When it comes to managing pharmacy reimbursement claims, the CF907527 form plays a crucial role. This form ensures individuals can claim reimbursement for pharmacy expenses efficiently and accurately. It requires detailed member and patient information, including identification numbers and addresses, to verify eligibility. The form also captures specific pharmacy information and prescription details, emphasizing the importance of accurate and complete documentation for successful reimbursement. It includes sections for compound prescriptions and purchases made outside the United States, addressing various scenarios that could affect reimbursement. The instructions highlight the necessity of attaching receipts and advise on the process for claims involving coordination of benefits, where another health plan has contributed to the payment. Importantly, the form contains warnings about the severe consequences of submitting false information, aiming to deter fraudulent claims and maintain the integrity of the reimbursement process. With sections designed to facilitate clear communication between members, pharmacies, and the reimbursement authority, the CF907527 form embodies a comprehensive approach to pharmacy claim reimbursement.
| Question | Answer |
|---|---|
| Form Name | Form Cf907527 |
| Form Length | 2 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 30 sec |
| Other names | Medco_Claim_For m_5_22_08_ID113 656 1199 pharmacy reimbursement form |
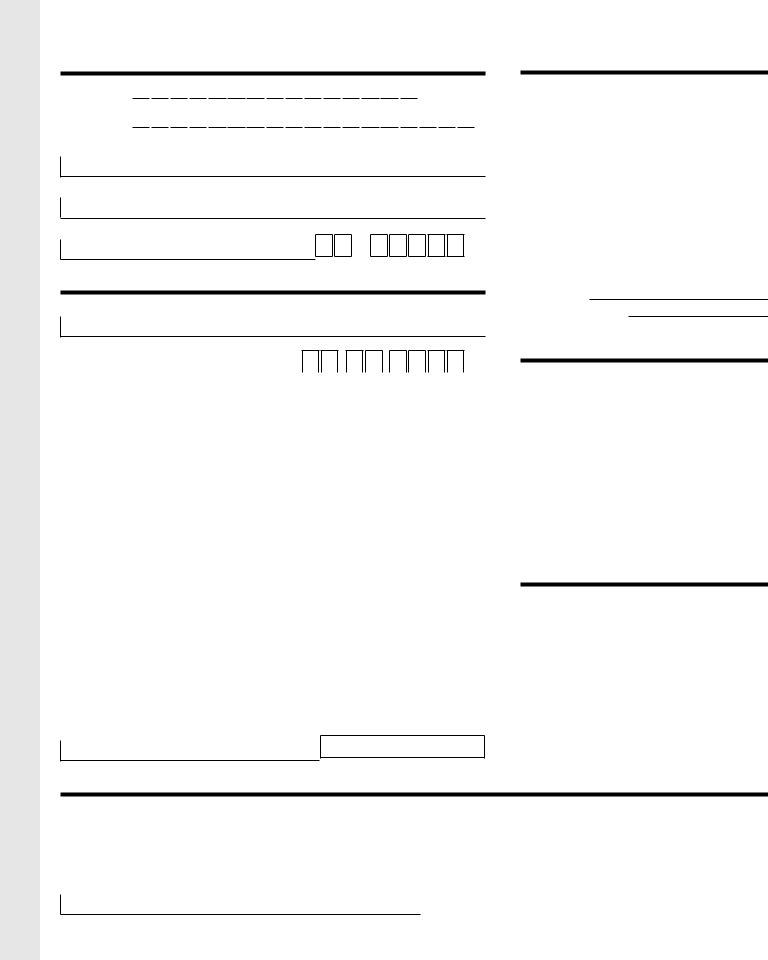
Pharmacy Reimbursement Claim Form
Please read the back for instructions. Complete all information.
An incomplete form may delay your reimbursement.
Member/Subscriber Information See your ID card.
RxGrp Member ID
Member Name (First, Last)
Street Address
City |
State |
Zip |
Patient Information
Patient Name (First, Last)
Patient Date of Birth (Month/Day/Year) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
Gender |
Relationship to Member/Subscriber |
|
|
|
|
|
|
|
|||||||||||||||||
Female |
1 |
Self |
5 |
Disabled Dependent |
|||||||||||||||||||||
Male |
2 |
Spouse |
6 |
Dependent Parent |
|||||||||||||||||||||
|
3 |
Eligible Child |
7 |
Nonspouse Partner |
|||||||||||||||||||||
|
4 |
Dependent Student |
8 |
Other |
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
Pharmacy Information |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Name of Pharmacy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Street Address |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
City |
|
|
|
|
|
|
|
State |
|
|
Zip |
||||||||||||||
Telephone (include area code) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Claim Receipts
(Please read Section A on back for details.)
Check the appropriate box if your receipts are for a:
Compound prescription
Make sure your pharmacist lists ALL the VALID 11 digit NDC numbers and ingredients and quantities on the receipt.
Medication purchased outside of the United States
Please indicate: Country Currency used
Allergy medication (if covered by your pharmacy plan)
Coordination of Benefits
(Another Health Plan has paid a portion) Is this a coordination of benefits claim? Yes No
If yes, please read Section B on back for details, and mark the appropriate box for your primary coverage method.
1 You are submitting an Explanation of Benefits (EOB) from another Health Plan or from Medicare
3 You are submitting a copay receipt
Any person who knowingly and with intent to defraud, injure, or deceive any insurance company, submits a claim or application containing any materially false, deceptive, incomplete or misleading information pertaining to such claim may be committing a fraudulent insurance act which is a crime and may subject such person to criminal or civil penalties, including fines and/or imprisonment, or denial of benefits.*
X
Signature of Pharmacist or Representative |
NCPDP#/NPI# (Pharmacy Account Number) |
(If required by your pharmacy plan) |
(11 Digit Number) |
Please tape receipts on the back.
Acknowledgment
I certify that the medication(s) described above was received for use by the patient listed above, and that I (or the patient, if not myself) am eligible for prescription drug benefits. I also certify that the medication received was not for an
X
Signature of Member/Subscriber
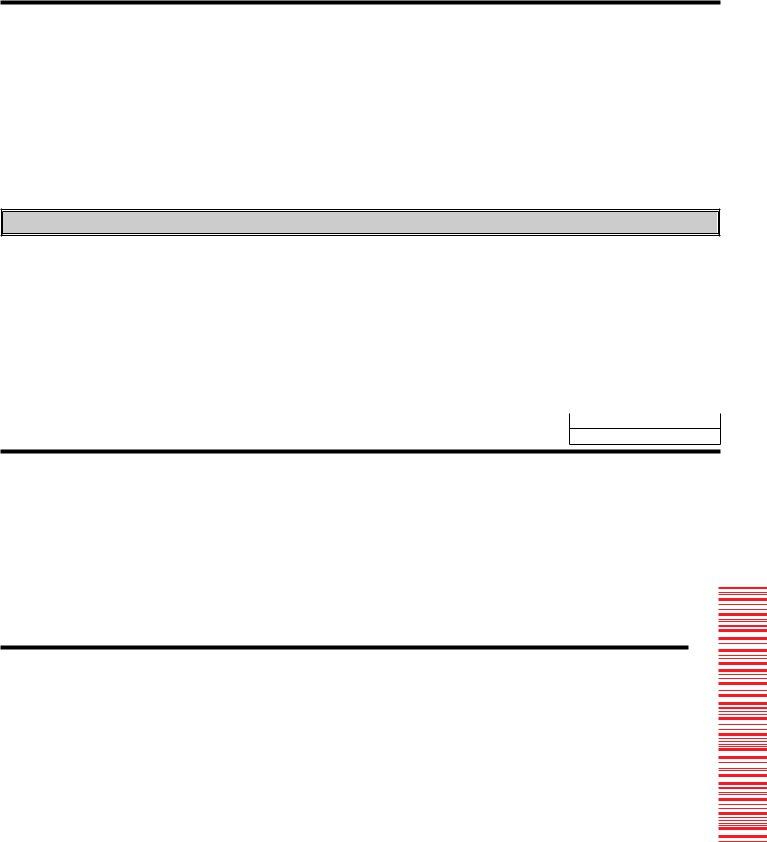
Instructions
Read carefully before completing this form
1.Be sure your receipts are complete. In order for your request to be processed, all receipts must contain the information listed below. Your pharmacist can provide the necessary information if your claim is not itemized.
2.The member/subscriber should read the acknowledgment carefully, then sign and date this form.
3.Return the completed form and receipt(s) to: Medco Health Solutions, Inc.
P.O. Box 14711
Lexington, KY 40512
Section A – Claim Receipts
Please tape your pharmacy receipts (not the cash register receipt) to this side of the claim form. Please do not staple.
Receipts must contain the following information.
• Date prescription filled |
• NDC number (drug number) |
• Prescription number (Rx number) |
• Name and address of pharmacy |
• Name of drug and strength |
• DAW (Dispense As Written) |
• Doctor name or ID number |
• Quantity and days’ supply |
• Amount paid |
TAPE YOUR PHARMACY RECEIPTS HERE
If you have additional receipts tape them to a separate piece of paper.
PHARMACY INFORMATION (For Compound Prescriptions ONLY)
•List the VALID 11 digit NDC number for EACH ingredient used for the compound prescription.
•For each NDC number, indicate the “metric quantity” expressed in the number of tablets, grams, milliliters, creams, ointments, injectables, etc.
•Indicate the TOTAL charge (dollar amount) paid by the patient.
•Receipt(s) must be attached to claim form.
RX# |
|
Date |
|
Days’ |
|
|
Filled |
|
Supply |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
VALID 11 digit NDC# |
Quantity |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Total Quantity
Total Charge
Section B – Coordination of Benefits
•You must complete a separate claim form for each pharmacy used and for each patient.
•You must submit claims within one year of date of purchase or as required by your plan.
You are submitting an Explanation of Benefits (EOB) from another Health Plan or from Medicare
If you have not already done so, submit the claim to the Primary Plan or Medicare. Once the EOB is received, complete this form, tape the original prescription receipts in the spaces provided above, and attach the EOB from the Primary Plan or Medicare, which clearly indicates the cost of the prescription and what was paid by the Primary Plan or Medicare.
You are submitting a copay receipt
If your Primary Plan is one in which a
* Arizona: For your protection, Arizona law requires the following statement to appear on this form. Any person who knowingly presents a false or fraudulent claim for payment or a loss is subject to criminal and civil penalties.
* California: For your protection, California law requires the following to appear on this form: Any person who knowingly presents false or fraudulent claim for the payment of a loss is guilty of a crime and may be subject to fines and confinement in state prison.
* Pennsylvania: Any person who knowingly and with intent to defraud any insurance company or other person, files an application for insurance or statement of claim containing any materially false information or conceals for the purpose of misleading, information concerning any fact material thereto, commits a fraudulent insurance act, which is a crime and subjects such person to criminal and civil penalties.
*CF907527*
*CF907527* |