The express scripts prior auth filling in procedure is simple. Our PDF tool allows you to work with any PDF form.
Step 1: The initial step would be to select the orange "Get Form Now" button.
Step 2: Now it's easy to modify your express scripts prior auth. This multifunctional toolbar lets you insert, remove, change, and highlight text or perhaps perform other sorts of commands.
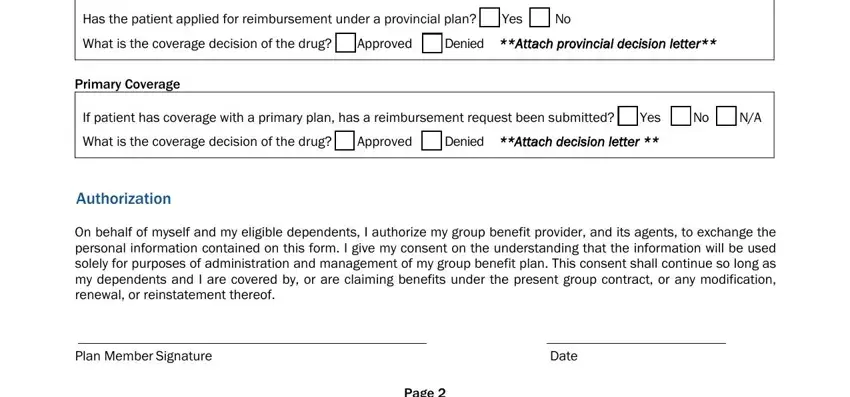
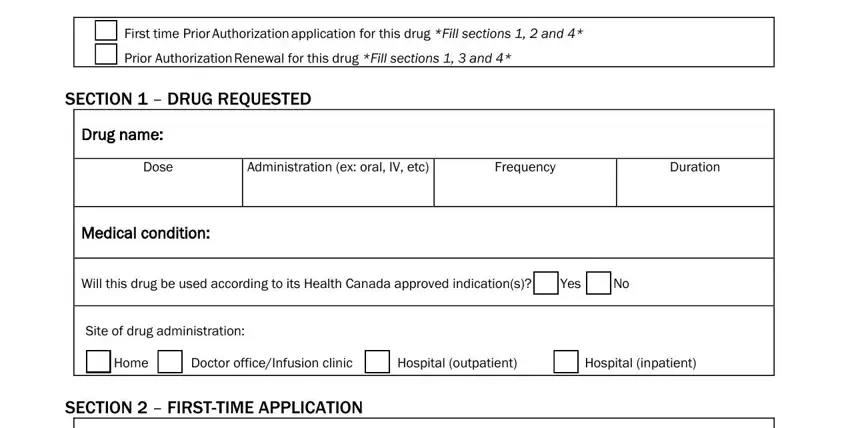
For every single part, create the details requested by the application.
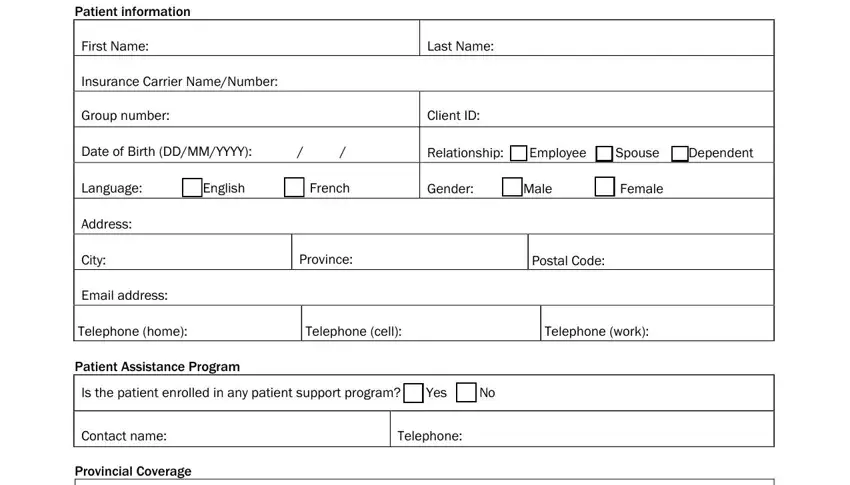
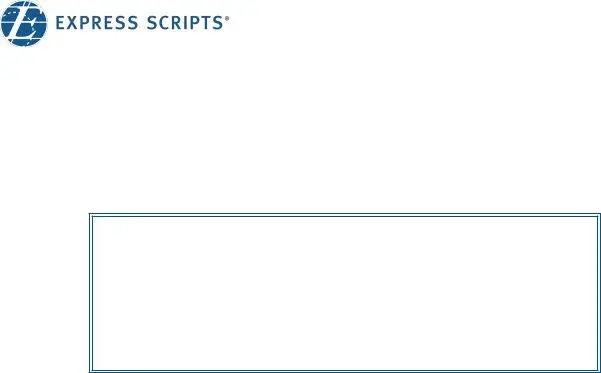
The program will require you to fill in the Has the patient applied for, Yes, What is the coverage decision of, Approved, Denied Attach provincial decision, Primary Coverage, If patient has coverage with a, Yes, What is the coverage decision of, Approved, Denied Attach decision letter, Authorization, On behalf of myself and my, Plan Member Signature, and Date section.
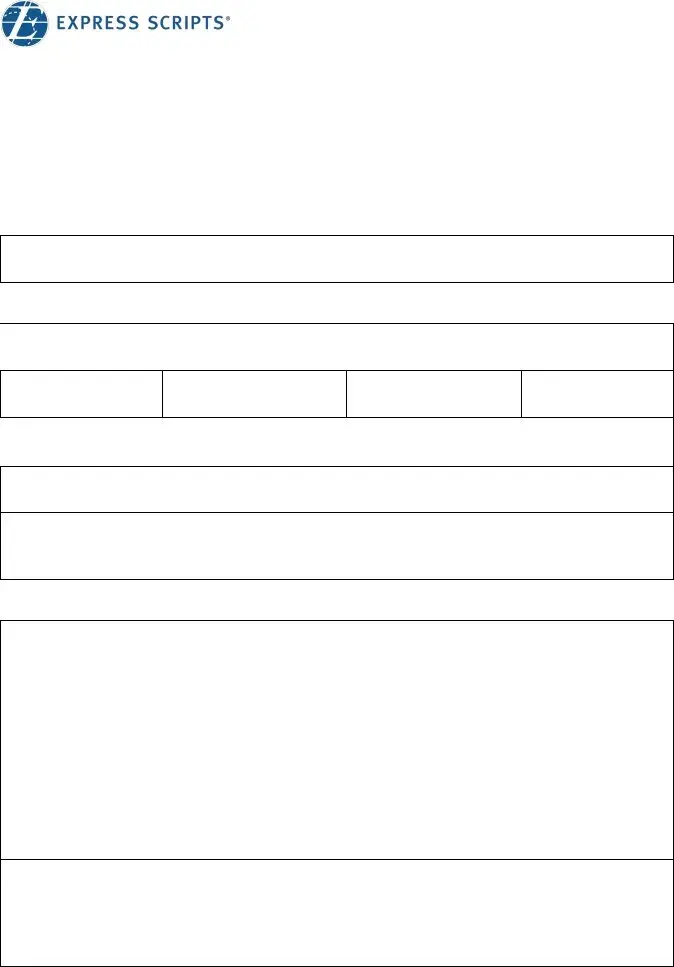
The system will ask you to put down some important info to instantly submit the segment First time Prior Authorization, Prior Authorization Renewal for, SECTION DRUG REQUESTED, Drug name, Dose, Administration ex oral IV etc, Frequency, Duration, Medical condition, Will this drug be used according, Yes, Site of drug administration, Home, Doctor officeInfusion clinic, and Hospital outpatient.
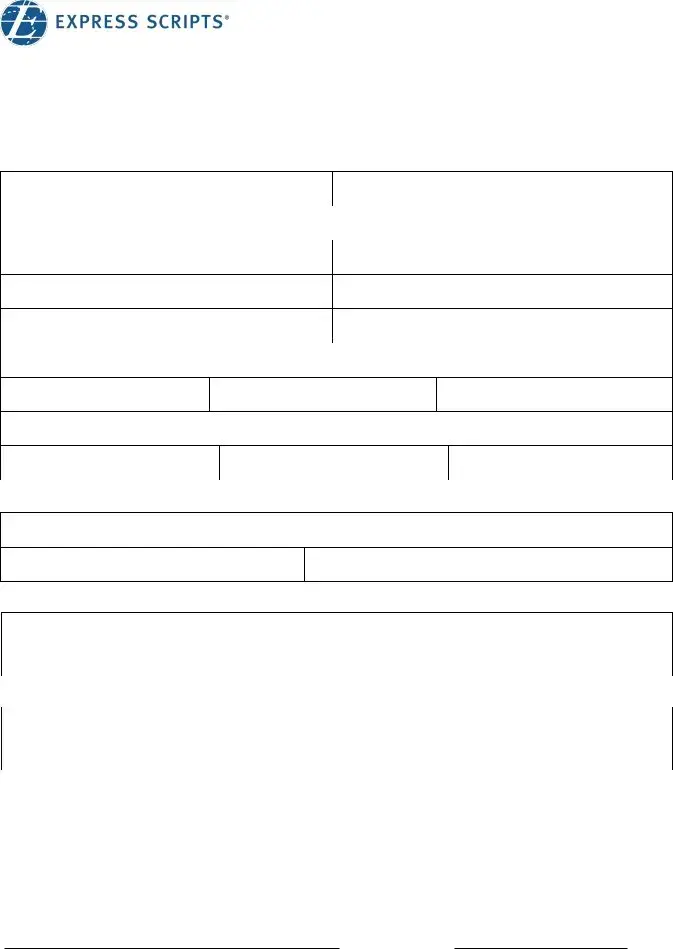
You will need to indicate the rights and responsibilities of each party in paragraph Any relevant information of the, Therapies, and Page.
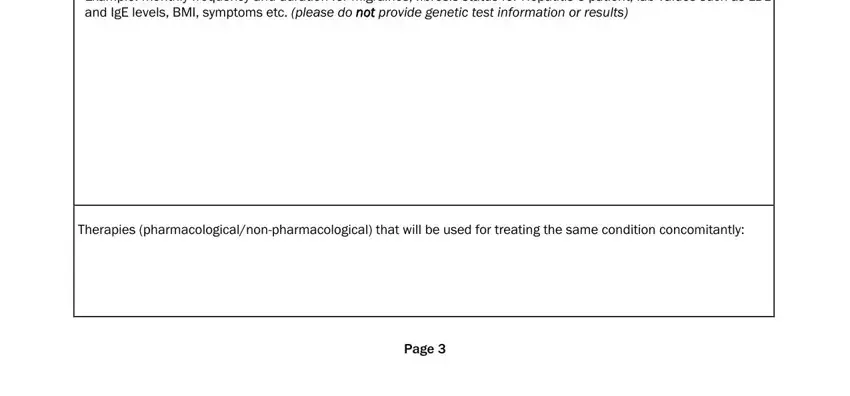
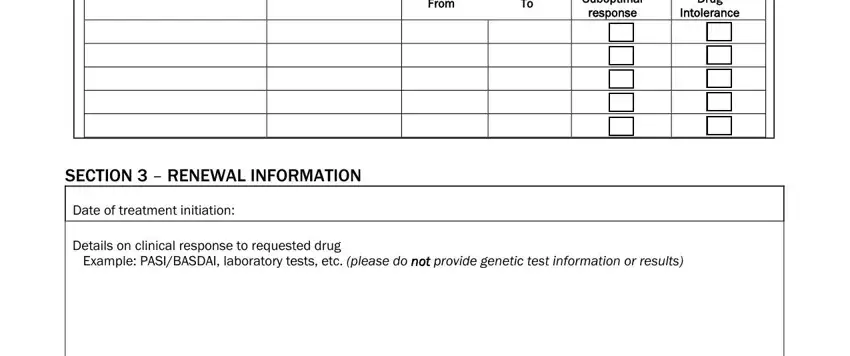
End up by analyzing the next fields and filling them in as required: From, Inadequate Suboptimal response, Allergy Drug Intolerance, SECTION RENEWAL INFORMATION, Date of treatment initiation, Details on clinical response to, and Example PASIBASDAI laboratory.
Step 3: After you select the Done button, your ready document can be transferred to any of your gadgets or to electronic mail indicated by you.
Step 4: In order to avoid potential future risks, it is important to have around two or three duplicates of any document.
 Drug name:
Drug name: Medical condition:
Medical condition: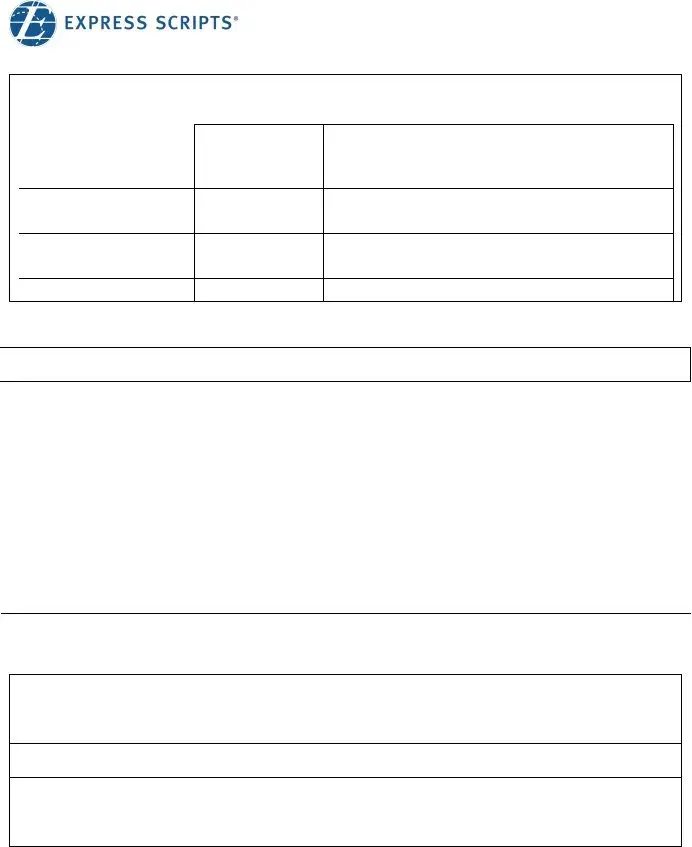
 Date of treatment initiation:
Date of treatment initiation: