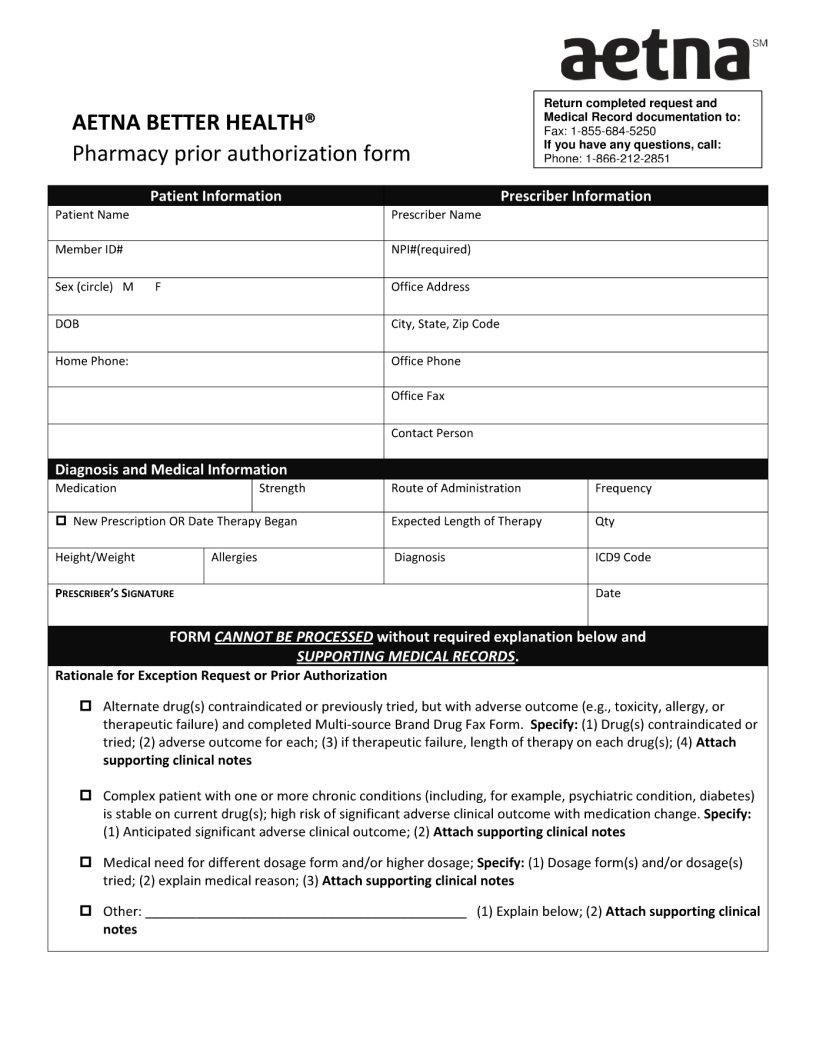
When it comes to managing healthcare expenses, understanding the process of getting necessary medications can be both important and overwhelming. This is where the Aetna Pharmacy Prior Authorization form comes into play, acting as a pivotal document for many patients. Essentially, this form is a tool used by healthcare providers to request approval from Aetna for the coverage of specific medications that may not automatically be covered under a patient's pharmacy benefit plan. The process involves a detailed review by Aetna, wherein they assess the necessity of the prescribed medication against their coverage policies. This form must be accurately completed and submitted by a healthcare provider, detailing the medical reasons for the specific prescription. The outcome can significantly affect the patient's access to necessary medication, either enabling coverage by Aetna or requiring the patient to consider alternative treatments or payment methods. Understanding this process and form is crucial for patients navigating their healthcare plans and seeking to ensure their medication needs are met efficiently and affordably.
| Question | Answer |
|---|---|
| Form Name | Aetna Pharmacy Prior Authorization Form |
| Form Length | 2 pages |
| Fillable? | Yes |
| Fillable fields | 81 |
| Avg. time to fill out | 16 min 46 sec |
| Other names | aetna prior authorazation, aetna medicare prior authorization fax form2020, aetna blank prior authorization forms, medicare a and b prior authorization form |