Navigating the landscape of healthcare billing in Massachusetts can often feel like moving through a maze, but understanding how to correctly submit a Subscriber Claim Form can turn complex paths into straight lines. This form is an essential tool for individuals who have received healthcare services from a provider that does not directly bill the local Blue Cross Blue Shield plan. To ensure efficient processing, claimants must adhere to several key instructions starting with submitting a claim for each patient separately. Alongside the form, an original, itemized bill which includes specific required information – such as provider's name, address, Tax ID/NPI, and credentials – is indispensable. The form also emphasizes the importance of retaining copies of all submitted bills and claim forms, as originals will not be returned. Further, to complete the submission, claimants must sign and date the form, then mail it alongside all necessary attachments to a designated address. Integration of patient and subscriber information, inclusive of identification numbers, addresses, and relevant insurance details, lays the foundation for the precise processing of these submissions. Additionally, the document outlines scenarios requiring further information like accidents or having other insurance coverage, thereby providing a comprehensive blueprint for members to navigate their claims. With a promised processing time of up to 30 days, this form represents a critical step for individuals seeking reimbursement or coverage for healthcare services not billed directly to BCBSMA, highlighting Blue Cross Blue Shield of Massachusetts' commitment to a streamlined, member-focused healthcare experience.
| Question | Answer |
|---|---|
| Form Name | Massachusetts Claim Form |
| Form Length | 2 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 30 sec |
| Other names | subscriber claim, blue cross shield massachusetts form, massachusetts ma claim, blue cross shield claim |
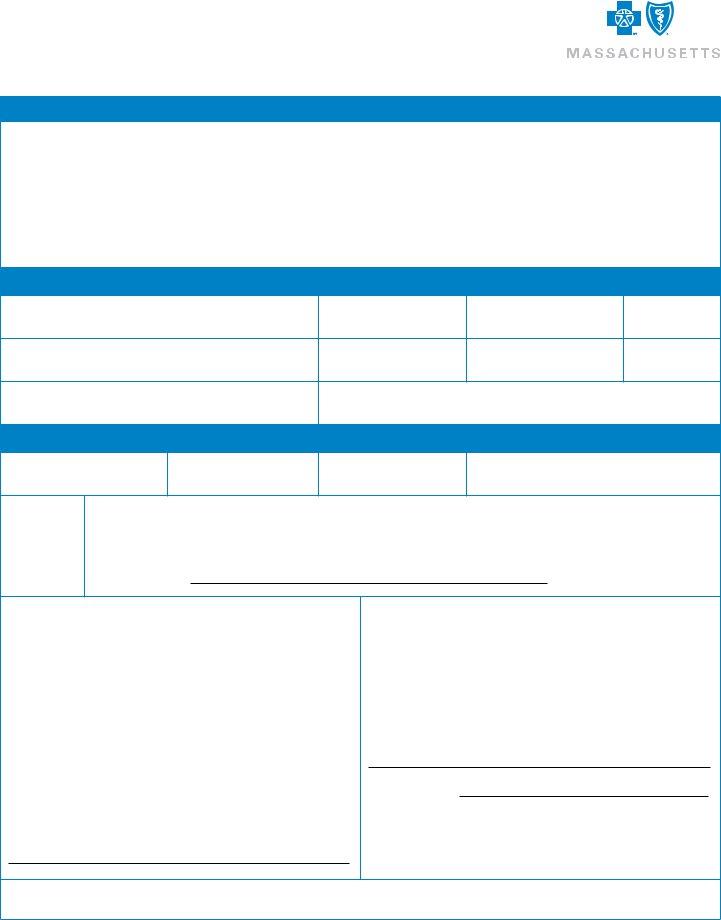
SUBSCRIBER CLAIM FORM
Instructions for Submitting Claims
1.Submit a claim only when you are billed for services from a provider that does not directly submit a claim to the local Blue Cross Blue Shield plan.
2.Submit a separate form for each patient.
3.Attach an original itemized bill from your provider (required information & example on the back)
4.Keep a copy of all bills and claim forms submitted (originals will not be returned)
5.Be sure to sign and date the completed form.
6.Mail claim form and all attachments to BCBSMA, P.O. Box 986030, Boston, MA 02298
Subscriber Information
Identification Number (including alpha prefix)
Last Name
First Name
Middle Initial
City
State
Zip Code
Date of Birth (MM/DD/YY)
Employer’s Name
Patient Information
Patient Last Name
First Name
Middle Initial
Date of Birth (MM/DD/YY)
Gender:
qMale
qFemale
Patient is:
q Subscriber (contract holder) q Student (age 19 or older) q Other (specify)
q Spouse (to contract holder)q Child (age 18 or younger) q Handicapped Dependent (age 19 or older)
Does the patient have other insurance: q Yes q No
|
|
Effective Date: |
|
Medicare Part A (Hospital) |
q Yes q No ____/____/_____ |
||
Medicare Part B (Medical) |
q Yes q No ____/____/_____ |
||
Medicare Part D (Pharmacy) |
q Yes q No ____/____/_____ |
||
Other Blue Cross |
|
|
|
Blue Shield Membership? |
q Yes q No ____/____/_____ |
||
Other Insurance Plan? |
q Yes q No ____/____/_____ |
||
Identification Number: |
|
|
|
Name and address of other insurance:
Was treatment for:
Accident at work? q Yes q No
Date of accident ____/____/_____
Auto accident? q Yes q No
Date of accident ____/____/_____
If yes, name of auto insurance:
Policy Number:
Other accident? q Yes q No
Date of accident ____/____/_____
Subscriber Signature: |
Date: |
Please allow up to 30 days for your claim to process.
Blue Cross Blue Shield of Massachusetts is an Independent Licensee of the Blue Cross and Blue Shield Association.
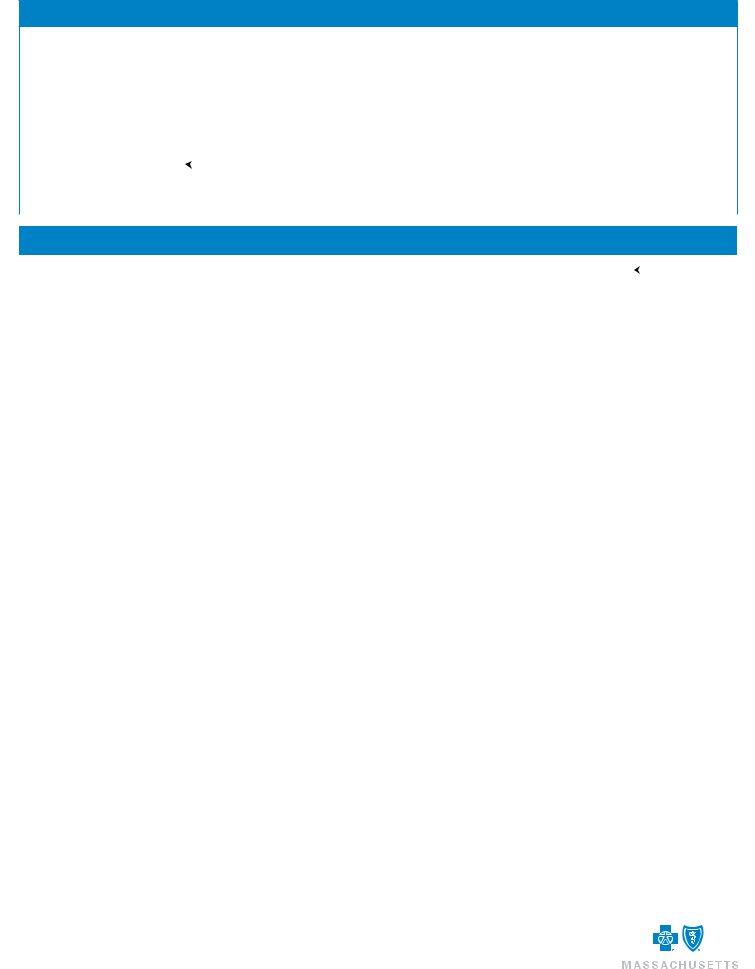
Example of a Complete Itemized Bill
|
Smith Speech Center |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
123 Main St. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Boston, MA 12345 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
To: Joe Smith |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
Patient Name: Joan Smith |
|
|
|
|
|||||||||
|
15 Elm St. |
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
Referring Doctor: Dr. John Jones |
|
|
|
||||||||||
|
Anytown, MA 12345 |
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Provider |
|
|
|
|
|
|
|
|
|||||
|
Jane Johnson, |
SLP, CCC |
|
|
|
Tax ID/NPI: |
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
Credentials |
|
|
|
|
|
|
|
|
|
|||||||||
|
License # Y777777 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
Procedure Code(s) |
|
|
|
Units |
|
Procedure Description |
|
|
Date of Service |
|
Amount |
|
|
|||||||
92507 |
|
|
|
|
|
1 |
|
|
10/5/2008 |
|
|
|
$72.50 |
|
Itemized |
||||||
|
|
|
|
|
|
|
|
|
|
|
Charges |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
92507 |
|
|
|
|
|
2 |
|
|
11/3/2008 |
|
|
|
$145.00 |
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
Diagnosis Codes: 784.50, 315.31 |
|
|
|
|
|
|
|
|
Total: $290.00 |
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Payments: $290.00 |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Balance Due: $0.00 |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Please note that your bill does not need to look exactly like the example above, but MUST contain the following required information:
1.A letterhead from the provider that MUST include all of the following:
–Provider name
–Provider address
–Provider Tax ID/NPI
–Provider credentials, i.e., the initials associated with the educational degrees the provider has earned. Examples include: MD, LICSW, DC, PT, OT, ST
2.Patient’s name
3.Date(s) of service
4.Itemized charges for each date of service and type of service received
5.Procedure codes (HCPCS/Revenue codes) for all services received
6.Diagnosis code(s) for services received
7.Number of
8.Attach any related claim summaries or Explanation of Medicare Benefit Forms you may have received for these services, including those received from other insurance companies.
9.When submitting a claim for PRESCRIPTION DRUGS, you must submit an itemized receipt from your pharmacy that includes:
–National Drug Code (NDC)
–Name of drug
–Date dispensed
–Quantity dispensed
–Name of prescribing physician
To view processed claims, visit our website http://www.bluecrossma.com/wps/portal/members/. If you have not already registered for Member Central, click Create an Account and follow the directions.
®Registered Marks of the Blue Cross and Blue Shield Association. © 2010 Blue Cross and Blue Shield of Massachusetts, Inc., and Blue Cross and Blue Shield of Massachusetts HMO Blue, Inc.
#101300 |
(10/10) PDF |