In Washington State, a distinctive approach is taken towards evaluating public mental health services through the use of the Washington State Program of Assertive Community Treatment (WA-PACT) Comprehensive Assessment Template. This essential tool is designed with a focus on ensuring thorough and individualized assessments, pivotal for offering personalized care and support. The template covers a broad spectrum of areas crucial for a comprehensive evaluation, including Psychiatric History, Physical Health, and Substance Use, among others, ensuring that individuals receive holistic care. It’s a product of collaborative input, developed to be person-centered and recovery-oriented, drawing upon expertise from leading figures in mental health practices. Furthermore, the WA-PACT Standards underscore the importance of ongoing assessment, advocating for adaptability and sensitivity in the engagement with consumers. This approach not only respects the regional autonomy in public mental health services but also underscores the importance of incorporating consumer perspectives and experiences into the assessment process, thereby enriching the understanding and delivering more effective care strategies tailored to individual needs. This template stands as a testament to Washington State’s commitment to enhancing mental health services, offering a framework that prioritizes comprehensive, compassionate, and consumer-directed care.
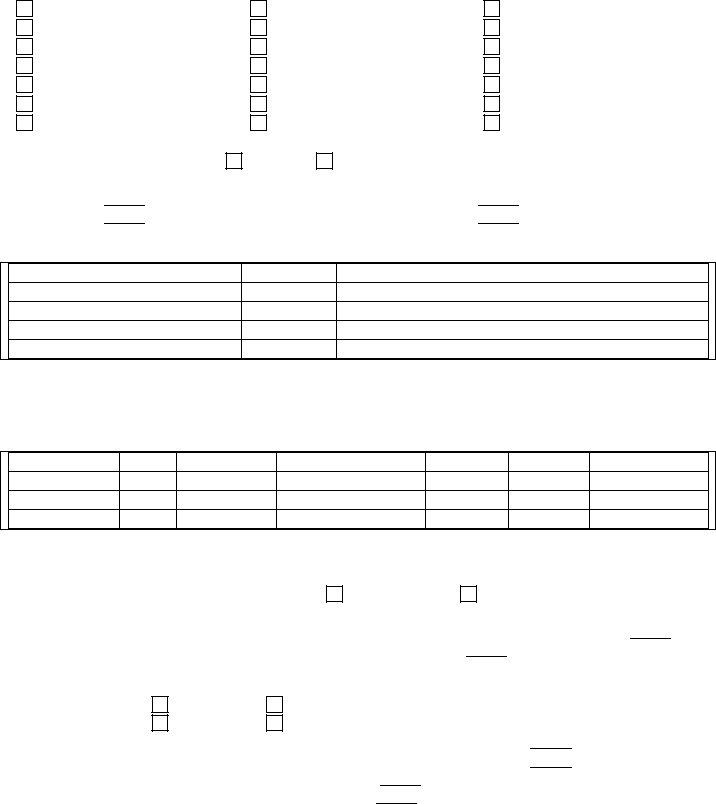
| Question | Answer |
|---|---|
| Form Name | Washington Pact Form |
| Form Length | 37 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 9 min 15 sec |
| Other names | how to comprehensive template, washington pact, pact wa how, pact wa |

Template
Overview
Given the local variation and regional authority in oversight of public mental health services in Washington State through the Regional Support Network (RSN) structure, the Washington State PACT
In recognition of this regional variation, the Washington Institute continues to develop and improve upon a template that may be used by PACT teams for completion of their Comprehensive Assessments. Please note that use of this template is NOT REQUIRED, as long as each team is assessing across the eight core areas specified within the
This updated template continues to follow the eight required areas of assessment, but with a more person- centered,
General Guidelines & Considerations for Completion of the Comprehensive Assessment:
•While the
•If engagement is an issue, you may want to prioritize the assessment areas that are most engaging to a consumer at enrollment, focusing on
•Don’t be limited to completing the assessment in one or two
•Be comfortable but sensitive to consumer reactions to questions. Assessments may be open to change and/or new information over time.
•All specialists should be contributing assessment information and as such, team members should look across specialty areas.
•Utilize client voice in direct quotes whenever possible to reflect attempts to gather information. Example: “I don’t have mental illness.” This helps ensure accuracy of assessment within the first 30 days.
Considerations for Assessing Substance Use in Part 3:
•Use assessment principles and practices consistent with Integrated Dual Disorders Treatment and Motivational Interviewing to assess consumers’ use and abuse of substances.
•In particular, remember that the first goal of substance abuse assessment within a PACT team is to facilitate an environment in which the consumer feels it is safe to talk openly with the team about substance use. Toward this end, Motivational Interviewing methods are especially helpful (e.g., using
•Specific substance abuse assessment forms, such as the Functional Analysis form and the Payoff Matrix, can be completed collaboratively with the consumer or completed initially by staff.
We hope that you find this updated template more purposeful and engaging for new PACT consumers admitted to the program.
For further questions and/or consultation on completion of the

Name: |
|
Chart #: |
Date:
Part 1: Mental Health & Psychiatric Symptoms
Including Psychiatric History Timeline, Mental Status, and Diagnosis
A. Mental Health & Psychiatric Symptoms
What are your most troubling psychiatric symptoms? How much do they interfere with your life? Are they getting in the way of the things you’d like to do?
How do you cope with your symptoms? What do you do to stay well? How much are your medications helping you?
If you want to make changes, what are they? What are your goals for maintaining your mental health?
What are the barriers keeping you from being as psychiatrically healthy as possible (e.g. side effects of medications, etc.)? How could the PACT team help you?
B. Mental Status Exam |
|
|
|
|
|
|
|
|
|
|
|
Presentation |
1. |
|
Clothing |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2. |
|
Other physical characteristics |
|
|
|
|
|
|
|
|
|
3. |
|
Openness to assessment |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
4. |
Consciousness (awareness, responsiveness, attentiveness) |
|
||
|
|
|
|
|
|
|
|
|
|
|
|
Posture |
5. |
|
Slumped |
|
|
|
|
|
|
|
|
|
6. |
|
Rigid, tense |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
7. |
|
Other |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
General Body |
8. |
|
Accelerated, increased |
|
|
Movements |
|
|
|
|
|
|
9. |
|
Decreased, slowed |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
10. |
Restless, fidgety |
|
||
|
|
|
|||
|
|
|
|
|
|
Amplitude & Quality |
11. Increased, loud |
|
|||
of Speech |
|
|
|
|
|
|
12. |
Decreased, slowed |
|
||
|
|
|
|
||
|
|
|
|
|
|
|
13. |
Slurred, stammering, etc. |
|
||
|
|
|
|||
|
|
|
|
|
|
Emotional State |
14. Different from thought content |
|
|||
|
|
|
|
|
|
|
15. Labile |
|
|||
|
|
|
|||
|
|
|
|
|
|
Predominate Mood |
16. Lessened emotion, “feeling nothing” |
|
|||
|
|
|
|||
|
|
|
|
|
|
|
17. Euphoria |
|
|||
|
|
|
|||
|
|
|
|
|
|
|
18. Anger, hostility |
|
|||
|
|
|
|||
|
|
|
|
|
|
|
19. Fear, anxiety, apprehension |
|
|||
|
|
|
|||
|
|
|
|
|
|
|
20. Depression, sadness |
|
|||
|
|
|
|
|
|
|
21. Panic attacks or symptoms |
|
|||
|
|
|
|
|
|
|
|
|
|
|
Facial Expression & |
|
22. Anxiety, fear, apprehension |
|
|
Overall Physical |
|
|
|
|
Behavior |
|
23. Depression, sadness |
|
|
|
|
|
|
|
|
|
|
|
|
|
24. |
Anger, hostility, irritability |
|
|
|
|
|
|
|
|
|
|
|
|
|
25. |
Decreased variability of expression, blunted, unvarying |
|
|
|
|
|
|
|
|
|
|
|
|
|
26. |
Elated |
|
|
|
|
|
|
|
|
|
|
|
|
Perception |
|
27. Illusions |
|
|
|
|
|
|
|
|
|
|
|
|
|
28. |
Hallucinations |
|
|
|
|
|
|
|
|
|
|
A. Auditory hallucinations |
|
|
|
|
|
|
|
|
|
B. Visual hallucinations |
|
|
|
|
|
|
|
|
|
C. Other hallucinations |
|
|
|
|
|
|
|
|
|
|
|
Thought Content |
|
29. Obsessions |
|
|
|
|
|
|
|
|
|
|
|
|
|
30. |
Compulsions |
|
|
|
|
|
|
|
|
|
|
|
|
|
31. |
Phobias |
|
|
|
|
|
|
|
|
|
|
|
|
|
32. |
Derealization |
|
|
|
|
|
|
|
|
|
|
|
|
|
33. |
Depersonalization |
|
|
|
|
|
|
|
|
|
|
|
|
|
34. |
Suicidal Ideation |
|
|
|
|
|
|
|
|
|
|
|
|
|
35. |
Homicidal Ideation |
|
|
|
|
|
|
|
|
|
|
|
|
|
36. |
Delusions |
|
|
|
|
|
|
|
|
|
|
|
|
|
37. |
Ideas of reference |
|
|
|
|
|
|
|
|
|
|
|
|
|
38. |
Ideas of influence |
|
|
|
|
|
|
|
|
|
|
|
|
Stream of Thought |
|
39. Associations |
|
|
|
|
|
|
|
|
|
|
|
|
|
40. |
Thought flow decreased, slowed |
|
|
|
|
|
|
|
|
|
|
|
|
|
41. |
Thought flow increased |
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
Intellectual |
42. Fund of common knowledge |
|
|
Functioning |
|
|
|
|
43. |
Abstract thinking |
|
|
|
|
|
|
|
|
|
|
44. |
Calculations ability |
|
|
|
|
|
|
|
|
|
|
45. |
Comprehension |
|
|
|
|
|
|
|
|
|
Orientation |
46. Person |
|
|
|
|
|
|
|
|
|
|
|
47. |
Place |
|
|
|
|
|
|
|
|
|
|
48. |
Time |
|
|
|
|
|
|
|
|
|
Attention |
49. Concentration on mental or practical tasks |
|
|
|
|
|
|
|
|
|
|
Memory |
50. Immediate recall |
|
|
|
|
|
|
|
|
|
|
|
51. |
Recent memory |
|
|
|
|
|
|
|
|
|
|
52. |
Remote memory |
|
|
|
|
|
|
|
|
|
Insight |
|
|
|
|
|
|
|
Judgment |
|
|
|
|
|
|
|
Mental Status Summary:
C. DSM IV
Axis I ______________________________________________________________
______________________________________________________________
______________________________________________________________
______________________________________________________________
Axis II ______________________________________________________________
______________________________________________________________
______________________________________________________________
Axis III _____________________________________________________________
_____________________________________________________________
_____________________________________________________________
Axis IV Primary Support |
Occupational |
Health Care |
Social Environment |
Housing |
Legal System/Crime |
Educational |
Economic |
Other _____________ |
Axis V __________ |
|
|
Assessment Summary |
|
|
Strengths/Resources
Completed by: _____________________________________ |
Date Completed: ____________ |
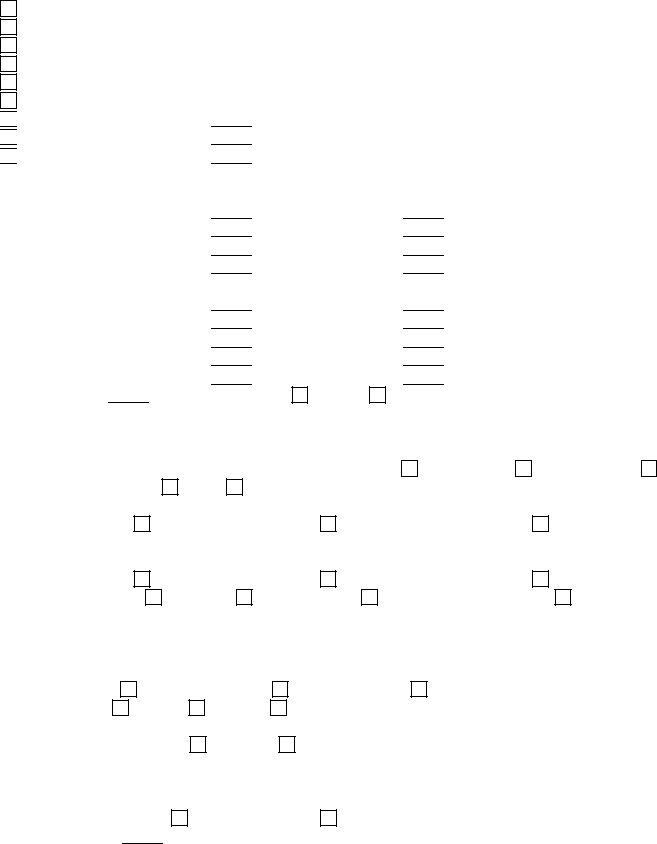
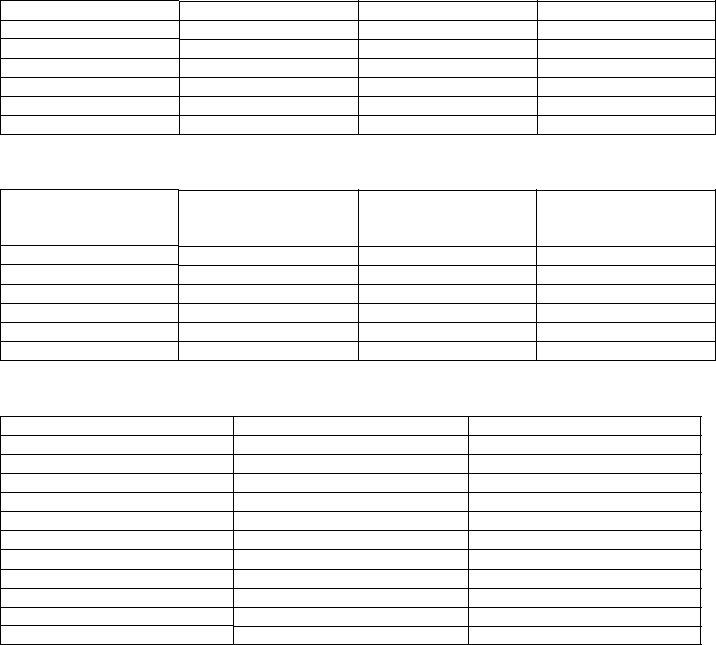
Comprehensive Time Line
Consumer Name
DOB
Marital Status
Education
Records Reviewed
Records Needed
Comprehensive Time Line
Admit/
DC Dates
Treatment
Provider
Presenting Problems/
Legal Status
Diagnosis
Medications
Services Received
Reasons for DC/
Recommendations
Living
Situation
Employment
Other
Comments
Name: |
|
Chart #: |
|
|
|
Date: |
|
|
|
|
|
Part 2: Physical Health
Do you have any specific medical problems or concerns about your health? Are you getting enough rest and exercise? If you smoke, are you interested in trying to quit?
If you want to make changes, what are they? What are your goals for staying healthy?
What are the barriers keeping you from being as healthy as possible? How could the PACT team help you with this area?
Name: __________________________________
Current Doctor and Dentist: |
|
|
|
|||||
1. |
General Physician: |
|
|
Address: |
||||
2. |
Dentist: |
|
|
|
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
3.Serious Illnesses and Disorders:
|
Heart disease |
Gallstones |
Diabetes |
|
|
High blood pressure |
Kidney infections |
Arthritis |
|
|
Emphysema |
Kidney stones |
Glaucoma |
|
|
Asthma |
Stomach ulcers |
Gout |
|
|
Liver disease |
Thyroid disorder |
Cancer |
|
|
Cirrhosis |
Anemia |
HIV / AIDS |
|
|
Hepatitis |
Rheumatic fever |
Other: |
|
4. Seizure Activity: |
Yes |
Frequency:
Last seizure:
No
Duration:
Type:
5.Previous Medical Hospitalizations
Hospital Name / Address
Date
Reason (e.g., injuries, surgery, tests and procedures)
Current Medications
6.List the medications taken NOW, dosage, frequency, reason for taking, when started, last date taken and prescribing physician.
Medication
Dose
Frequency
Reason
Start Date
End Date
Prescriber
Allergies |
|
|||
7. |
Do you have any known allergies? |
Yes |
||
8. |
If so, describe allergies to: |
|
||
|
Medications |
|
|
|
|
Foods |
|
|
|
No
Hay Fever or Allergic Rhinitis Other
Family Health |
|
|
|
|
|
|
|
|
|
|
|
|
9. |
Father: |
Living |
Deceased |
Age, or age at death |
|
|
||||||
10. |
Mother: |
Living |
Deceased |
Age, or age at death |
|
|
||||||
11. |
Sisters: |
Number Living |
|
|
Number deceased |
|
Causes if deceased |
|||||
12. |
Brothers: |
Number living |
|
|
|
|
Number deceased |
|
Causes if deceased |
|||
13.Children (number, names, and dates of birth/ages)
Number Deceased |
|
Causes if Deceased |
|
|
Name: __________________________________ |
||
Disease in Your Family |
|
Relation of Family Member |
||
14. |
Heart Disease |
|
|
|
15. |
Diabetes |
|
|
|
16. |
Glaucoma |
|
|
|
17. |
Cancer |
|
|
|
18. |
Goiter |
|
|
|
19. |
High Blood Pressure |
|
|
|
20. Mental Illness
21. Substance Abuse
22. Other
Most Recent Exam |
Date |
23.Physical Exam
24.Chest
25.Hearing Exam
26.Pelvic Exam/Pap Smear
27.Lab Work
Blood Chemistry
CBC
Hepatitis Antibody Screen
Urinalysis |
|
HIV Assay |
|
TB Skin Test |
Reaction: Negative |
Ordering Physician
Positive
Physical Information |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
28. |
Ht. |
|
Wt. |
|
|
|
|
|
|
|
|
Usual Wt. |
|
|
Normal Weight |
|
Overweight |
Underweight |
||||||||||||||||||||||||
29. |
T. |
|
|
P. |
|
|
|
|
reg |
irreg |
R. |
|
|
BP. |
|
|
|
|
||||||||||||||||||||||||
30. |
Hair: Color |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Condition |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
31. |
Hearing: Adequate |
|
|
|
Impaired Partial |
Impaired Complete |
|
|
||||||||||||||||||||||||||||||||||
|
Hearing Aid |
|
|
|
|
|
|
|
|
Type |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
32. |
Eyes: |
Color |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
Vision: |
Adequate |
|
|
|
Impaired Partial |
Impaired Complete |
|
|
|||||||||||||||||||||||||||||||||
|
Vision Corrected: Yes |
|
|
|
No |
Glasses |
|
|
Contact Lenses |
|
|
|||||||||||||||||||||||||||||||
|
Optician/Ophthalmologist: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
Most recent vision exam: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
Glasses purchased at: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
33. |
Teeth: |
Natural |
|
|
|
|
|
|
|
Good Condition |
Poor Condition |
|
|
|||||||||||||||||||||||||||||
|
Dentures: Upper |
|
|
|
|
Lower |
|
|
|
Partial |
Orthodontic Appliance: |
|
|
|||||||||||||||||||||||||||||
|
Most recent dental exam: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
34. |
Ambulation: |
Unassisted |
|
|
|
Assisted |
Specify |
|
Prosthesis: Type |
|
|
|||||||||||||||||||||||||||||||
|
Corrective Devices: Type |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
35. |
Skin: Condition |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
Notable features (e.g., scars, bruises, tattoos, birthmarks) and location |
|
|
|||||||||||||||||||||||||||||||||||||||
36. |
Bowel Habits: |
Regular |
|
|
|
|
|
Irregular |
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
Bowel Medication:

|
Name: __________________________________ |
|||
Questions for Women Only: |
|
|
|
|
37. |
Are you having your menstrual periods? |
|
Yes |
No |
38. |
When was your last period? Month/Year |
|
|
|
39. |
Are your periods regular? |
|
Yes |
No |
40.If yes, how many days do they last?
41.How many days between periods?
42. |
Do you examine your breasts regularly? |
Yes |
No |
|
|
|||
43. |
Have you ever been pregnant? |
Yes |
No |
|
|
|||
|
Number of pregnancies: Births |
|
|
Abortions |
|
Miscarriages |
|
Still Births |
44.Do you presently have any noticeable vaginal discharge or discomfort?
45.Have you ever been treated for a yeast infection?
Sexual
46.Do you have any sexual concerns?
47.Which is most true?
|
I have sex with people of a different sex. |
|
|
|
|
|
|
||||||
|
I have sex with people of the same sex. |
|
|
|
|
|
|
||||||
|
I have sex with both males and females. |
|
|
|
|
|
|
||||||
48. |
Where did you acquire your sex information? |
|
|
|
|
|
|
||||||
49. |
Would you like information related to bodily function, performance, birth control? Yes |
No |
|||||||||||
50. |
Are you using any birth control methods at the present time? |
Yes |
No |
|
|||||||||
|
Partner |
|
Self |
Type |
|
|
Length of time |
|
|
|
|
||
51. |
If not, have you used any birth control methods in the past? |
Yes |
No |
|
|||||||||
|
What kind? |
|
|
|
|
|
|
|
|
|
|
|
|
|
Why did you discontinue its use? |
|
|
|
|
|
|
|
|
|
|
||
52.Did you plan on using any birth control in the future?
53.Are you aware of signs and symptoms of sexually transmitted diseases?
54.Have you ever suspected you have, had, or have you been treated for:
Syphilis |
Chlamydia |
Gonorrhea |
Herpes |
HIV Infection (ARC, AIDS) |
Do you know and/or use measures (e.g., condoms) to prevent sexually transmitted diseases?
55.Have you ever been sexually assaulted or abused?
56.Have you ever been treated for injuries connected with the above?
Summary of Significant Physical Conditions
Recommendations for Immediate Care & Diagnostic Treatment
Strengths/Resources
Completed by:___________________________________________ |
Date: ____________ |

Name: __________________________________
Name: |
|
Chart #: |
|
|
Date: |
Part 3: Use of Drugs or Alcohol
Do drugs and/or alcohol influence your life right now? If so, how? (if person alludes to possible substance abuse or dependence, utilize assessment questions on page 2)
If you want to make changes, what are they? What are your goals for reducing or eliminating your use of drugs and alcohol and/or decreasing the harmful effect they have on your life?
What are the barriers to reaching these goals? (e.g. all my friends use, there are a lot of drugs in my building) How could the PACT team help you with your goals?)

Name: __________________________________
ASSESSMENT QUESTIONS
1.People use alcohol and street drugs for different reasons. What would you say are the reasons that you drink? That you use street drugs?
2.When you first started drinking/using, how much did you have to drink/use to feel drunk/high?
3.How much does it take for you to feel drunk/high now?
4.Do you find that using alcohol or drugs relieves tremors, shakes, sweating, anxiety, sleep problems, or hallucinations? Which ones?
5.Have you ever drank or used more than you originally planned?
6.Have you ever tried to cut down or quit drinking or using and found that you were unable to do
so? Yes |
No |
7.How much of your day do you think about drinking/using/coming down from using?
8.What is the longest you have been able to stay clean and sober?
9.How did you do it? What was helpful to you?
10.Have you ever been in treatment for alcohol or drug use?
11.What are the situations or times in which you DON’T use?
12.What do you think about continuing to use (assess his/her motivations or intentions concerning usage):
13.Describe the client's “islands of health” (those dreams, goals, values, strengths, aspects of the persons life that might be discrepant with drinking or drugging or be used as levers for change)
Name: __________________________________
CLINICIAN RATING SCALES:
SUBSTANCE ABUSE TREATMENT SCALE (SATS)
Client ID:____________________ Rating Date:___________
Instructions: Circle the most appropriate number. This scale is for assessing a person’s stage of substance abuse treatment, not for determining diagnosis. The reporting interval is the last six months. If the person is in an institution, the reporting interval is the time period prior to institutionalization.
1.
2.Engagement The person has had only irregular contact with case manager or counselor, and meets criteria for substance abuse or dependence.
3.Early Persuasion The person has regular contacts with a case manager or counselor, continues to use the same amount of substances or has reduced substance use for less than 2 weeks, and meets criteria for substance abuse or dependence.
4.Late Persuasion The person has regular contacts with a case manager or counselor, shows evidence of reduction in use for the past
5.Early Active Treatment The person is engaged in treatment and has reduced substance use for more than the past month, but still meets criteria for substance abuse or dependence during this period of reduction.
6.Late Active Treatment The person is engaged in treatment and has not met criteria for substance abuse or dependence for the past
7.Relapse Prevention The person is engaged in treatment and has not met criteria for substance abuse or dependence for the past
8.In Remission or Recovery The person has not met criteria for substance abuse or dependence for more than the past year.
9.Not Applicable No substance use disorder
Comments: ____________________________________________________________

Name: __________________________________
CLINICAN’S RATING SCALES:
Alcohol Use Scale (AUS)
Initial rating will be based on
Client ID:____________________ Rating Date:____________
1.Abstinent: no use of alcohol during this time period.
2.Use without impairment: use of alcohol during this time period but no evidence of persistent or recurrent problems related to use or dangerous use.
3.Abuse: use of alcohol and evidence of persistent or recurrent problems related to use or recurrent dangerous use.
4.Dependence: meets at least three of the following: greater amounts or intervals of use than intended, much of time used obtaining or using substance, frequent intoxication or withdrawal interferes with other activities, important activities given up because of alcohol use, continued use despite knowledge of alcohol or
5.Dependence with Institutionalization: Problems related to dependence are so severe that they make
CLINICIAN ALCOHOL USE RATING:
Name: __________________________________
CLINICAN’S RATING SCALES:
Drug Use Scale (DUS)
Initial rating will be based on client
Client ID:____________________ Rating Date:____________
1.Abstinent: no use of drugs during this time period.
2.Use without impairment: use of drugs during this time period but no evidence of persistent or recurrent problems related to use or dangerous use.
3.Abuse: use of drugs and evidence of persistent or recurrent problems related to use or recurrent dangerous use.
4.Dependence: meets at least three of the following: greater amounts or intervals of use than intended, much of time used obtaining or using substance, frequent intoxication or withdrawal interferes with other activities, important activities given up because of drug use, continued use despite knowledge of alcohol or
5.Dependence with Institutionalization: Problems related to dependence are so severe that they make
CLINICIAN DRUG USE RATING: ___________
Identify drugs used:___________________________________
Name: __________________________________
MY RELAPSE PREVENTION PLAN:
1.Relapse Risk Factors:
2.Lifestyle factors (e.g., high stress):
3.My external triggers: ( people, places, things, times, dates, events):
4.Actions and decisions I make that set me up for relapse ( e.g., hanging out with people who use, going to drinking parties, telling myself that drinking a little won’t hurt):
5.Slips/lapse contingencies:
6.The likely
7.The likely
8.Health lifestyle/wellness: What I can do to prevent relapse (daily meditation or prayer, regular exercise):
9.Ways I can prevent or avoid experiencing these triggers:
10.Skills I can use to cope with these triggers if I do experience them, i.e. what I can think, actions I can take:
11.Alternative choices and decisions I can make:
12.People I can ask for support:
13.Other supports I think I need:
14.Resources I can use (for instance, AA):
15.If I do slip or lapse, what do I need to think and do?
Strengths/Resources:
Completed by: ___________________________________________ |
Date:________ |

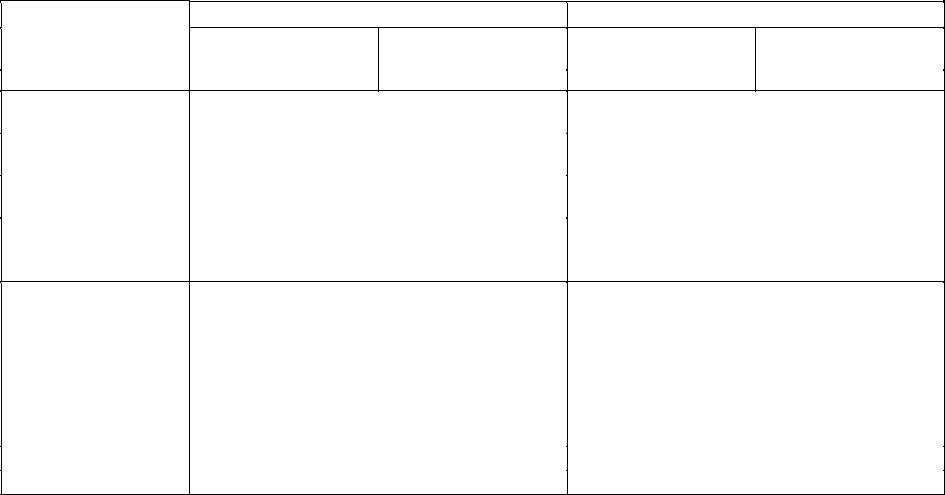
Functional Analysis Form
I. Triggers |
II. Responses |
|
III. Consequences |
|
||
|
|
|
|
|
||
Situations, places, |
Thoughts, feelings, |
(Choices, decisions, |
Immediate |
Delayed or long- |
||
times, etc |
urges, moods, etc |
actions, etc.) |
|
|
|
term |
|
|
|
Positive |
Negative |
Positive |
Negative |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Name: __________________________________
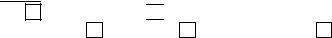
PAYOFF MATRIX
Name:
Date:
Using
Not Using
Immediate
Delayed or Long Term
Immediate
Delayed or Long Term
Advantages
Disadvantages

Name: |
|
Chart #: |
|
|
Date: |
Part 4: Money, Employment & Education
A.Money/Finances
What are your sources of income? What do you usually spend your money on? Do you have enough money to do the things you would like to do?
How do you mange your money? Do you have a budget?
If you want to make changes, what are they? In terms of money, what would your ideal situation be (if different from what it is now)?
What are the barriers keeping you from being in the financial situation you want to be in? How could the PACT team help you?
Name: ______________________________________
B.Employment
Are you working right now? If so, where? Are you happy with this job? Where have you worked in the past? Are you interested in getting a new or different job now?
If you want to make changes, what are they? What kind of work situation would you like to be in (if different from where you are now)? What would be your ideal job?
What did you like about past jobs? What do you feel your best job skills are? Are you interested in getting a new or different job now?
What are the barriers keeping you from being in the work situation you want to be in? How could the PACT team help you with this?
Name: ______________________________________
C.Military History
Have you ever been in the military? If so, what branch?
Dates of Service: Combat action? Yes
Type of Discharge: Honorable
No General
Dishonorable
D.Education
Are you satisfied with your education? Do you feel you have the training you need to do the kind of work you want to do? Are there things you would just like to learn more about?
If you want to make changes, what are they? What are your goals for education/training?
What are the barriers keeping you from getting the education/training you want? How could the PACT team help you with this?
Name: ______________________________________
Strengths/Resources:
Completed by: ____________________________ |
Date:________ |

Name: ______________________________________
Name: |
|
Chart #: |
|
|
Date: |
Part 5: Social Development and Functioning
A.Social Development History
Early Childhood
How would you describe your childhood? Who raised you? Describe your friendships as a young child.
Adolescence
What were your adolescent/high school years like? What did you do for fun during adolescence/high school? Did you drink or use drugs? Did your friends drink or use drugs? Describe your friendships during your teenage years. Did you date in high school?
Adulthood
Who are the most important people in your life now? Tell me a little bit about these people. (Who are the people you feel you can turn to or lean on? Who are the people who most believe in you? Are there people who depend on you? What kinds of qualities do you bring into a relationship?)
Are you happy with your friendships right now? Are you happy with your dating life or romantic relationships? What would help you to enjoy them more (e.g., spend more time with friends, feel more comfortable in social situations)?
Name: ______________________________________
B.Culture
What is your family’s nationality or ethnic origin? Father? Mother? How long have you or your family lived in this country? When did your family immigrate? Calculate immigrant generational status (e.g.,
first generation).
What language do you speak at home? In the community? Assess level of cultural assimilation* (Monocultural=new immigrant, Bicultural=balancing and integrating nondominant culture; Unicultural=assimilated to the point of no longer identifying with ethnic background).
What does your culture/family say about education? What do they say about work? Family and child- rearing practices?
What does your family/culture say about mental health needs? How does your family respond to your mental health needs? Do you feel you or your family have ever been misunderstood or misinterpreted by mental health providers because of cultural or ethnic differences?
Do you think you have experienced discrimination because of your culture or ethnic background? If so, how?
Name: ______________________________________
C.Spirituality
How important is faith/spirituality in your life? What are some of your spiritual practices? How satisfied are you with your opportunities to participate in your spiritual practice or attend the congregation of your choice right now? Do you belong to a spiritual community or would you like to?
If you want to make changes, what are they? What are your spiritual goals? How could the PACT team help you reach these goals?
E. Legal Involvement
Are you dealing with any legal issues right now? If your legal issues are bothering you, how can we help?
Name: ______________________________________
The following is a list of situations. Please read the situation and then rate how easy it is for you.
1=very easy |
2=sometimes easy |
3=often difficult |
1.Walking down the street
2.Being with your family
3.Riding city bus
4.Being with older people
5.Going into bars
6.Mixing with people at work
7.Being in a crowd
8.Expressing anger
9.Making friends your own age
10.Talking about your feelings
11.Having someone over to your place
12.Starting a conversation
13.Going to social gatherings
14.Meeting new people
15.Asking for assistance
16.Being alone
17.Answering questions
18.Spending time with men
19.Spending time with women
20.Going into stores
21.Being criticized by someone
22.Making a mistake
23.Going on a date
24.Saying “No” to a friend
25.Talking to a work supervisor
26.Keeping friends
Name: ______________________________________
Please check the things you would like to do during the next six months or at some time in the future.
I would like to:
move to a new apartment study photography save money
get my driver’s license buy a car
meet some men finish school play basketball
get special job training improve my cooking
go camping play cards
have more money buy a TV
go bowling
go to see plays learn relaxation go to concerts play pool
get a roommate
get a volunteer job
enter a contest
______________________
write poetry
______________________
go fishing
______________________
spend more time alone
______________________
meet some women live in a house get off of welfare
get along with my parents learn a skill
improve my grooming learn to job hunt
be less lonely maintain friendships communicate with parents
go to church drink less go on dates join a club
be more active
stop smoking eat better gain weight
call friends on the phone learn to be less anxious
visit relatives do painting
learn to knit
play baseball
lose weight
get a job
talk about feelings go to bars
be more assertive go to restaurants
go to movies drink less coffee learn to manage stress do woodworking have more friends
take a vacation get new clothes have a party learn to sew
open a bank account
get together with friends express my feelings
go on picnics
go see a baseball game be assertive with friends
go to the library other
other
other
other
Strengths/Resources:
Completed by:_________________________________ |
Date:________ |

Name: ______________________________________
Name: |
|
Chart #: |
|
|
Date: |
Part 6: Activities of Daily Living
A.Living Situation
What is your current living situation? Do you live alone, with roommates? How do you feel about your place and your neighborhood?
If you want to make changes, what are they? What kind of living situation would you like to be in (if different from where you live now?
What are the barriers keeping you from being in the living situation you want to be in? What kind of help would you like?
Name: ______________________________________
B.Daily Living and Routine
How do you spend your day? What does a “typical” day look like? Is this satisfying/enjoyable for you? Are there places in the community where you feel comfortable and safe?
If you want to make changes, what are they? What would your ideal day look like? How/where and with whom would you like to be spending your time? What kind of things do you like to do that you aren’t doing now?
What are the barriers keeping you from spending your time the way you would want? How could the PACT team help you with these?
Name: ______________________________________
C.Housekeeping, Diet/Nutrition, Laundry, Transportation
What housekeeping tasks do you enjoy the most? The least? Do you have access to laundry facilities?
What type of meals do you like? Where do you get your food currently?
How do you get to your appointments and activities?
If you’d like to change any of these areas (housekeeping, nutrition, laundry, transportation), what would they look like?
What are the major barriers to make these changes? How could the PACT team help you with these areas?
Strengths/Resources:
Completed by:_________________________________ |
Date: ________ |

Name: ______________________________________
Name: |
|
Chart #: |
|
|
Date: |
Part 7: Family and Relationships
Who are the most important people in your life right now? Are there people you can turn to when things get difficult? Are there people that depend on you?
How are your friendships going? How are your family relationships going? Do you have (or hope to have) a romantic or sexual
If you want to make changes, what are they? Would you like to make new relationships or improve your current relationships?
What are the barriers to forming or improving relationships? How could the PACT team help you with this?
Name: ______________________________________
List all names of the members of the family of origin (i.e., parents and siblings) and of spouse or partner:
Name
Relationship
Address and Telephone
Age
List the names of Children:
Name
Relationship
Birth Date and Age
Address and Telephone (if minor, whom are they living with)
Significant Others:
Name
Relationship
Age
Strengths/Resources:
Completed by: ____________________ |
Date: _________ |
Name: ______________________________________
Name: |
|
Chart #: |
|
|
|
Date: |
|
|
|
|
|
Part 8: Strengths and Resources
A.Hopes and Dreams
What are your hopes and dreams for the future? What are some of the most important things you want to have in your life?
If you could change anything in your life right now, what would it be?
B.Personal Strengths
To help you meet your goals, we need to think about what strengths you have. Sometimes people have a hard time remembering their strengths. The following statements may help you get ideas:
1.My best qualities as a person are…
2.Something I would NOT change about myself is…
Name: ______________________________________
3.The times I am most at peace are when…
4.People like that I am (people say they like my…)
5.I help other people out by… (Something I give to others that makes me feel good is…)
6.I admire people who are…
7.I notice my problems least when I am…
8.The kinds of things I’d like to change in my life are…
Name: ______________________________________
D. Other Issues
Are there other issues that are important in your recovery that we have not covered so far? Are there any other issues or areas in your life where you’d like to make changes?
If you want to make changes, what are they? What are your goals in this area?
What are the barriers for reaching this goal? How could the PACT team help you?
Completed by:_______________________ |
Date:______ |