The 114 Oklahoma form, officially designated for the Oklahoma Police Pension and Retirement System, serves as a comprehensive physical and medical examination document, crucial for assessing the health status of applicants. This thorough form requires detailed information from both the examinee and the examining physician, covering a broad spectrum of health aspects. These include a complete medical and surgical history, a wide array of physical exams from visual and audiometric testing to comprehensive metabolic profiles, and specifics like cholesterol levels and infectious disease markers. Additionally, the form mandates detailed reports on any knee examinations, if applicable, reinforcing its exhaustive nature. It also encompasses tests like TB skin tests, pulmonary function examinations, and even urine drug tests to align with NIDA Standards, ensuring a holistic evaluation of the applicant's health. The form is meticulously structured to elicit pertinent health information, including any history of diseases or injuries, alongside family medical history, thereby facilitating a robust assessment framework for eligibility determination within the system. Each section of the form, delineated across its pages, is designed to gather essential health data, making it a pivotal tool in the context of pension and retirement system processes in Oklahoma.
| Question | Answer |
|---|---|
| Form Name | Form 114 Oklahoma |
| Form Length | 8 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 2 min |
| Other names | HCV, OKLAHOMA, pension physical, GGTP |
Page 1
OKLAHOMA POLICE PENSION AND RETIREMENT SYSTEM
INSTRUCTION TO THE PHYSICIAN
The following History and Physical with Lab Data are required by each applicant:
1.Complete medical and surgical history with dates.
2.Complete physical exam.
3.Visual testing: With and without correction.
Binocular Vision Color Vision
4.Audiometric testing with decibel level.
5.Blood work: A. Comprehensive Metabolic Profile
B.Cholesterol
C.GGTP
D.Complete Blood Count
E.RPR
F.Hepatitis B Surface Antigen – HBSAG
G.Hepatitis B Core Antibody – HBCAB
H.Hepatitis C Antibody – HCV
I.Human Immunodeficiency Virus - HIV
6.Urinalysis with microscopic.
7.
8.T.B. Skin Test.
9.Pulmonary Function Test.
10.Exercise Tolerance Test (Bruce Protocol) with interpretation.
11.Complete knee examination form if history of knee surgery or significant injury.
12.Urine drug test must meet NIDA Standards.
SSN |
|
|
|
|
|
|
NAME |
|
|
|
|
|
DATE |
|
|
|
|||
SEX |
|
|
|
|
RACE |
|
|
|
AGE |
|
|
DATE OF BIRTH |
|
|
|
|
|||
ADDRESS |
|
|
|
|
|
|
PHONE ( |
) |
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
CITY,STATE,ZIP |
|
|
|
|
|
|
PHYSICIAN |
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
A. |
Have you ever: |
|
|
|
|
|
|
|
|
|
|
|
YES |
NO |
|||||
1.Received compensation for injury?
2.Received a disability pension?
3.Received medical discharge from armed forces?
4.Been rejected for military service for medical reasons?
5.Been hospitalized?
6.Been operated on?
7.Been rejected in any medical examination?
8.Had allergic reactions to drugs, medications, blood transfusions, insect bites? B. Have you ever had disease or injury to: (Circle affirmative items)
1.Head, ears, eyes, nose, throat?
2.Neck, back, hips, arms, legs, hands, feet?
3.Joints: shoulder, elbows, knees, wrist, ankles?
Form 114 4/08
Page 2
4.Heart: chest pain, palpitations, fainting, shortness of breath with exertion, sudden shortness of breath at night, feet swell, high blood pressure? History of Rheumatic fever or heart murmur, varicosities, deep leg pain (thrombophlebitis), heart attack, or stroke?
5.Lungs: Unusual shortness of breath, sputum production, coughed up blood, chest pain, wheezing, recurrent infections, history of asthma, history of smoking cigarette_____, pipe______, cigar______, other? How many per day?_____ For how many years?______
6.Breast: Pain, masses, nipple discharge? History of trauma, self breast exam and/or history of mammograms?
7.GI: Weight change, nausea or vomiting, vomiting blood, heart burn, abdominal pain, diarrhea or constipation of chronic or unusual character? History of ulcers, rectal bleeding, jaundice, laxative use/abuse?
8.GU: Pain when you urinate, blood colored urine, frequency or urgency to urinate? History of kidney stones, recurrent urinary tract infections, venereal diseases (syphilis, gonorrhea)?
9.Genital Tract:
Female: Age of Menses ______; # of days between periods ______; Date of last regular period ______;
History of severe pain during menstruation? Any history of unusual bleeding between periods? History of vaginal discharge? # of pregnancies ______; # of abortions or miscarriages ______; #
of deliveries ______; Types of contraceptive currently used ______________; date and result of last
pap smear?________________.
Male: Penile pain, discharge or skin lesions? Testicular pain or masses. History of prostate problems, hernias? History of vasectomy?
10.History of anemia, swollen and/or sore lymphnodes, easy or spontaneous bruising, excessive bleeding? History of any type of cancer?
11.History of retarded growth or development? Temperature intolerance, goiter, increased thirst, appetite, or frequency to urinate? History of diabetes, gout, recurrent skin rashes, unusual loss of hair?
12.History of tremor, paralysis, imbalance, muscle weakness or low sensitivity with the sense of touch? History of seizure disorder?
13.History of nervousness, anxiety, irritability? History of depression or suicide? History of psychiatric/psychological evaluation and/or treatment? History of drug or alcohol abuse?
14.History of Hepatitis B, Hepatitis C, HIV or AIDS?
C.Family medical history and any descriptive comments on positively answered question(s) should be completed below.
D.All affirmative answered responses to the health screen if significant or pertinent to current health status of the applicant should be identified and outlined as to the time of onset, duration, location, aggravating or alleviating symptoms and any associated symptoms that are characteristic of the problem.
I certify that the above health information is complete and true to the best of my knowledge. I authorize the medical examiner for the participating municipality to investigate any and all statements of health made herein.
Signature of Examinee |
Date |
Comments:
Form 114 4/08
Page 3
PHYSICAL EXAM AND LABORATORY ASSESSMENT FORM
Name: |
|
|
|
|
City: |
|
|
|
Date: |
|
|
Height: |
|
Weight: |
|
Pulse: |
|
Blood Pressure: |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
NormalComments
1)Integument
2)Heent
3)Breast
4)Chest
5)Heart
6)Abdomen
7)Genitalia
8)Rectal
9)Stool Guaiac Results
10)Musculoskeletal
11)Neurologic
Laboratory Results
1) |
Visual Acuity: |
Uncorrected |
R______/ L______ |
Binocular Vision |
|
|
Corrected |
R______/ L______ |
Color Vision |
2)Audiometric: (500) ___/___ (1000) ___/___ (2000) ___/___ (3000) ___/___ (4000) ___/___ (6000) ___/___
3) |
B)Lumbar Spine Series
(Obtain only if history of back problem)
4)Please submit copy of:
A. Comprehensive Metabolic Profile |
G. Hepatitis B Core Antibody - HBCAB |
B. Cholesterol |
H. Hepatitis C Antibody – HCV |
C. GGTP |
I. Human Immunodeficiency Virus – HIV |
D. Complete Blood Count |
J. Urinalysis |
E. RPR |
K. Drug Screen |
F. Hepatitis B Surface Antigen HBSAG
5)PPD Positive ( ) Negative ( )
Examiner’s Signature
Form 114 4/08
Page 4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
SPIROMETRY REPORT |
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
PHYSICIAN: |
|
|
|
|
|
|
|
|
|
|
|
|
TEST #: |
|||||
NAME: |
|
|
|
|
|
|
|
|
|
|
|
|
DATE: |
|
|
|
|
|
|
|
||||
AGE: |
|
|
|
HEIGHT: |
|
(cm) WEIGHT: |
(lbs) |
|
RACE: |
|
|
|
|
SEX: |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
DIAGNOSIS: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
ASTHMA |
|
|
|
TUBERCULOSIS |
|
|
|
|
|
|
|
|
HISTORY: |
|||||||
|
|
|
|
BRONCHITIS |
|
|
|
HYPERTENSION |
|
|
|
|
|
|
|
|
MORNING COUGH |
|||||||
|
|
|
|
EMPHYSEMA |
|
|
|
CHEST PAIN |
|
|
|
|
|
|
|
|
|
SPUTUM COLOR |
||||||
|
|
|
|
LUNG CANCER |
|
|
|
OTHER |
|
|
|
|
|
|
|
|
|
SPUTUM AMOUNT |
||||||
SMOKING: |
|
|
|
|
|
|
|
|
|
|
|
MEDICATION NOW TAKING: |
||||||||||||
A.Never used
B. |
Used to smoke, stopped |
|
years ago. |
|
||
C. |
Used to smoke |
|
pack/day for |
|
years. |
|
D.Continue to smoke.
E. Have smoked |
|
pack/day for |
|
years. |
F.Smoke only a pipe or cigar.
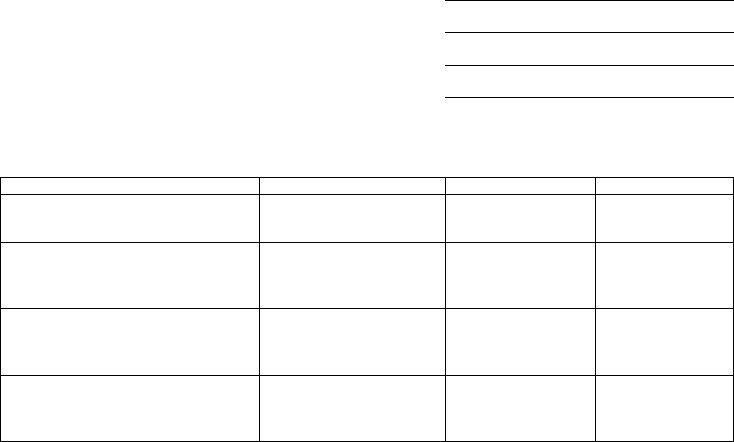
TEST |
PREDICTED |
ACTUAL |
% |
Forced Vital Capacity (FVC) (L)
Forced Expiratory Volume (FEV1) (L)
FEV1
FVC
Forced Expiratory Flow (FEF
INTERPRETATION:
Form 114 4/08
Page 5
NAME:
|
|
|
KNEE EXAMINATION |
||||
RANGE OF MOTION: |
|
|
|
|
|
|
|
Flexion: |
|
|
|
Extension: |
|
||
Crepitus with range of motion testing: |
Yes: |
|
|
|
No: |
||
DEFORMITIES: |
|
|
|
|
|
|
|
Swelling/Effusion:
With leg in full extension, circumference of thigh 7 cm and 20 cm proximal to superior pole of patella:
L:
R:
TESTS:
McMurray’s (medical meniscus):
Internal Rotation (lateral meniscus) with the foot internally rotated, movement from full flexion to extension:
Medial collateral ligament:
Lateral collateral ligament:
Anterior drawer (anterior cruciate ligament):
Patellar apprehension:
VMO on injured side compared to other:
Hop on each leg: |
|
|
|
Squat: |
||
Knee pain on rotation of hips and shoulders with feet together: |
||||||
Yes: |
|
|
No: |
|
|
|
Knee pain on rotation of hips and shoulders with feet crossed: |
||||||
Yes: |
|
|
No: |
|
|
|
Form 114 4/08
Page 6
INFORMED CONSENT FOR TREADMILL EXERCISE TEST OF PATIENTS
In order to evaluate the functional capacity of my heart, lungs, and blood vessels, I hereby consent, voluntarily, to perform an exercise test. I understand that I will be questioned and examined by a doctor, and have an electrocardiogram recorded to exclude any apparent contraindications to testing. Exercise will be performed by walking on a treadmill, with the speed and grade increasing every three minutes, until limits of fatigue, breathlessness, chest pain, and/or other symptoms occur to indicate that I have reached my limit. Blood pressure and electrocardiogram will be monitored during the test. The test may be stopped sooner than my own limit if the technician’s observations suggest that it may be unnecessary or unwise to continue.
The risks in performing this test are the risks of physical exercise and include irregular, slow and very rapid heart beats, large changes in blood pressure, fainting, and very rare instances of heart attack. Every effort will be made to minimize these by the preliminary examination and by observations during testing. Emergency equipment and trained personnel are available to deal with unusual situations as they arise.
The information obtained will be treated as confidential and will not be released to anyone without my express written consent. The information may, however, be used for statistical or scientific purpose with my right of privacy retained.
I have read the above, understand it, and all questions have been satisfactorily answered.
Patient’s Signature:
Witness:
Date:
Form 114 4/08
Page 7
EXERCISE TOLERANCE TESTING WORKSHEET
Name: |
|
|
|
|
|
|
|
|
|
|
|
Date: |
|
|
|
|
|||
Age: |
|
|
|
|
|
|
|
Sex: |
|
|
|
Height: |
|
|
Weight: |
|
|||
MPHR |
|
|
|
|
100% |
|
85% |
|
|
|
Medications: |
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
HR |
BP |
ST DEPRESSION |
OTHER EKG CHANGES |
SYMPTOMS |
|
|||||||||||
Sit |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Standing |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
Hypervent. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
Minutes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
STAGE 1 |
|
|
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1.7 MPH |
|
|
3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
10% GRADE |
|
|
4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
STAGE 2 |
|
|
5 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2.5 MPH |
E |
6 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
12% GRADE |
|
X |
7 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
STAGE 3 |
|
E |
8 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3.4 MPH |
|
R |
9 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
14% GRADE |
|
C |
10 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
STAGE 4 |
||
I |
11 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4.2 MPH |
||
S |
12 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
16% GRADE |
||
E |
13 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
STAGE 5 |
||
|
|
14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
5.0 MPH |
|
|
|
15 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
18% GRADE |
|
|
|
16 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
STAGE 6 |
|
|
|
17 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
5.5 MPH |
|
|
|
18 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
20% GRADE |
|
IMMED. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
R |
1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
E |
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
C |
3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
O |
4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
V |
5 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
E |
6 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
R |
7 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Y |
8 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TOTAL: |
|
|
LAST STAGE: |
|
TIME IN LAST STAGE: |
|
|
||||
|
|
MHR: |
|
% OF MHR: |
|
|
|||||
MAX. SYSTOLIC B.P.: |
|
|
ST: |
|
DOUBLE PRODUCT: |
|
|
||||
VO2: |
|
|
|
POST: |
|
|
RST: |
|
|||
FUNCTIONAL AEROBIC IMPAIRMENT: |
|
|
|
|
|
|
|
|
|
||
INTERPRETATION: |
|
|
|
|
|
|
|
|
|
||
Form 114 4/08

Page 8
AUTHORIZATION TO RELEASE MEDICAL/PSYCHIATRIC/PSYCHOLOGICAL INFORMATION
Patient’s Name
Date of Birth
Social Security Number
TO WHOM IT MAY CONCERN:
I hereby request and authorize any health plan, physician, health care professional, hospital, clinic, laboratory, pharmacy, medical facility, or other health care provider that has provided payment, treatment or services to me or on my behalf to furnish to the Oklahoma Police Pension and Retirement System , the Retirement Board, and/or the participating municipality to which I am seeking employment and any representative thereof (collectively, the “System”) any and all records, information and evidence in their possession regarding my injuries, medical history, physical condition, and psychiatric/psychological information, including information related to alcohol or drug abuse, both prior and subsequent to the date below until this authorization expires or until I revoke this authorization. Any or all of such health information is referred to in this authorization as my “protected health information” or “PHI.”
Upon presentation of this authorization, or an exact photocopy thereof, you are directed (1) to permit the personal review, copying or photostatting of such records, information and evidence by the System or (2) to provide copies of such records to the System.
I further understand that, if my PHI is transmitted or maintained electronically (my “electronic PHI”), you or any agent or subcontractor that creates, receives, maintains, or transmits my electronic PHI will implement administrative, physical, and technical safeguards that reasonably and appropriately protect the confidentiality, integrity, and availability of my electronic PHI, and you will ensure that any agent (including a subcontractor) to whom you provide my electronic PHI agrees to implement reasonable and appropriate security measures to protect my PHI.
THE INFORMATION AUTHORIZED FOR RELEASE MAY INCLUDE RECORDS WHICH MAY INDICATE THE PRESENCE OF A COMMUNICABLE OR NONCOMMUNICABLE DISEASE.
I hereby acknowledge that the information authorized for release may include information which may be considered information about a communicable or venereal disease, which may include, but is not limited to, a disease such as hepatitis, syphilis, gonorrhea or the human immunodeficiency virus, also known as Acquired Immune Deficiency Syndrome (AIDS).
I also acknowledge that the information that is used or disclosed pursuant to this authorization may be used or redisclosed by the System for purposes of eligibility and benefits determinations and, if presented at a Retirement Board meeting and/or hearing, the information may become part of a public record.
I understand that I may revoke this authorization at any time, in writing, except that revocation will not apply to information already used or disclosed in response to this authorization.
Unless revoked or otherwise indicated, this authorization will expire two years from date of signature.
I hereby release the System from any liability in connection with the release of information pursuant to this authorization.
Signature |
|
Date |
Form 114 4/08