In the State of Illinois, ensuring the well-being and health of children in educational settings is of paramount importance, which is highlighted by the requirement of the Illinois Certificate of Child Health Examination. This comprehensive form, updated and mandated for use in DCFS licensed child care facilities, demands a thorough documentation of a child's immunizations, health history, and screenings for vision and hearing. It requires detailed records of vaccinations against a number of diseases, with space to note any medical contraindications and alternative proofs of immunity where applicable. Beyond immunizations, the form delves into the child's medical history, including allergies, medications, surgeries, and any diagnoses of chronic conditions like asthma or diabetes, as well as noting any developmental delays or physical disabilities. Vision and hearing screenings are integral parts of the examination, ensuring any issues that could affect the child's learning are identified early. Additionally, the form addresses the need for diabetes screening in certain at-risk populations and contains a lead risk questionnaire mandatory for young children in specific areas or circumstances. The exhaustive nature of this health examination form ensures that educators, healthcare providers, and guardians are all aligned in their understanding of a child's health needs and conditions, facilitating a supportive and safe educational environment.
| Question | Answer |
|---|---|
| Form Name | Illinois Child Health Examination Form |
| Form Length | 2 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 30 sec |
| Other names | certificate of child health examination, state of illinois certificate of child health examination 2021, illinois physical exam form, illinois physical exam |
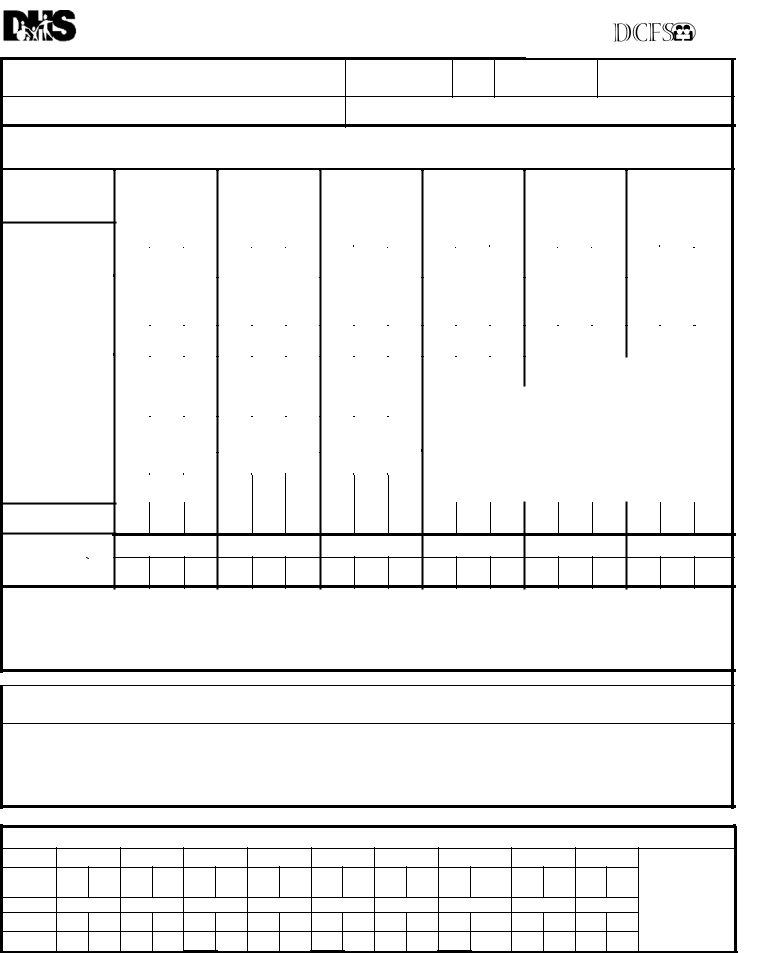
State of Illinois
Certificate of Child Health Examination
FOR USE IN DCFS LICENSED CHILD CARE FACILITIES
CFS 600
REV 2/2013
Student’s Name
Last |
First |
Middle |
Birth Date
Month/Day/Year
Sex Race/Ethnicity
School /Grade Level/ID#
Address |
Street |
City |
Zip Code |
Parent/Guardian |
Telephone # Home |
Work |
IMMUNIZATIONS: To be completed by health care provider. Note the mo/da/yr for every dose administered. The day and month is required if you cannot determine if the vaccine was given after the minimum interval or age. If a specific vaccine is medically contraindicated, a separate written statement must be attached explaining the medical reason for the contraindication.
Vaccine / Dose |
1 |
|
2 |
|
3 |
|
4 |
|
5 |
|
6 |
|
||||||||
MO DA YR |
MO DA YR |
MO DA YR |
MO DA YR |
MO DA YR |
MO DA YR |
|||||||||||||||
|
|
|||||||||||||||||||
DTP or DTaP |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Tdap; Td or Pediatric |
TdapTdDT |
TdapTdDT |
TdapTdDT |
TdapTdDT |
TdapTdDT |
TdapTdDT |
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
DT (Check specific type) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Polio (Check specific |
IPV OPV |
IPV OPV |
IPV OPV |
IPV OPV |
IPV OPV |
IPV OPV |
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
type) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hib Haemophilus |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
influenza type b |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hepatitis B (HB) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Varicella |
|
|
|
|
|
|
|
|
COMMENTS: |
|
|
|
|
|
|
|
|||
(Chickenpox) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MMR Combined |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Measles Mumps. Rubella |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Single Antigen |
Measles |
Rubella |
Mumps |
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Vaccines |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Pneumococcal
Conjugate
Other/Specify |
Meningococcal, |
Hepatitis A, HPV, |
Influenza |
Health care provider (MD, DO, APN, PA, school health professional, health official) verifying above immunization history must sign below. If adding dates
to the above immunization history section, put your initials by date(s) and sign here.)
Signature |
Title |
Date |
Signature |
Title |
Date |
ALTERNATIVE PROOF OF IMMUNITY
1.Clinical diagnosis is acceptable if verified by physician. *(All measles cases diagnosed on or after July 1, 2002, must be confirmed by laboratory evidence.)
*MEASLES (Rubeola) MO DA YR MUMPS MO DA YR VARICELLA MO DA YR Physician’s Signature
2. History of varicella (chickenpox) disease is acceptable if verified by health care provider, school health professional or health official.
Person signing below is verifying that the parent/guardian’s description of varicella disease history is indicative of past infection and is accepting such history as documentation of disease.
Date of Disease |
Signature |
|
Title |
|
Date |
|
|
|
|
|
|
3. Laboratory confirmation (check one) |
Measles |
Mumps |
Rubella |
Hepatitis B |
Varicella |
Lab Results |
Date |
MO DA YR |
|
|
(Attach copy of lab result) |
VISION AND HEARING SCREENING BY IDPH CERTIFIED SCREENING TECHNICIAN
Date
Age/
Grade
R |
L |
R |
L |
R |
L |
R |
L |
R |
L |
R |
L |
R |
L |
R |
L |
R |
L |
Vision
Hearing
Code:
P = Pass
F = Fail
U = Unable to test R = Referred G/C = Glasses/Contacts
(COMPLETE BOTH SIDES) |
Printed by Authority of the State of Illinois |
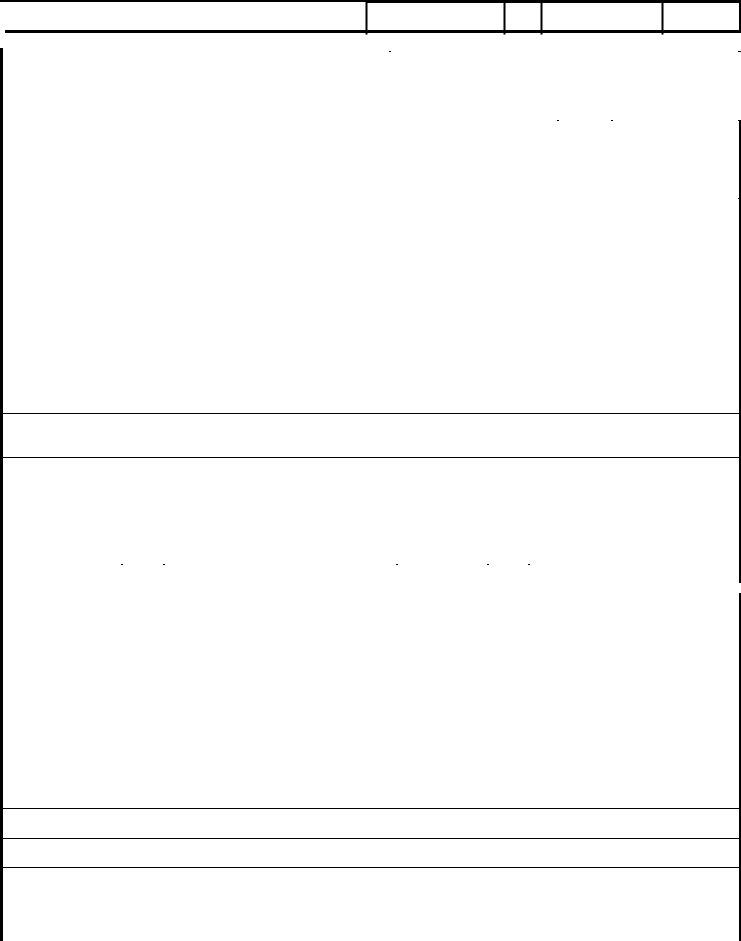
Last |
First |
Middle |
|
|
|
|
|
Birth Date
Month/Day/ Year
Sex School
Grade Level/ ID
|
HEALTH HISTORY |
TO BE COMPLETED AND SIGNED BY PARENT/GUARDIAN AND VERIFIED BY HEALTH CARE PROVIDER |
||||||||||
|
|
|
|
|
|
|
|
|
||||
|
ALLERGIES (Food, drug, insect, other) |
|
|
|
|
MEDICATION (List all prescribed or taken on a regular basis.) |
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Diagnosis of asthma? |
|
Yes |
No |
|
|
Loss of function of one of paired |
|
Yes |
No |
|
|
|
Child wakes during night coughing? |
Yes |
No |
|
|
organs? (eye/ear/kidney/testicle) |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Birth defects? |
|
Yes |
No |
|
|
Hospitalizations? |
|
Yes |
No |
|
|
|
|
|
|
|
|
|
When? What for? |
|
|
|
|
|
|
Developmental delay? |
|
Yes |
No |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Blood disorders? Hemophilia, |
|
Yes |
No |
|
|
Surgery? (List all.) |
|
Yes |
No |
|
|
|
Sickle Cell, Other? Explain. |
|
|
|
|
|
When? What for? |
|
|
|
|
|
|
Diabetes? |
|
Yes |
No |
|
|
Serious injury or illness? |
|
Yes |
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Head injury/Concussion/Passed out? |
Yes |
No |
|
|
TB skin test positive (past/present)? |
|
Yes* |
No |
*If yes, refer to local health |
||
|
|
|
|
|
|
|
|
|
|
|
department. |
|
|
Seizures? What are they like? |
|
Yes |
No |
|
|
TB disease (past or present)? |
|
Yes* |
No |
||
|
|
|
|
|
|
|
|
|
|
|
||
|
Heart problem/Shortness of breath? |
Yes |
No |
|
|
Tobacco use (type, frequency)? |
|
Yes |
No |
|
||
|
|
|
|
|
|
|
|
|
|
|
||
|
Heart murmur/High blood pressure? |
Yes |
No |
|
|
Alcohol/Drug use? |
|
Yes |
No |
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Dizziness or chest pain with |
|
Yes |
No |
|
|
Family history of sudden death |
|
Yes |
No |
|
|
|
exercise? |
|
|
|
|
|
before age 50? (Cause?) |
|
|
|
|
|
|
Eye/Vision problems? _____ |
Glasses Contacts Last exam by eye doctor ______ |
Dental |
Braces Bridge |
Plate |
Other |
||||||
|
Other concerns? (crossed eye, drooping lids, squinting, difficulty reading) |
|
|
|
|
|
|
|||||
|
Ear/Hearing problems? |
|
Yes |
No |
|
|
Information may be shared with appropriate personnel for health and educational purposes. |
|||||
|
|
|
|
|
|
|
Parent/Guardian |
|
|
|
|
|
|
Bone/Joint problem/injury/scoliosis? |
Yes |
No |
|
|
|
|
|
|
|||
|
|
|
Signature |
|
|
|
|
Date |
||||
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|||||
|
PHYSICAL EXAMINATION REQUIREMENTS |
Entire section below to be completed by MD/DO/APN/PA |
|
|
||||||||
|
HEAD CIRCUMFERENCE if < |
|
|
HEIGHT |
WEIGHT |
|
BMI |
|
B/P |
|||
|
|
|
|
|
||||||||
|
DIABETES SCREENING (NOT REQUIRED FOR DAY CARE) |
BMI>85% age/sex Yes |
No |
And any two of the following: Family History Yes No |
||||||||
Ethnic Minority Yes No Signs of Insulin Resistance (hypertension, dyslipidemia, polycystic ovarian syndrome, acanthosis nigricans) Yes No At Risk Yes No
LEAD RISK QUESTIONNAIRE Required for children age 6 months through 6 years enrolled in licensed or public school operated day care, preschool, nursery school and/or kindergarten. (Blood test required if resides in Chicago or high risk zip code.)
Questionnaire Administered ? Yes No Blood Test Indicated? Yes No |
Blood Test Date |
Result |
TB SKIN OR BLOOD TEST Recommended only for children in
in high prevalence countries or those exposed to adults in |
No test needed |
Test performed |
|
|
|||||||||
Skin Test: |
Date Read |
/ |
/ |
Result: Positive |
Negative |
mm ______________ |
|
|
|||||
Blood Test: |
Date Reported |
/ |
/ |
Result: Positive |
Negative |
Value ______________ |
|
|
|||||
LAB TESTS (Recommended) |
|
Date |
|
Results |
|
|
|
Date |
|
Results |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hemoglobin or Hematocrit |
|
|
|
|
|
Sickle Cell (when indicated) |
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Urinalysis |
|
|
|
|
|
|
|
Developmental Screening Tool |
|
|
|
||
SYSTEM REVIEW |
Normal |
|
|
Normal |
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Skin |
|
|
|
|
|
|
|
Endocrine |
|
|
|
|
|
Ears |
|
|
|
|
|
|
|
Gastrointestinal |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Eyes |
|
|
|
|
|
Amblyopia |
Yes No |
|
|
|
LMP |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Nose |
|
|
|
|
|
|
|
Neurological |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Throat |
|
|
|
|
|
|
|
Musculoskeletal |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Mouth/Dental |
|
|
|
|
|
|
|
Spinal Exam |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Cardiovascular/HTN |
|
|
|
|
|
|
Nutritional status |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Respiratory |
|
|
|
|
|
Diagnosis of Asthma |
Mental Health |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
Currently Prescribed Asthma Medication: |
|
|
|
|
|
|
|
|
|
||||
|
medication (e.g. Short Acting Beta Agonist) |
|
Other |
|
|
|
|
|
|||||
Controller medication (e.g. inhaled corticosteroid) |
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|||||||
NEEDS/MODIFICATIONS required in the school setting |
|
DIETARY Needs/Restrictions |
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SPECIAL INSTRUCTIONS/DEVICES e.g. safety glasses, glass eye, chest protector for arrhythmia, pacemaker, prosthetic device, dental bridge, false teeth, athletic support/cup
MENTAL HEALTH/OTHER Is there anything else the school should know about this student?
If you would like to discuss this student’s health with school or school health personnel, check title: Nurse Teacher Counselor Principal
EMERGENCY ACTION needed while at school due to child’s health condition (e.g. ,seizures, asthma, insect sting, food, peanut allergy, bleeding problem, diabetes, heart problem)? Yes No If yes, please describe.
On the basis of the examination on this day, I approve this child’s participation in |
|
(If No or Modified please attach explanation.) |
|
||
PHYSICAL EDUCATION |
Yes No Modified |
INTERSCHOLASTIC SPORTS |
Yes |
No Limited |
|
Print Name |
(MD,DO, APN, PA) |
Signature |
|
Date |
|
Address |
|
|
Phone |
|
|
|
|
|
|
|
|
(Complete Both Sides)