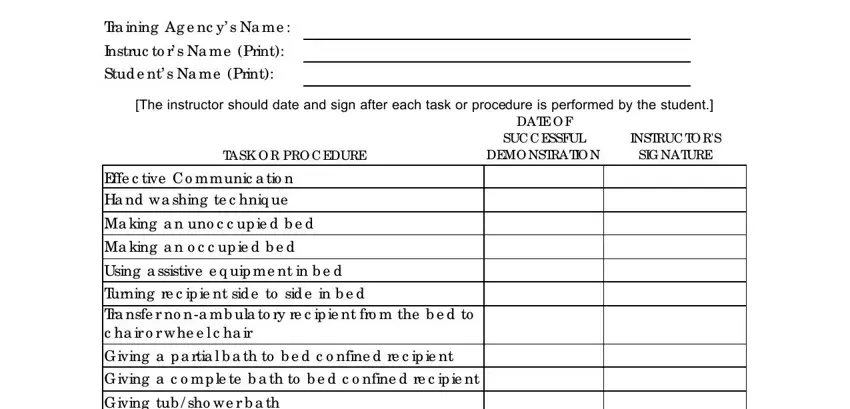
2. Soon after filling in the last step, head on to the subsequent step and enter the essential details in all these blank fields - Pe rine a l c a re ma le fe ma le, Skin c a re, G iving a p a rtia l b a th to b e, Dre ssing o r a ssisting with d re, Ha ir c a re inc lud ing sha ving, Pro vid ing p a ssive ra ng e o f, O ra l hyg ie ne with witho ut d e, Pre p a ring a nd se rving the re, Fe e d ing re c ip ie nt who is, We a r g lo ve s whe n a p p ro p, and Re c ip ie nt s la und ry.
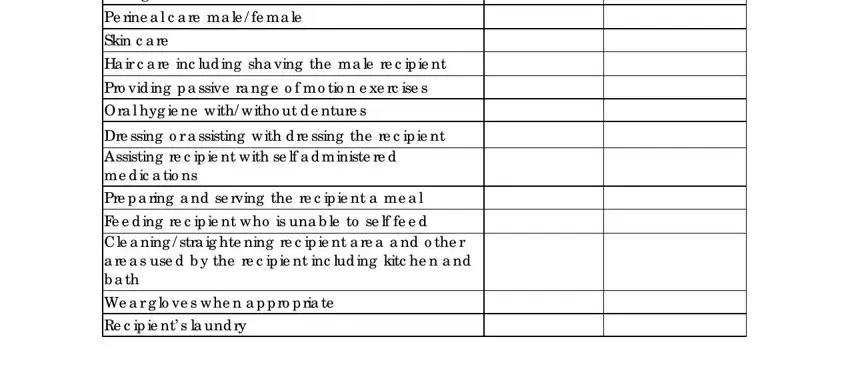
In terms of Pro vid ing p a ssive ra ng e o f and Ha ir c a re inc lud ing sha ving, be certain that you double-check them here. Both of these are surely the key fields in this file.
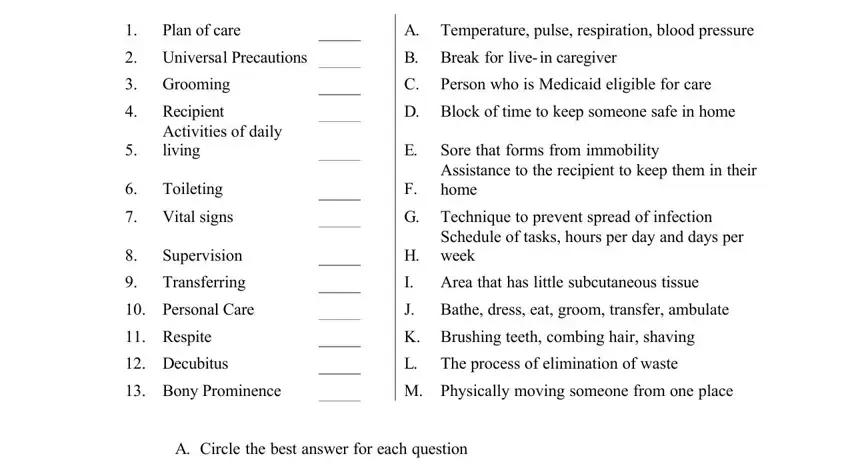
3. Completing Match the following vocabulary, Plan of care, Universal Precautions, Grooming, Recipient, Activities of daily living, Toileting, Vital signs, Supervision, Transferring, Personal Care, Respite, Decubitus, Bony Prominence, and A Temperature pulse respiration is essential for the next step, make sure to fill them out in their entirety. Don't miss any details!
4. This section comes next with the next few blanks to consider: List five different bony, What are some of the symptoms of, a Itching b Blisters c Redness d, When transferring a recipient the, and a Make sure they are barefoot b.
5. This very last step to submit this form is crucial. Make certain to fill in the appropriate blank fields, including List physical aspects of aging, B True or False, T F DMAS does not require a, Record DMAS, and Page of Pa g e o f, before using the pdf. Failing to accomplish that can generate an unfinished and potentially unacceptable form!
Step 3: Once you've reviewed the details you given, just click "Done" to complete your form at FormsPal. Join FormsPal today and immediately access aide curriculum virginia, prepared for download. Each modification made is conveniently saved , helping you to edit the form later as needed. FormsPal is focused on the privacy of our users; we make sure that all information coming through our editor is kept protected.