Understanding the intricacies of the MO 886 4405 form is crucial for providers within the Missouri Department of Social Services' network. As a concise requisition document, it serves a specific yet pivotal role in the pharmacy administration sector of the Missouri HealthNet Division. Designed explicitly for instances where a previous claim has been denied, this form initiates a review process imperative for seeking reimbursement or resolution. It categorically states from the outset that it is not a standard pharmacy claim form, emphasizing its unique function in the administrative workflow. Providers are instructed to submit denied claim details, encapsulating essential information ranging from the provider's identifiers to the detailed medication prescribed, including the drug name, dosage, prescription number, and the rationale for the medication without prior override approval. In addition, it necessitates information on the contact person, the patient for whom the medication was prescribed, and specific dates that are critical to the review process. It is of utmost importance that all required fields are thoroughly completed to avoid processing delays. The document underscores the necessity of adhering to the specified communication channels — via phone or fax — to facilitate efficient handling. By laying out these prerequisites, the form acts as a streamlined conduit between healthcare providers and the MO HealthNet Division, ensuring that requests for backdating are managed with the precision and urgency they warrant.
| Question | Answer |
|---|---|
| Form Name | Form Mo 886 4405 |
| Form Length | 1 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 15 sec |
| Other names | NDC, DISPENSING, ADMIN, PROVIDER |
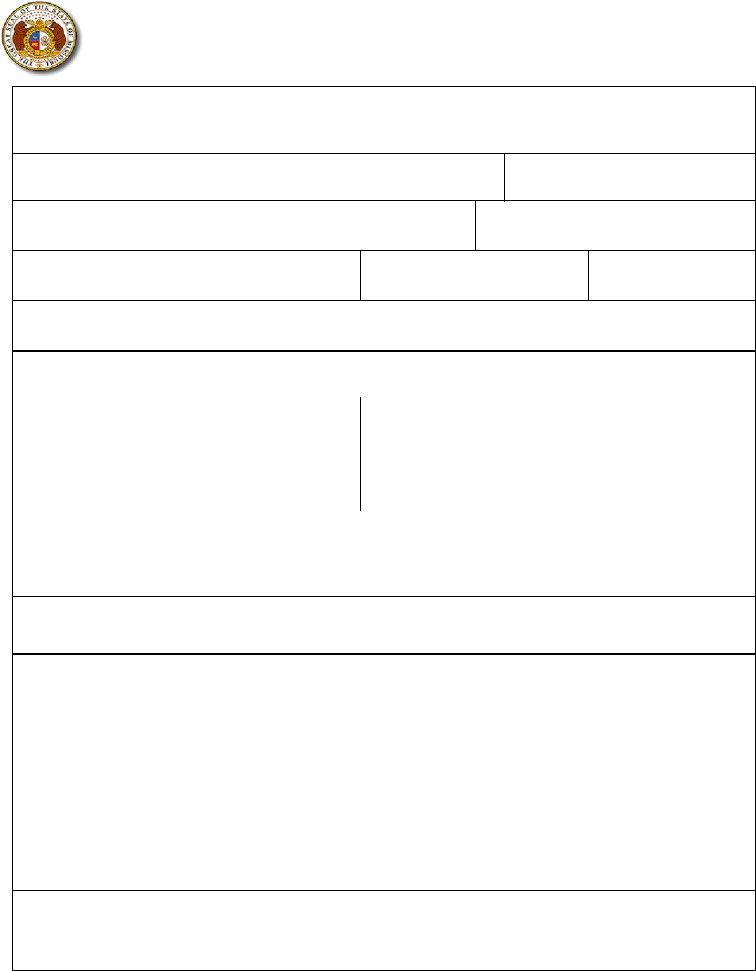
MISSOURI DEPARTMENT OF SOCIAL SERVICES |
RETURN TO: PHARMACY ADMIN |
MO HEALTHNET DIVISION |
MO HEALTHNET DIVISION |
|
PO BOX 6500 |
REQUEST FOR BACKDATE
JEFFERSON CITY, MO
***THIS IS NOT A PHARMACY CLAIM FORM. ***
THERE MUST BE A DENIED CLAIM SUBMITTED TO MO HEALTHNET FOR THE REVIEW PROCESS TO BEGIN. ALL REQUIRED INFORMATION MUST BE SUPPLIED OR THE REQUEST CANNOT BE PROCESSED.
PHONE:
PLEASE CHECK ONE
Initial Request Duplicate Request
CURRENT DATE
PROVIDER NAME
MO HEALTHNET PROVIDER IDENTIFIER OR NPI
CONTACT NAME
TELEPHONE NUMBER
FAX NUMBER
CONTACT MAILING ADDRESS (INCLUDING CITY, STATE, AND ZIP)
PARTICIPENT NAME |
DCN |
DATE OF BIRTH |
|
||
|
|
|
|
|
|
DATE OF SERVICE |
DRUG NAME/STRENGTH |
NDC |
PRESCRIPTION |
SUBMITTED CHARGE |
|
NUMBER |
|||||
|
|
|
|
||
|
|
|
|
|
|
DIAGNOSIS
PHYSICIAN DEA NO. OR MO HEALTHNET PROVIDER NO. OR NPI
NAME OF PRESCRIBING PHYSICIAN |
DATE DRUG WAS FIRST USED |
|
|
LIST ALL OTHER RELATED MEDICATIONS PREVIOUSLY TRIED INCLUDING LENGTH AND DATES OF EACH
DETAILED EXPLANATION FOR WHY THE OVERRIDE WAS NOT OBTAINED PRIOR TO DISPENSING THE THERAPY
RECIPIENT NAME |
|
|
DCN |
|
DATE OF BIRTH |
|
|
|
|
|
|
|
|
|
|
DATE OF SERVICE |
DRUG NAME/STRENGTH |
NDC |
|
PRESCRIPTION NUMBER |
|
SUBMITTED CHARGE |
|
|
|
|
|
|
|
|
|
DIAGNOSIS |
|
|
|
|
DATE DRUG WAS FIRST USED |
||
|
|
|
|
|
|||
NAME OF PRESCRIBING PHYSICIAN |
|
|
|
PRESCRIPTION DEA NO. OR MO |
|||
|
|
|
|
|
HEALTHNET PROVIDER NO. |
||
|
|
|
|
|
|
|
|
LIST ALL OTHER RELATED MEDICATIONS PREVIOUSLY TRIED INCLUDING LENGTH AND DATES OF EACH
DETAILED EXPLANATION FOR WHY THE OVERRIDE WAS NOT OBTAINED PRIOR TO DISPENSING THE THERAPY
MO