Navigating the complexities of healthcare services can be challenging, especially when dealing with Medicaid Managed Care in New Mexico. The Care Prior Authorization Request form plays a crucial role in this process, designed to streamline the approval of various healthcare services ranging from outpatient procedures to long-term care. This form requires detailed information about the member, including their name, date of birth, ID number, and coverage specifics, alongside the requesting provider's details. It also distinguishes between routine, urgent, or expedited requests, with the latter categories necessitating a provider's attestation regarding the immediacy of the member’s healthcare needs. To consider a request as urgent or expedited, it must be clearly stated that any delay in treatment could significantly impact the member's health or ability to recover fully. The form encompasses various service requests such as Durable Medical Equipment (DME), surgeries, inpatient care, and more, highlighting the necessity for attached clinical information to mitigate processing delays or outright denials. Moreover, it serves as a critical communication tool between healthcare providers and insurance entities, ensuring that all relevant clinical data supports the need for requested services, ultimately facilitating timely and appropriate care for Medicaid beneficiaries.
| Question | Answer |
|---|---|
| Form Name | Care Prior Authorization Request Form |
| Form Length | 1 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 15 sec |
| Other names | molina centennial prior authorization form, presbyterian centennial care prior authorization form, new mexico medicaid prior authorization form, blue cross blue shield centennial care prior authorization |
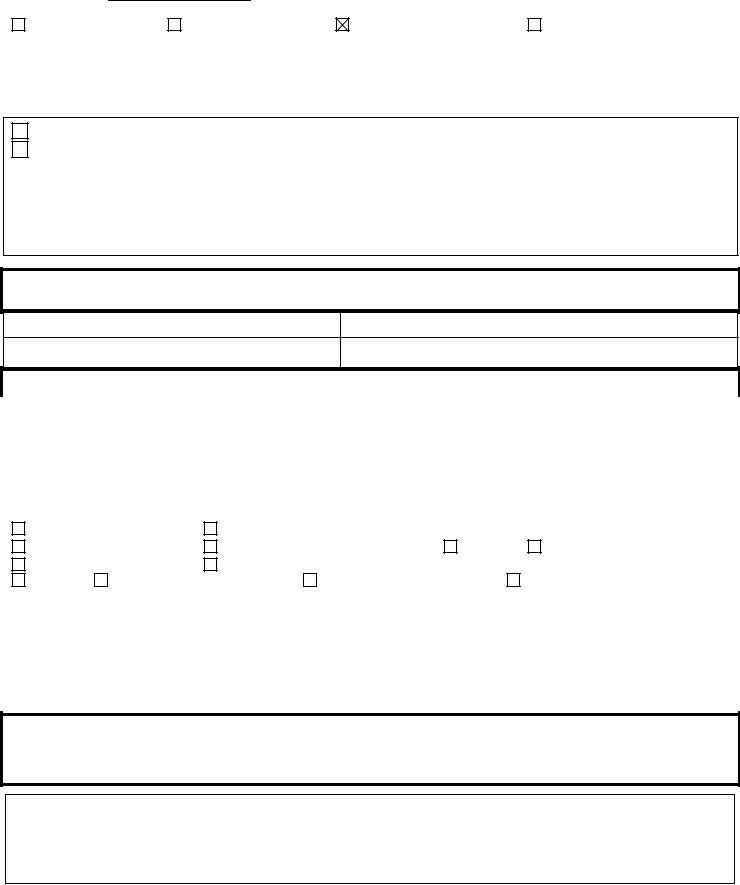
New Mexico Medicaid Managed Care
Prior Authorization Request Form
Request Date:
BCBS |
Molina |
Presbyterian |
United Healthcare |
Outpatient FAX: (505) |
Long Term Care FAX: (505) |
||
Inpatient FAX: (505) |
UNM FAX: (505) |
||
Phone: (505)
Routine
Urgent or Expedited Initial Determination
For a Prior Authorization request to be considered “Urgent” or “Expedited,” the request must include a provider’s order stating that waiting for a decision under a standard timeframe could endanger the member’s life, health, or ability to regain maximum functionality or would cause serious pain. Provider’s signature below is an attestation that this request meets expedited/urgent criteria listed here.
Practitioner Signature: |
|
(Required for Urgent or Expedited requests) |
Member Information: Complete the information below and attach all of the clinical information pertinent to the request.
Member Name:
Other Carrier:
ID Number: |
DOB: |
Policy/ID #: |
Phone No. |
|
|
Provider Information
|
Requesting Provider: |
|
|
Phone: |
|
|
|
Fax: |
|
|||
|
Servicing Provider/Facility: |
|
|
Phone: |
|
|
|
Fax: |
|
|||
|
Servicing Provider/Facility Address: |
|
|
|
|
|
|
|
|
|
|
|
|
Tax ID/NPI #: |
|
|
|
|
|
|
|
|
|
|
|
|
New/Initial Request |
Ongoing Care |
Previous Authorization Number: |
|
|
|
||||||
|
DME/Prosthetic/Orthotic |
Ambulatory/Outpatient Surgery |
|
Office |
|
Home Birth |
|
|||||
|
Inpatient LOS: |
|
Facility: |
|
|
|
|
|
|
|
||
|
PT/OT/ST Practitioner’s |
Order Attached |
Clinical Information Attached |
Other: |
|
|
|
|||||
|
Diagnosis(es) |
_________ |
_________ |
_________ _________ |
|
|||||||
Procedure (Must match CPT code/s):________________________________________________________
Procedure(s) (CPT/HCPC) (Required): _________ _________ _________ _________ _________
Requested Effective Date: ___________ |
End Date: ___________ |
Number of Visits/Units: ________ |
Please attach all supporting clinical information to include symptoms, past medical history, diagnostic testing, conservative treatment prior to request.
Services requested. Submit all relevant clinical data to support the request for services. Failure to provide supporting documentation will delay processing and may result in a denial.
For Health Plan Use ONLY: (this would be to communicate authorization information)
[MPC121322] |
[CENTENNIAL CARE # 389] |