The PDF editor that you can go with was designed by our leading computer programmers. You may submit the amerigroup appeal form file instantly and efficiently with our software. Merely keep up with the procedure to get going.
Step 1: Select the "Get Form Now" button to start out.
Step 2: You're now on the document editing page. You may edit, add content, highlight specific words or phrases, place crosses or checks, and insert images.
The PDF template you decide to fill out will contain the next segments:
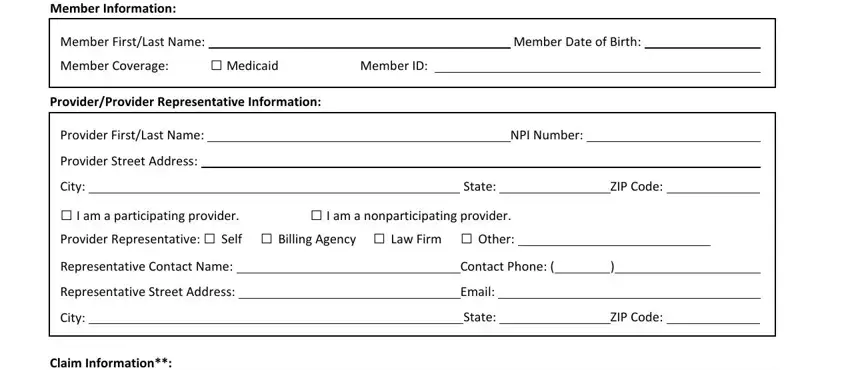
You should enter the particulars within the box Claim Number, Billed Amount, Amount Received, Start Date of Service, End Date of Service, Authorization Number, If you have multiple claims, Payment Appeal A payment appeal is, Claim code editing denial, Denied as duplicate Denial, OHI but member doesnt have OHI, and to your contract.
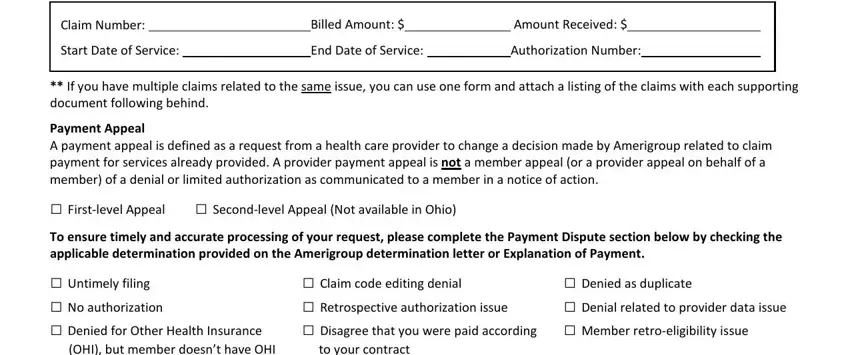
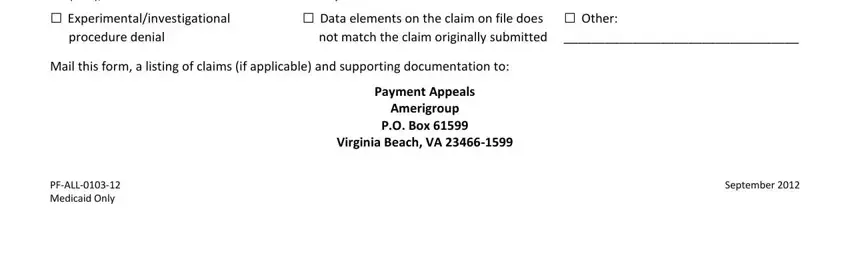
It's essential to point out the relevant details within the OHI but member doesnt have OHI, to your contract, Experimentalinvestigational, procedure denial, Data elements on the claim on, Other, Mail this form a listing of claims, Payment Appeals Amerigroup PO Box, PFALL Medicaid Only, and September area.
Step 3: Click "Done". You can now export your PDF form.
Step 4: To protect yourself from all of the issues in the long run, you will need to make around several duplicates of your form.