Navigating the complexity of healthcare and support services requires accurate and detailed assessment forms to ensure that individuals receive the care and support they need. Among these essential tools in Massachusetts is the Minimum Data Set – Home Care (MDS-HC), introduced in a significant overhaul by the Executive Office of Health and Human Services, Division of Medical Assistance. As of February 2003, chronic disease and rehabilitation hospitals have been mandated to transition to this form and the accompanying Request for Services (RFS-1), moving away from the previous Long Term Care Assessment form. This shift aims to streamline the referral process for long-term care services, encompassing nursing-facility and adult-day-health services among others. The MDS-HC form must be completed meticulously by an assessment coordinator, a role designated to a registered nurse to guarantee the form’s accuracy and completeness, although certain sections can also be filled out by a licensed social worker. The assessment’s breadth covers various essential aspects of a patient’s care needs, from cognitive and communication patterns to social functioning and informal support services, underlining the importance of a comprehensive approach to patient care planning and implementation. The inclusion of meticulous documentation on the patient’s condition, coupled with ICD-9-CM codes for diagnoses, lays a robust foundation for determining clinical eligibility for MassHealth's long-term-care services. Furthermore, the directive for chronic disease and rehabilitation hospitals to adhere to the updated documentation requirements by February 1, 2003, emphasizes the state’s commitment to enhancing communication lines between providers and the Division, thereby facilitating a smoother and more efficient process in addressing the long-term care needs of Massachusetts’ residents.
| Question | Answer |
|---|---|
| Form Name | Mds Hc Form |
| Form Length | 9 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 2 min 15 sec |
| Other names | mds hc manual, mds hc edit, mds hc form, mds hc rfs template |
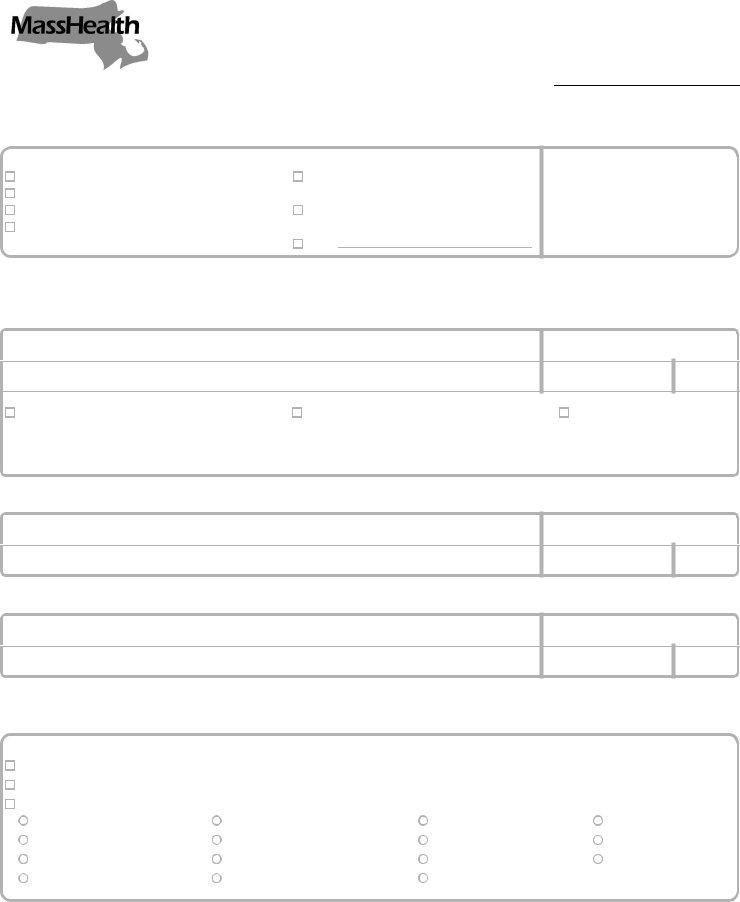
COMMONWEALTH OF MASSACHUSETTS
EXECUTIVE OFFICE OF HEALTH AND HUMAN SERVICES
DIVISION OF MEDICAL ASSISTANCE
600 Washington Street Boston, MA 02111 www.mass.gov/dma
MassHealth
Chronic Disease and
Rehabilitation Hospital Bulletin 83
January 2003
TO: Chronic Disease and Rehabilitation Hospitals Participating in MassHealth
FROM: Wendy E. Warring, Commissioner
RE: |
Changes in Clinical Assessment Forms |
|
|
|
|
Background |
The Division determines clinical eligibility for MassHealth |
|
|
services based upon documentation submitted by the provider. The Long |
|
|
Term Care Assessment form has been replaced by two new forms in |
|
|
order to facilitate communication between providers and the Division. |
|
|
|
|
New Forms |
Attached to this bulletin are copies of the two new forms required for |
|
|
approving referrals for |
|
|
to, |
|
|
• Request for Services |
|
|
Long Term Care Assessment form) |
|
|
• Minimum Data Set – Home Care |
|
|
Chronic disease and rehabilitation hospitals must begin using these new |
|
|
forms by February 1, 2003. Please discard all previous versions of the Long |
|
|
Term Care Assessment form. |
|
|
|
|
Who May Complete |
The |
|
the |
assessment coordinator must be a registered nurse who certifies the |
|
|
accuracy and completeness of the |
|
|
The following sections of the |
|
|
social worker (LSW, LCSW, or LICSW). |
|
|
AA – Name and Identification Numbers |
|
|
BB – Personal Items |
|
|
CC – Referral Items |
|
|
B – Cognitive Patterns |
|
|
C – Communication/Hearing Patterns |
|
|
E – Mood and Behavior Patterns |
|
|
F – Social Functioning |
|
|
G – Informal Support Services |
|
|
O – Environmental Assessment |
|
|
|
|
|
CONTINUED ON BACK |
|

MassHealth
Chronic Disease and
Rehabilitation Hospital Bulletin 83
January 2003
Page 2
Who May Complete |
Each person who completes a portion of the |
the |
certify the sections he or she completes in Section R – Assessment |
(cont.) |
Information (Other Signatures, Title, Sections, Date). |
|
|
Qualifications for |
The registered nurse or social worker must be licensed by the |
Completing the Forms |
Massachusetts Board of Registration. |
|
|
The |
|
|
medical diagnoses. |
|
|
Trainings |
The Division holds periodic trainings for providers. You will receive notice |
|
of trainings when they are scheduled. |
|
|
Supplies of the Forms |
You may photocopy the forms as needed. To obtain supplies of the |
|
forms, use the information below to mail or fax your request. Include your |
|
provider number, address, telephone number, the exact title of the form, |
|
and the desired quantity. |
|
MassHealth Forms Distribution |
|
P.O. Box 9101 |
|
Somerville, MA 02145 |
|
Fax: |
|
|
Questions |
If you have any questions about this bulletin, please contact MassHealth |
|
Provider Services at |
|
|
|
|
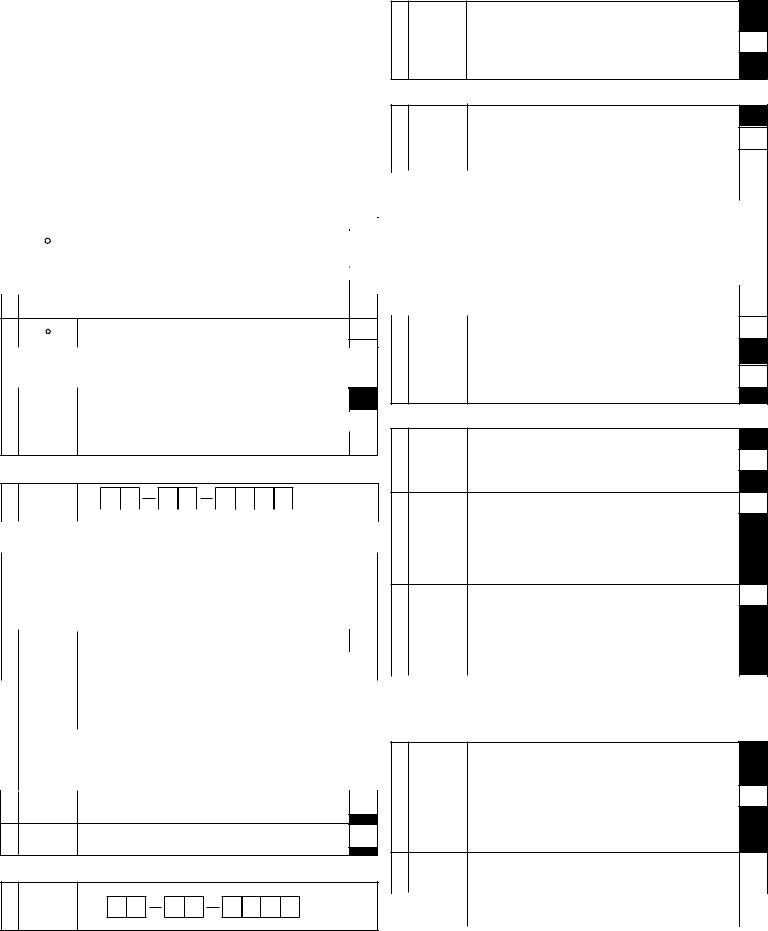
MINIMUM DATA SET - HOME CARE
•Unless otherwise noted, score for last 3 days
•Examples of exceptions include IADLs/Continence/Services/Treatments where status scored over last 7 days
SECTION AA. NAME AND IDENTIFICATION NUMBERS
1. |
NAME OF |
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
CLIENT |
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
a. (Last/Family Name) |
|
|
|
b. (First Name) |
|
c. (Middle Initial) |
|||||||||||||
2. |
CASE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
RECORD |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NO. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
3. |
GOVERN- |
a. Pension (Social Security) Number |
|
|
|
||||||||||||||||
|
MENT |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PENSION |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
AND HEALTH |
b. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Health |
insurance |
|
number |
(or |
other comparable insurance number) |
||||||||||||||
|
INSURANCE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
NUMBERS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SECTION BB. PERSONAL ITEMS (Complete at Intake Only)
1. |
GENDER |
1. Male |
2. Female |
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2. |
BIRTHDATE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Month |
Day |
|
Year |
|
|
|
|||||||||||
3. |
RACE/ |
(Check all that apply) |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
ETHNICITY |
RACE |
|
|
|
|
|
|
Native Hawaiian or other Pacific |
|
||||||||||
|
* |
|
|
|
|
|
|
|
||||||||||||
|
American Indian/Alaskan |
|
|
|
|
Islander |
|
|
d. |
|||||||||||
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
White |
|
|
|
||||||||||||||
|
|
Native |
|
|
a. |
|
|
e. |
||||||||||||
|
|
Asian |
|
|
b. |
ETHNICITY: |
|
|
|
|||||||||||
|
|
Black or African American |
c. |
Hispanic or Latino |
f. |
|||||||||||||||
4. |
MARITAL |
1. Never married |
3. Widowed |
5. Divorced |
|
|||||||||||||||
|
STATUS |
2. Married |
4. Separated |
6. Other |
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
5.LANGUAGE Primary Language
* |
0. English |
1. Spanish |
2. French |
3. Other |
|
|
|
|
|
||||
6. |
EDUCATION |
1. No schooling |
|
5. Technical or trade school |
|
|
|
(Highest |
2. 8th grade/less |
|
6. Some college |
|
|
|
Level |
3. |
|
7. Bachelor's degree |
|
|
|
Completed) |
4. High school |
|
8. Graduate degree |
|
|
7.RESPONSI- (Code for responsibility/advanced directives)
BILITY/ |
0. No |
1. Yes |
|
ADVANCED |
|
|
|
DIRECTIVES a. Client has a legal guardian |
|
||
|
|
|
|
b. Client has advanced medical directives in place (for example, a do not hospitalize order)
SECTION CC. REFERRAL ITEMS (Complete at Intake Only)
1.DATE CASE
OPENED/
|
REOPENED |
|
|
|
|
|
|
|
|
|
|
|
|
Month |
|
Day |
|
|
Year |
||||
|
|
|
|
|
|
||||||
2. |
REASON |
1. Post hospital care |
|
|
4. Eligibility for home care |
|
|||||
|
FOR |
2. Community chronic care |
|
|
5. Day care |
|
|||||
|
REFERRAL |
3. Home placement screen |
|
|
6. Other |
|
|||||
3. |
GOALS OF |
(Code for client/family understanding of goals of care) |
|
||||||||
|
CARE |
0. No |
1. Yes |
|
|
|
|
|
|||
|
|
a. Skilled nursing treatments |
|
|
d. Client/family education |
|
|||||
|
|
b. Monitoring to avoid clinical |
|
|
e. Family respite |
|
|||||
|
|
|
|
|
|||||||
|
|
|
|
|
|||||||
|
|
complications |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|||
|
|
c. Rehabilitation |
|
|
|
|
f. Palliative care |
|
|||
|
|
|
|
|
|
|
|||||
4.TIME SINCE Time since discharge from last
LAST recent instance in LAST 180 DAYS)
HOSPITAL |
0. No hospitalization within 180 days |
3. Within 15 to 30 days |
|
|
STAY |
1. Within last week |
4. More than 30 days ago |
|
|
|
2. Within 8 to 14 days |
|
|
|
|
|
|
|
|
5. WHERE |
1. Private home/apt. with no home care services |
|
|
|
LIVED AT |
2. Private home/apt. with home care services |
|
|
|
TIME OF |
3. Board and care/assisted living/group home |
|
|
|
REFERRAL |
4. Nursing home |
|
|
|
|
5. Other |
|
|
|
6. WHO LIVED |
1. Lived alone |
|
|
|
WITH AT |
2. Lived with spouse only |
|
|
|
REFERRAL |
3. Lived with spouse and other(s) |
|
|
|
|
4. Lived with child (not spouse) |
|
|
|
|
5. Lived with other(s) (not spouse or children) |
|
|
|
|
6. Lived in group setting with |
|
|
|
|
|
|
|
|
7.PRIOR NH Resided in a nursing home at anytime during 5 YEARS prior to case
PLACEMENT opening |
|
0. No |
1. Yes |
8.RESIDENTIAL Moved to current residence within last two years
HISTORY
0. No |
1. Yes |
SECTION A. ASSESSMENT INFORMATION
1.ASSESSMENT Date of assessment
REFERENCE
DATE
Month |
Day |
Year |
2.REASONS Type of assessment
FOR 1. Initial assessment
ASSESS- 2.
MENT 3. Routine assessment at fixed intervals
4.Review within
5.Review at return from hospital
6.Change in status
7.Other
SECTION B. COGNITIVE PATTERNS
1.MEMORY (Code for recall of what was learned or known)
RECALL |
0. Memory OK |
1. Memory problem |
ABILITY |
a. |
|
|
||
|
b. Procedural memory |
|
|
multitask sequence without cues for initiation |
|
2. |
COGNITIVE |
a. How well client made decisions about organizing the day (e.g., when |
|||
|
SKILLS FOR |
to get up or have meals, which clothes to wear or activities to do) |
|||
|
DAILY |
0. |
|
||
|
DECISION- |
|
|||
|
MAKING |
1. |
MODIFIED |
|
|
|
|
|
only |
|
|
|
|
2. |
MINIMALLY |
|
|
|
|
|
poor or unsafe and cues/supervision necessary at those times |
|
|
|
|
3. |
MODERATELY |
|
|
|
|
|
safe, cues/supervision required at all times |
|
|
|
|
4. |
SEVERELY |
|
|
|
|
|
|
||
|
|
b. Worsening of decision making as compared to status of 90 DAYS |
|||
|
|
AGO (or since last assessment if less than 90 days) |
|||
|
|
0. No |
1. Yes |
||
3.INDICATORS a. Sudden or new onset/change in mental function over LAST 7 DAYS
OF DELIRIUM (including ability to pay attention, awareness of surroundings, being |
|
coherent, unpredictable variation over course of day) |
|
0. No |
1. Yes |
b. In the LAST 90 DAYS (or since last assessment if less than 90 |
|
days), client has become agitated or disoriented such that his or |
|
her safety is endangered or client requires protection by others |
|
0. No |
1. Yes |
SECTION C. COMMUNICATION/HEARING PATTERNS
1. HEARING
0.HEARS
1.MINIMAL
2.HEARS IN SPECIAL SITUATIONS
3.HIGHLY IMPAIRED
2.MAKING (Expressing information
SELF |
0. |
UNDERSTOOD |
|
|
1. USUALLY |
(Expression) |
BUT if given time, little or no prompting required |
2. OFTEN |
|
|
prompting usuallly required |
|
3. SOMETIMES |
|
requests |
|
4. RARELY/NEVERUNDERSTOOD |
3.ABILITY TO (Understands verbal
UNDER- |
0. |
|
STAND |
||
1. USUALLY |
||
OTHERS |
||
BUT comprehends most conversation with little or no prompting |
||
|
||
(Comprehen- |
2. OFTEN |
|
sion) |
prompting can often comprehend conversation |
|
3. SOMETIMES |
||
|
||
|
rect communication |
|
|
4. RARELY/NEVERUNDERSTANDS |
4. |
COMMUNICA- |
Worsening in communication (making self understood or understand- |
|
|
|
TION |
ing others) as compared to status of 90 DAYS AGO (or since last |
|
|
|
DECLINE |
assessment if less than 90 days) |
|
|
|
|
|||
|
|
0. No |
1. Yes |
|
SECTION D. VISION PATTERNS
1.VISION (Ability to see in adequate light and with glasses if used)
0.
1.
2.MODERATELY
3.HIGHLY
4.SEVERELY
2.VISUAL Saw halos or rings around lights, curtains over eyes, or flashes of LIMITATION/ lights
|
DIFFICUL- |
0. No |
1. Yes |
|
|
|
|
||||
|
TIES |
|
|
|
|
3. |
VISION |
Worsening of vision as compared to status of 90 DAYS AGO (or since |
|||
|
DECLINE |
last assessment if less than 90 days) |
|
|
|
|
|
0. No |
1. Yes |
|
|
|
|||||
SECTION E. MOOD AND BEHAVIOR PATTERNS
1. INDICATORS OF
DEPRES-
SION,
ANXIETY,
(Code for observed indicators irrespective of the assumed cause)
0.Indicator not exhibited in last 3 days
1.Exhibited
2.Exhibited on each of last 3 days
1. TWO KEY |
|
|
|
(A) |
(B) |
INFORMAL |
|
|
|
PrIm |
Secn |
HELPERS |
If needed, willingness (with ability) to increase help: |
|
|
||
|
|
|
|||
Primary (A) |
0. More than 2 hours 1. |
2. No |
|
|
|
|
|
|
|
|
|
SAD MOOD
a. A FEELING OF SADNESS OR BEING DEPRESSED, that life is not worth living, that nothing matters, that he or she is of no use to anyone or would rather be dead
b.PERSISTENTANGER WITH SELF OR OTHERS— e.g., easily annoyed, anger at care received
c.EXPRESSIONS OF WHAT APPEARTO BE UNREAL- ISTIC
d.REPETITIVEHEALTHCOM-
e.REPETITIVEANXIOUSCOM-
f.SAD,PAINED,WORRIED FA- CIAL EXPRESSIONS — e.g.,
furrowed brows
g.RECURRENTCRYING,TEAR- FULNESS
h.WITHDRAWALFROMACTIVI- TIES OF
i . REDUCED SOCIAL INTER-
ACTION
|
and |
j . — Advice or emotional support |
|
|
|
|
|
Secondary (B) |
|
|
|
|
|
|
k. — IADL care |
|
|
|
||
|
|
|
|
|
||
|
(cont) |
|
|
|
|
|
|
l. — ADL care |
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
|
|
2. |
CAREGIVER |
(Check all that apply) |
|
|
|
|
|
STATUS |
A caregiver is unable to continue in caring |
|
|
||
|
|
|
|
|||
|
|
the health of the caregiver makes it difficult to continue |
|
a. |
||
|
|
Primary caregiver is not satisfied with support received from family |
|
b. |
||
|
|
and friends (e.g., other children of client) |
|
|||
|
|
|
c. |
|||
|
|
Primary caregiver expresses feelings of distress, anger or depression |
||||
|
|
NONE OF ABOVE |
|
d. |
||
|
|
|
|
|
||
3. |
EXTENT OF |
For instrumental and personal activities of daily living received over the |
||||
|
INFORMAL |
LAST 7 DAYS, indicate extent of help from family, friends, and |
|
|
|
|
|
neighbors |
HOURS |
||||
|
HELP |
|||||
|
|
|
||||
|
(HOURS |
a. Sum of time across five weekdays |
|
|
|
|
|
OF CARE, |
|
|
|
||
|
|
|
|
|
|
|
|
ROUNDED) |
b. Sum of time across two weekend days |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
2.MOOD Mood indicators have become worse as compared to status of 90
DECLINE days ago (or since last assessment if less than 90 days) |
|
0. No |
1. Yes |
3.BEHAVIORAL Instances when client exhibited behavioral symptoms. If EXHIBITED, ease of SYMPTOMS altering the symptom when it occurred.
0.Did not occur in last 3 days
1.Occurred, easily altered
2.Occurred, not easily altered
a.
b.VERBALLY ABUSIVE BEHAVIORAL
c.PHYSICALLY ABUSIVE BEHAVIORAL
d.SOCIALLY INAPPROPRIATE/DISRUPTIVE BEHAVIORAL SYMP-
e.RESISTS
4.CHANGES IN Behavioral symptoms have become worse or are less well tolerated BEHAVIOR by family as compared to 90 DAYS AGO (or since last assessment if
SYMPTOMS less than 90 days) |
|
0. No, or no change in behavioral symptoms |
1. Yes |
SECTION F. SOCIAL FUNCTIONING
1.INVOLVE- a. At ease interacting with others (e.g., likes to spend time with others)
MENT |
0. At ease |
1. Not at ease |
|
b. Openly expresses conflict or anger with family/friends |
|
|
0. No |
1. Yes |
2.CHANGE IN As compared to 90 DAYS AGO (or since last assessment if less than
SOCIAL 90 days ago), decline in the client's level of participation in social,
ACTIVITIES religious, occupational or other preferred activities. IF THERE WAS A |
|
DECLINE, client distressed by this fact |
|
0. No decline |
|
1. Decline, not distressed |
|
2. Decline, distressed |
|
3. ISOLATION a. Length of time client is alone during the day (morning and afternoon) |
|
0. Never or hardly ever |
|
1. About one hour |
|
2. Long periods of |
|
3. All of the time |
|
b. Client says or indicates that he/she feels lonely |
|
0. No |
1. Yes |
SECTION G. INFORMAL SUPPORT SERVICES
SECTION H. PHYSICAL FUNCTIONING:
•IADL PERFORMANCE IN 7 DAYS
•ADL PERFORMANCE IN 3 DAYS
1.IADL SELF
(A)IADL SELF PERFORMANCE CODE (Code for client's performance during LAST 7 DAYS)
0.
1.SOME
2.FULL
3.BY
8.ACTIVITY DID NOT OCCUR
(B)IADL DIFFICULTY CODE How difficult it is (or would it be) for client to do
activity on ownPerformance
0.NO DIFFICULTY
1.SOME
2.GREAT
a.MEAL
b.ORDINARY
c.MANAGING
d.MANAGING
e.PHONE
f.
g.
2.ADL
0.
1.SETUP HELP
2.
1.
TWO KEY
INFORMAL HELPERS
Primary (A)
and
Secondary
(B)
NAME OF PRIMARY AND SECONDARY HELPERS
a. (Last/Family Name) |
b. (First) |
|
||
|
|
|
|
|
c. (Last/Family Name) |
d. (First) |
|
||
|
|
|
|
|
|
|
|
(A) |
(B) |
|
|
|
PrIm |
Secn |
|
|
|
|
|
e. Lives with client |
|
|
|
|
0. Yes |
1. No |
2. No such helper [skip other items in |
|
|
|
|
the appropriate column] |
|
|
f.Relationship to client
0. Child or
1. Spouse |
3. Friend/neighbor |
|
|
|
|
|
|
Areas of help: |
0. Yes |
1. No |
|
|
|
|
|
g. — Advice or emotional support h. — IADL care
i. — ADL care
2 times (for a total of 3 or more episodes of help or supervision)
3.LIMITED
4.EXTENSIVE
—
—Full performance by another during part (but not all) of last 3 days
5.MAXIMAL
6.TOTAL
8. ACTIVITY DID NOT OCCUR (regardless of ability)
2. |
a. MOBILITY IN |
positioning body while in bed. |
b. |
standing position. |
c. LOCOMOTION IN |
d. LOCOMOTION OUTSIDE OF |
chair] |
e. DRESSING UPPER |
wear) above the waist, includes prostheses, orthotics, fasteners, pullovers, etc. |
f. DRESSING LOWER |
wear) from the waist down, includes prostheses, orthotics, belts, pants, skirts, shoes, |
and fasteners |
3.BOWEL CONTI- NENCE
In LAST 7 DAYS, control of bowel movement (with appliance or bowel continence program if employed)
1.CONTINENT WITH
2.USUALLY
3.OCCASIONALLY
4.FREQUENTLY
8.DID NOT
g. |
h. TOILET |
on/off toilet, cleaning self after toilet use or incontinent episode, changing pad, managing |
any special devices required (ostomy or catheter), and adjusting clothes. |
i . PERSONAL
j .
3.ADLDECLINE ADL status has become worse (i.e., now more impaired in self perfor- mance) as compared to status 90 days ago (or since last assessment
|
|
if less than 90 days) |
|
|
|
|
|
|
|
|
|
|
|
0. No |
1. Yes |
|
|
4. |
PRIMARY |
0. No assistive device |
3. Scooter (e.g., Amigo) |
|
|
|
MODES OF |
1. Cane |
4. Wheelchair |
|
|
|
LOCOMO- |
2. Walker/crutch |
8. ACTIVITY DID NOT OCCUR |
|
|
|
TION |
a. Indoors |
|
|
|
|
|
|
|
|
|
|
|
b. Outdoors |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
5. |
STAIR |
In the last 3 days, how client went up and down stairs (e.g., single or |
|
||
|
CLIMBING |
multiple steps, using handrail as needed) |
|
||
|
|
0. Up and down stairs without help |
|
||
|
|
1. Up and down stairs with help |
|
||
|
|
2. Not go up and down stairs |
|
||
|
|
|
|
|
|
6. |
STAMINA |
a. In a typical week, during the LAST 30 DAYS (or since last assess- |
|
|
|
|
|
ment), code the number of days client usually went out of the house |
|
|
|
|
|
or building in which client lives (no matter how short a time period ) |
|
|
|
|
|
0. Every day |
2. 1 day a week |
|
|
|
|
1. |
3. No days |
|
|
|
|
b. Hours of physical activities in the last 3 days (e.g., walking, cleaning |
|
|
|
|
|
|
|
||
|
|
house, exercise) |
|
|
|
|
|
0. Two or more hours |
1. Less than two hours |
|
|
|
|
|
|
||
|
7.FUNCTIONAL |
Client believes he/she capable of increased functional independence |
|
|
|
|
POTENTIAL |
(ADL, IADL, mobility) |
|
|
a. |
|
|
|
|
|
|
|
|
Caregivers believe client is capable of increased functional indepen- |
|
|
|
|
|
dence (ADL, IADL, mobility) |
|
b. |
|
|
|
Good prospects of recovery from current disease or conditions, im- |
|
|
|
|
|
proved health status expected |
|
c. |
|
|
|
NONE OF ABOVE |
|
|
d. |
SECTION I. CONTINENCE IN LAST 7 DAYS
1. BLADDER |
a. In LAST 7 DAYS control of urinary bladder function (with appliances |
CONTI- |
such as catheters or incontinence program employed) |
NENCE |
dribbles, volume insufficient to soak through underpants] |
0.CONTINENT
1.CONTINENTWITH
2.USUALLY
3.OCCASIONALLY
4.FREQUENTLY
5.
8. DID NOT OCCUR
b.Worsening of bladder incontinence as compared to status 90 DAYS AGO (or since last assessment if less than 90 days)
0. No1. Yes
2. |
BLADDER |
(Check all that apply in LAST 7 DAYS) |
|
|
DEVICES |
Use of pads or briefs to protect against wetness |
a. |
|
|
||
|
|
Use of an indwelling urinary catheter |
b. |
|
|
|
|
|
|
NONE OF ABOVE |
c. |
|
|
|
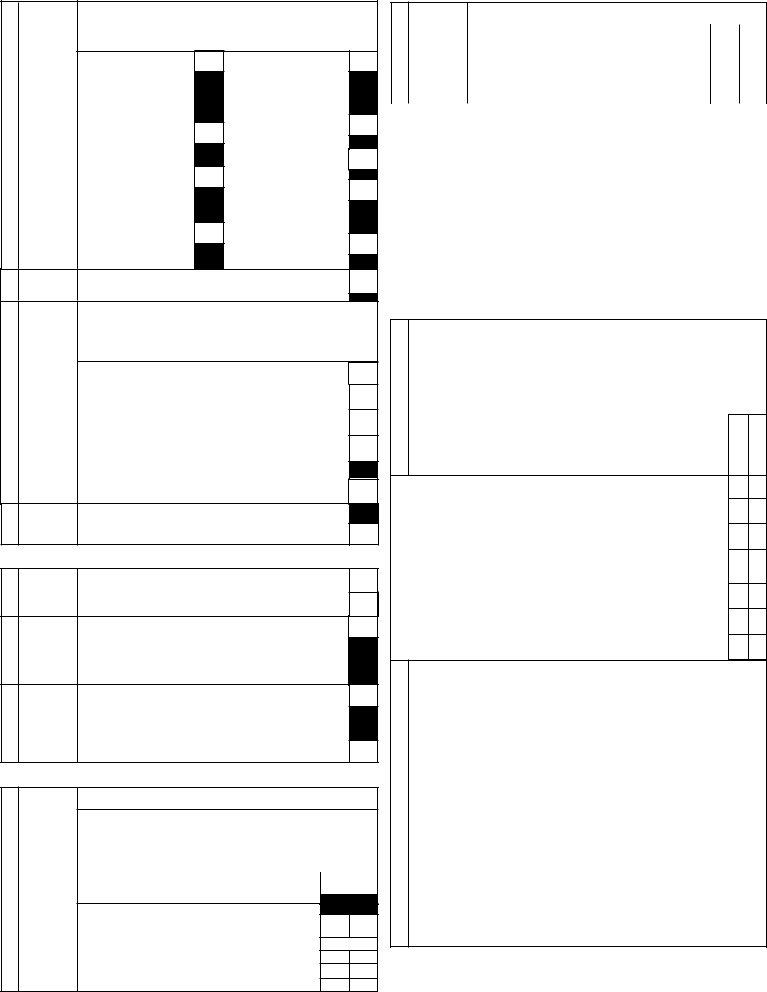
SECTION J. DISEASE DIAGNOSES
Disease/infection that doctor has indicated is present and affects client's status, requires treat- ment, or symptom management. Also include if disease is monitored by a home care professional or is the reason for a hospitalization in LAST 90 DAYS (or since last assessment if less than 90 days)
[blank]. Not present
1.
2.
[If no disease in list, check J1ac, None of Above]
1. |
DISEASES |
HEART/CIRCULATION |
|
p. Osteoporosis |
|
|
|
||||||||
|
|
a. Cerebrovascular accident |
|
SENSES |
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
(stroke) |
|
q. Cataract |
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|||||||
|
|
b. Congestive heart failure |
|
r. Glaucoma |
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|||||||
|
|
c. Coronary artery disease |
|
|
PSYCHIATRIC/MOOD |
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|||||||
|
|
d. Hypertension |
|
|
s. Any psychiatric diagnosis |
|
|
|
|||||||
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|||||||
|
|
e. Irregularly irregular pulse |
|
|
INFECTIONS |
|
|
|
|||||||
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|||||||
|
|
f. Peripheral vascular disease |
|
|
t. HIV infection |
|
|
|
|||||||
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|||||||
|
|
NEUROLOGICAL |
|
|
u. Pneumonia |
|
|
|
|||||||
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|||||||
|
|
g. Alzheimer's |
|
|
v. Tuberculosis |
|
|
|
|||||||
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|||||||
|
|
h. Dementia other than |
|
|
w. Urinary tract infection (in |
|
|
|
|||||||
|
|
|
|
|
|
|
|||||||||
|
|
Alzheimer's disease |
|
|
|
|
|
||||||||
|
|
|
|
LAST 30 DAYS) |
|
|
|
||||||||
|
|
i . Head trauma |
|
|
|
|
|
||||||||
|
|
|
|
OTHER DISEASES |
|
|
|
||||||||
|
|
|
|
|
|
|
|||||||||
|
|
j . Hemiplegia/hemiparesis |
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|||||||||
|
|
|
|
x. |
|
|
|
||||||||
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|||||||
|
|
k. Multiple sclerosis |
|
|
not including skin cancer |
|
|
|
|||||||
|
|
l . Parkinsonism |
|
|
y. Diabetes |
|
|
|
|||||||
|
|
|
|
|
|
|
|||||||||
|
|
|
|
z . Emphysema/COPD/asthma |
|
|
|
||||||||
|
|
|
|
|
|
|
|||||||||
|
|
m.Arthritis |
|
|
aa. Renal Failure |
|
|
|
|||||||
|
|
|
|
|
|
|
|||||||||
|
|
n. Hip fracture |
|
|
ab.Thyroid disease (hyper or |
|
|
|
|||||||
|
|
|
|
|
|
|
|||||||||
|
|
o. Other fractures (e.g., wrist, |
|
|
hypo) |
|
|
|
|||||||
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
vertebral) |
|
|
ac. NONE OF ABOVE |
ac. |
|||||||||
2. |
OTHER |
a. |
|
|
|
|
|
|
• |
|
|
|
|||
|
CURRENT |
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
OR MORE |
b. |
|
|
|
|
|
|
• |
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
||||||
|
DETAILED |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
DIAGNOSES |
c. |
|
|
|
|
|
|
• |
|
|
|
|||
|
AND |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CODES |
d. |
|
|
|
|
|
|
• |
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
SECTION K. HEALTH CONDITIONS AND PREVENTIVE HEALTH |
|
|
|
||||||||||||
|
MEASURES |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
||||||
1. |
PREVENTIVE |
(Check all that |
|
|
|
||||||||||
|
HEALTH |
Blood pressure measured |
|
|
|
|
|
|
|
|
a. |
||||
|
(PAST TWO |
|
|
|
|
|
|
|
|
||||||
|
Received influenza vaccination |
|
|
|
|
|
|
|
b. |
||||||
|
YEARS) |
|
|
|
|
|
|
|
|||||||
|
|
Test for blood in stool or screening endoscopy |
c. |
||||||||||||
|
|
IF FEMALE: Received breast examination or mammography |
d. |
||||||||||||
|
|
NONE OF ABOVE |
|
|
|
|
|
|
|
|
e. |
|
|||
|
PROBLEM |
(Check all that were present on at least 2 of the last 3 days) |
|
|
|
||||||||||
|
CONDITIONS |
Diarrhea |
|
Loss of appetite |
|
|
|
|
|||||||
|
PRESENT ON |
a. |
|
d. |
|||||||||||
|
2 OR MORE |
Difficulty urinating or urinating |
|
|
|
|
|
|
|
|
|||||
|
|
|
Vomiting |
|
|
|
|||||||||
|
DAYS |
3 or more times at night |
|
b. |
e. |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
Fever |
c. |
NONE OF ABOVE |
f. |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
||||
3. |
PROBLEM |
(Check all present at any point during last 3 days) |
|
|
|
||||||||||
|
CONDITIONS |
PHYSICAL HEALTH |
|
Shortness of breath |
e. |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
Chest pain/pressure at rest or |
|
|
MENTAL HEALTH |
|
|
|
|||||||
|
|
on exertion |
|
a. |
Delusions |
f. |
|||||||||
|
|
|
|
|
|||||||||||
|
|
No bowel movement in 3 days |
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
b. |
Hallucinations |
g. |
||||||||||
|
|
Dizziness or lightheadedness |
|
c. |
NONE OF ABOVE |
||||||||||
|
|
|
h. |
||||||||||||
|
|
Edema |
|
d. |
|
|
|
|
|
|
|
|
|
|
|
4. |
PAIN |
a. Frequency with which client complains or shows evidence of pain |
|||||
|
|
0. No pain (score |
2. Daily - one period |
||||
|
|
1. Less than daily |
|
3. Daily - multiple periods |
|
|
|
|
|
|
|
(e.g., morning and evening) |
|
||
|
|
b. Intensity of pain |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
0. No pain |
2. Moderate |
4. Times when pain is horrible |
|||
|
|
1. Mild |
3. Severe |
or excruciating |
|
|
|
|
|
|
|
|
|||
|
|
c. From client's point of view, pain intensity disrupts usual activities |
|||||
|
|
0. No |
1. Yes |
|
|
|
|
|
|
d. Character of pain |
|
|
|
|
|
|
|
0. No pain |
1. Localized - single site |
2. Multiple sites |
|
||
|
|
e. From client's point of view, medications adequately control pain |
|||||
|
|
0. Yes or no pain |
1. Medications do not |
2. Pain present, |
|||
|
|
|
adequately control pain |
medication not |
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
taken |
|
|
|
|
|
|
|
|
|
|
5.FALLS Number of times fell in LAST 90 DAYS (or since last assessment if FREQUENCY less than 90 days) If none, code "0"; if more than 9, code "9"
6. |
DANGER OF |
(Code for danger of falling) |
|
|
|
FALL |
0. No |
1. Yes |
|
|
|
|
|
|
|
|
a. Unsteady gait |
|
|
|
|
b. Client limits going outdoors due to fear of falling (e.g., stopped |
|
|
|
|
|
||
|
|
using bus, goes out only with others) |
|
|
|
|
|
|
|
7. |
LIFE STYLE |
(Code for drinking or smoking) |
|
|
|
(Drinking/ |
0. No |
1. Yes |
|
|
Smoking) |
|
|
|
a. In the LAST 90 DAYS (or since last assessment if less than 90 days), |
|
|||
|
|
|
||
|
|
client felt the need or was told by others to cut down on drinking, or |
|
|
|
|
others were concerned with client's drinking |
|
|
|
|
b. In the LAST 90 DAYS (or since last assessment if less than 90 days), |
|
|
|
|
|
||
|
|
client had to have a drink first thing in the morning to steady nerves |
|
|
|
|
(i.e., an "eye opener") or has been in trouble because of drinking |
|
|
|
|
c. Smoked or chewed tobacco daily |
|
|
8.HEALTH (Check all that apply)
STATUS |
Client feels he/she has poor health (when asked) |
a. |
|
INDICATORS |
|||
Has conditions or diseases that make cognition, ADL, mood, or |
|
||
|
|
||
|
behavior patterns unstable (fluctuations, precarious, or deteriorating) |
b. |
|
|
Experiencing a |
c. |
|
|
Treatments changed in LAST 30 DAYS (or since last assessment if |
|
|
|
less than 30 days) because of a new acute episode or condition |
d. |
|
|
Prognosis of less than six months to |
|
|
|
client or client's family that client has |
e. |
|
|
NONE OF ABOVE |
f. |
9.OTHER (Check all that apply)
STATUS |
Fearful of a family member or caregiver |
a. |
|
INDICATORS |
|||
Unusually poor hygiene |
b. |
||
|
|||
|
|
||
|
Unexplained injuries, broken bones, or burns |
c. |
|
|
|
||
|
Neglected, abused, or mistreated |
d. |
|
|
|
||
|
Physically restrained (e.g., limbs restrained, used bed rails, |
|
|
|
constrained to chair when sitting) |
e. |
|
|
NONE OF ABOVE |
f. |
SECTION L. NUTRITION/HYDRATION STATUS
1. |
WEIGHT |
(Code for weight items) |
1. Yes |
|
|
|
|
|
0. No |
|
|
|
|
|
a. Unintended weight loss of 5% or more in the LAST 30 DAYS [or 10% |
|
|
|
|
|
or more in the LAST 180 DAYS] |
|
|
|
|
|
|
|
|
|
|
|
b. Severe malnutrion (cachexia) |
|
|
|
|
|
c. Morbid obesity |
|
|
|
|
|
|
|
|
2. |
CONSUMP- |
(Code for consumption) |
|
|
|
0. No |
1. Yes |
|
|||
|
TION |
|
|||
|
|
|
|
||
|
|
|
a. In at least 2 of the last 3 days, ate one or fewer meals a day |
|
|
|
|
|
|
|
|
|
|
|
b. In last 3 days, noticeable decrease in the amount of food client |
||
|
|
|
usually eats or fluids usually consumes |
||
c. Insufficient
3 days
d.Enteral tube feeding
3.SWALLOWING 0.
1.REQUIRES DIET MODIFICATION TO SWALLOW SOLID FOODS (mechanical diet or able to ingest specific foods only)
2.REQUIRES MODIFICATION TO SWALLOW SOLID FOODS AND LIQUIDS (puree, thickened liquids)
3.COMBINED ORAL AND TUBE FEEDING
4.NO ORAL INTAKE (NPO)
SECTION M. DENTAL STATUS (ORAL HEALTH)
1. |
ORAL |
(Check all that apply) |
|
|
STATUS |
Problem chewing (e.g., poor mastication, immobile jaw, surgical resec- |
|
|
|
||
|
|
|
|
|
|
tion, decreased sensation/motor control, pain while eating) |
a. |
|
|
|
|
|
|
Mouth is "dry" when eating a meal |
b. |
|
|
Problem brushing teeth or dentures |
c. |
|
|
NONE OF ABOVE |
d. |
SECTION N. SKIN CONDITION
1. |
SKIN |
Any troubling skin conditions or changes in skin condition (e.g., burns, |
|
|||
|
PROBLEMS |
bruises, rashes, itchiness, body lice, scabies) |
|
|||
|
|
0. No |
1. Yes |
|
|
|
2. |
ULCERS |
Presence of an ulcer anywhere on the body. Ulcers include any area of |
|
|||
|
(Pressure/ |
persistent skin redness (Stage 1); partial loss of skin layers (Stage 2); |
|
|||
|
deep craters in the skin (Stage 3); breaks in skin exposing muscle or |
|
||||
|
Stasis) |
|
||||
|
bone (Stage 4).[Code 0 if no ulcer,otherwise record the highest ulcer |
|
||||
|
|
|
||||
|
|
stage (Stage |
|
|
|
|
|
|
|
|
|
|
|
|
|
a. Pressure |
|
|||
|
|
resulting in damage of underlying tissues |
|
|||
|
|
b. Stasis |
|
|||
|
|
|
||||
|
|
extremities |
|
|
|
|
3. |
OTHERSKIN |
(Check all that apply) |
|
|
|
|
|
PROBLEMS |
Burns (second or third |
|
|
Surgical wound |
|
|
|
|
|
|||
|
REQUIRING |
|
|
d. |
||
|
degree) |
|
|
|||
|
TREATMENT |
|
|
|
||
|
|
|
a. |
Corns, calluses, structural prob- |
|
|
|
|
|
|
|
||
|
|
Open lesions other than |
|
|
|
|
|
|
|
|
lems, infections, fungi |
e. |
|
|
|
ulcers, rashes, cuts (e.g., |
|
|||
|
|
|
|
|||
|
|
|
|
|
||
|
|
cancer) |
|
b. |
NONE OF ABOVE |
f. |
|
|
|
|
|||
|
|
Skin tears or cuts |
|
c. |
|
|
|
|
|
|
|
|
|
4. |
HISTORY OF |
Client previously had (at any time) or has an ulcer anywhere on the |
|
|||
|
RESOLVED |
body |
|
|
|
|
|
|
|
|
|
|
|
|
PRESSURE |
0. No |
1. Yes |
|
|
|
|
ULCERS |
|
|
|||
|
|
|
|
|
|
|
5. |
WOUND/ |
(Check for formal care in LAST 7 DAYS) |
|
|||
|
ULCER |
Antibiotics, systemic or topical |
|
a. |
||
|
CARE |
|
||||
|
|
|
|
|
||
|
|
Dressings |
|
|
|
b. |
|
|
|
|
|
|
|
|
|
Surgical wound care |
|
|
|
c. |
|
|
|
|
|
|
|
|
|
Other wound/ulcer care (e.g., pressure relieving device, nutrition, turn- |
|
|||
|
|
ing, debridement) |
|
|
|
d. |
|
|
|
|
|
|
|
|
|
NONE OF ABOVE |
|
|
|
e. |
SECTION O. ENVIRONMENTAL ASSESSMENT
1. |
HOME |
Lighting in evening (including inadequate or no lighting in living room, |
|
|
|
ENVIRON- |
sleeping room, kitchen, toilet, corridors) |
a. |
|
|
MENT |
Flooring and carpeting (e.g., holes in floor, electric wires where client |
|
|
|
[Check any |
|
||
|
walks, scatter rugs) |
|
|
|
|
of following |
|
b. |
|
|
|
|
||
|
that make |
Bathroom and toiletroom (e.g., |
|
|
|
home |
|
||
|
rails though needed, slippery bathtub, outside toilet) |
c. |
||
|
environment |
|||
|
hazardous or |
Kitchen (e.g., dangerous stove, inoperative refrigerator, infestation by |
|
|
|
uninhabit- |
rats or bugs) |
|
d. |
|
able (if none |
|
||
|
apply, check |
Heating and cooling (e.g., too hot in summer, too cold in winter, wood |
|
|
|
NONE OF |
|
||
|
stove in a home with an asthmatic) |
e. |
||
|
ABOVE; if |
|||
|
|
|
||
|
|
|
|
|
|
temporarily |
Personal safety (e.g., fear of violence, safety problem in going to |
|
|
|
in institution, |
mailbox or visiting neighbors, heavy traffic in street) |
f. |
|
|
base |
|
|
|
|
Access to home (e.g., difficulty entering/leaving home) |
|
||
|
assessment |
g. |
||
|
on home |
Access to rooms in house (e.g., unable to climb stairs) |
h. |
|
|
visit)] |
|||
|
|
NONE OF ABOVE |
|
i. |
2. |
LIVING |
a. As compared to 90 DAYS AGO (or since last assessment), client |
|
|
|
ARRANGE- |
now lives with other |
|
|
|
other moved in with client |
|
||
|
MENT |
|
||
|
0. No |
1. Yes |
|
|
|
|
|
||
|
|
b. Client or primary caregiver feels that client would be better off in |
|
|
|
|
|
||
|
|
another living environment |
|
|
|
|
0. No 1. Client only |
2. Caregiver only 3. Client and caregiver |
|
|
|
|
||
|
|
|
|
|
SECTION P. SERVICE UTILIZATION (IN LAST 7 DAYS)
1. |
FORMAL |
Extent of care or care management in LAST 7 DAYS (or since last |
|
|
||||
|
CARE |
assessment if less than 7 days) involving |
(A) |
|
(B) |
(C) |
||
|
|
|
|
|||||
|
(Minutes |
|
# of |
|
|
|
|
|
|
|
Days |
Hours |
Mins |
||||
|
rounded to |
a. Home health aides |
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
even 10 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
minutes) |
b. Visiting nurses |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c. Homemaking services |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
d. Meals |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
e. Volunteer services |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
f. Physical therapy |
|
|
|
|
|
|
|
|
g. Occupational therapy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
h. Speech therapy |
|
|
|
|
|
|
|
|
i. Day care or day hospital |
|
|
|
|
|
|
|
|
j. Social worker in home |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2. SPECIAL |
Special treatments, therapies, and programs received or scheduled during the |
|
TREAT- |
LAST 7 DAYS (or since last assessment if less than 7 days) and adherence to |
|
MENTS, |
the required schedule. Includes services received in the home or on an |
|
THERAPIES, |
outpatient basis. |
|
PROGRAMS |
[Blank]. Not applicable |
2. Scheduled, partial adherence |
|
||
1.Scheduled, full adherence as prescribed 3. Scheduled, not received [If no treatments provided, check NONE OF ABOVE P2aa]
|
RESPIRATORYTREATMENTS |
|
o. Occupational therapy |
|
||
|
|
|
p. Physical therapy |
|
||
|
a. Oxygen |
|
|
|||
|
b. Respirator for assistive |
|
PROGRAMS |
|
||
|
|
|
||||
|
|
breathing |
|
q. Day center |
|
|
|
|
|
|
|
||
|
c. All other respiratory treat- |
|
r. |
Day hospital |
|
|
|
|
ments |
|
s. Hospice care |
|
|
|
|
|
|
|||
|
OTHERTREATMENTS |
|
|
|||
|
|
t. Physician or clinic visit |
|
|||
|
|
|||||
|
d. Alcohol/drug treatment |
|
|
|||
|
|
|
||||
|
|
u. Respite care |
|
|||
|
|
|||||
|
|
program |
|
|
||
|
e. Blood transfusion(s) |
|
SPECIAL PROCEDURES DONE |
|
||
|
|
IN HOME |
|
|||
|
|
|
|
|
||
|
f. |
Chemotherapy |
|
|
||
|
|
v. Daily nurse monitoring (e.g., |
|
|||
|
|
|||||
|
g. Dialysis |
|
|
|||
|
|
|
||||
|
|
|
EKG, urinary output) |
|
||
|
h. IV infusion - central |
|
w. Nurse monitoring less than |
|
||
|
|
|
||||
|
|
|
|
|
||
|
i . |
IV infusion - peripheral |
|
|
daily |
|
|
j . |
Medication by injection |
|
x. Medical alert bracelet or elec- |
|
|
|
|
|
||||
|
k. Ostomy care |
|
|
tronic security alert |
|
|
|
|
|
|
|||
|
|
y. |
Skin treatment |
|
||
|
l . |
Radiation |
|
|
||
|
|
|
||||
|
|
|
|
|
||
|
m. Tracheostomy care |
|
z . |
Special diet |
|
|
|
|
|
||||
|
|
|
|
|
||
|
THERAPIES |
|
aa. NONE OF ABOVE |
aa. |
||
|
|
|||||
|
|
|
|
|||
|
n. Exercise therapy |
|
|
|
|
|
|
|
|
|
|
|
|
3.MANAGE- Management codes:
MENT OF |
0. Not used |
|
|
EQUIPMENT |
1. Managed on own |
|
|
(In Last 3 |
2. Managed on own if laid out or with verbal reminders |
||
Days) |
3. Partially performed by others |
|
|
|
4. Fully performed by others |
|
|
|
|
|
|
|
a. Oxygen |
|
c. Catheter |
|
b. IV |
|
d. Ostomy |
|
|
||
4.VISITS IN Enter 0 if none, if more than 9, code "9" LAST90
DAYS |
a. Number of times ADMITTED TO HOSPITAL with an overnight stay |
OR |
|
SINCELAST |
b. Number of times VISITED EMERGENCY ROOM without an overnight |
ASSESSMENT |
stay |
c. EMERGENT
5.TREATMENT Any treatment goals that have been met in the LAST 90 DAYS (or since
GOALS last assessment if less than 90 days)
0. No |
1. Yes |
6.OVERALL Overall self sufficiency has changed significantly as compared to
CHANGE IN status of 90 DAYS AGO (or since last assessment if less than 90 days) |
|
CARE NEEDS 0. No change 1. |
2. Deteriorated— |
fewer supports |
receives more support |
7.TRADE OFFS Because of limited funds, during the last month, client made
0. No |
1. Yes |
SECTION Q. MEDICATIONS
1.NUMBER OF Record the number of different medicines (prescriptions and over the
MEDICA- |
counter), including eye drops, taken regularly or on an occasional basis |
|
in the LAST 7 DAYS (or since last assessment)[If none, code "0", if |
||
TIONS |
||
more than 9, code "9"] |
||
|
2.RECEIPT OF Psychotropic medications taken in the LAST 7 DAYS (or since last PSYCHO- assesssment)
TROPIC applies to the following categories] |
0. No |
1. Yes |
||
MEDICATION |
|
|
|
|
a. Antipsychotic/neuroleptic |
|
c. Antidepressant |
||
|
b. Anxiolytic |
|
d. Hypnotic |
|
|
|
|
||
|
|
|
|
|
3.MEDICAL Physician reviewed client's medications as a whole in LAST 180 DAYS OVERSIGHT (or since last assessment)
0.Discussed with at least one physician (or no medication taken)
1.No single physician reviewed all medications
4.COMPLI- Compliant all or most of time with medications prescribed by physician
ANCE/ (both during and between therapy visits) in LAST 7 DAYS |
|
ADHERENCE |
|
WITH |
0. Always compliant |
MEDICA- |
1. Compliant 80% of time or more |
TIONS |
2. Compliant less than 80% of time, including failure to purchase |
|
prescribed medications |
3.NO MEDICATIONS PRESCRIBED
=When box blank, must enter number or letter a. = When letter in box, check if condition applies
©Copyright interRAI, 1994,1996, 1997, 1999
5.LIST OF ALL List prescribed and nonprescribed medications taken in LAST 7 DAYS (or since MEDICATIONS last assessment)
a.Name and
b.Form: Code the route of Administration using the following list:
1. |
By mouth (PO) |
5. Subcutaneous (SQ) |
9. Enteral tube |
||||
2. |
Sub lingual (SL) |
6. Rectal (R) |
10. Other |
||||
3. |
Intramuscular (IM) |
7. |
Topical |
|
|
||
4. |
Intravenous (IV) |
8. Inhalation |
|
||||
|
c. Number |
||||||
|
the medication is given |
|
|
|
|
||
|
d. Freq: Code the number of times per day, week, or month the medication is |
||||||
|
administered using the following list: |
|
|
||||
|
PRN. As necessary |
|
5D. |
Five times daily |
|||
|
QH. |
|
Every hour |
|
QOD. Every other day |
||
|
Q2H. |
Every two hours |
|
QW. |
Once each wk |
|
|
|
Q3H. |
Every three hours |
|
2W. |
Two times every week |
||
|
Q4H. |
Every four hours |
|
3W. |
Three times every week |
||
|
Q6H. |
Every six hours |
|
4W. |
Four times each week |
||
|
Q8H. |
Every eight hours |
|
5W. |
Five times each week |
||
|
QD. |
|
Once daily |
|
6W. |
Six times each week |
|
|
BID. |
|
Two times daily |
|
1M. |
Once every month |
|
|
|
|
(includes every 12 hrs) |
2M. |
Twice every month |
||
|
TID. |
|
Three times daily |
|
C. |
Continuous |
|
|
QID. |
|
Four times daily |
|
O. |
Other |
|
|
|
|
|
|
|
|
|
a. Name and Dose |
|
|
|
|
b. Form |
c. Number d. Freq. |
|
|
|
|
|
|
|
|
Taken |
a._________________________________________________________________________
b._________________________________________________________________________
c._________________________________________________________________________
d._________________________________________________________________________
e._________________________________________________________________________
f._________________________________________________________________________
g._________________________________________________________________________
h._________________________________________________________________________
i._________________________________________________________________________
j._________________________________________________________________________
k._________________________________________________________________________
SECTION R. ASSESSMENT INFORMATION
1.SIGNATURES OF PERSONS COMPLETINGTHE ASSESSMENT:
a.Signature of Assessment Coordinator
b.Title of Assessment Coordinator
c.Date Assessment Coordinator signed as complete
Month |
Day |
Year |
|
|
|
|
|
|
|
d. Other Signatures |
Title |
Sections |
Date |
|
|
|
|
|
|
e. |
|
|
Date |
|
|
|
|
|
|
f. |
|
|
Date |
|
|
|
|
|
|
g. |
|
|
Date |
|
|
|
|
|
|
h. |
|
|
Date |
|
|
|
|
|
|
i . |
|
|
Date |
|
* Country specific |
|
Request for Services
Type of clinical eligibility determination all requested services.
Service(s) requested |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
Home and community |
|||||||||||||||||
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
based services (HCBS) waiver |
|||||||
|
|
Adult day health (ADH) |
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
Adult foster care (AFC) |
|
|
|
|
Program for |
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
for the Elderly (PACE) |
|||||||||
|
|
Group adult foster care (GAFC) |
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
Other |
|||||||
Date
Nursing facility use only
Conversion
Continued stay
Short term review
Transfer NF to NF
Retrospective
Member information
Member/applicant
Last name |
First name |
Telephone
Address
City
Zip
Check one |
|
|
|
|
|
|
|
|||
|
MassHealth |
|
|
MassHealth |
|
|
GAFC/ |
|||
|
|
|
||||||||
|
|
|
||||||||
|
member |
|
|
application pending |
|
|
Assisted living residence |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
MassHealth ID number |
|
Date application iled |
|
|
Date |
|||
Next of kin/Responsible party |
|
|
|
|
|
|
|
|||
Last name |
|
First name |
Telephone
Address
City
Zip
Physician
Last name |
|
First name |
Telephone
Address
City
Zip
Screening for mental illness, mental retardation, and developmental disability
Does the member/applicant have any of the following diagnoses/conditions? Check all that apply.
|
Mental illness |
|
Specify: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
Mental retardation without related condition |
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
Developmental disability with related condition that occurred prior to age 22. |
Check all that apply. |
|
|
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
Autism |
|
|
|
|
|
|
|
|
Deafness/severe hearing impairment |
|
Multiple sclerosis |
|
|
|
|
Severe learning disability |
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
Blindness/severe visual impairment |
Epilepsy/seizure disorder |
|
|||||||||||||||||||||||||
|
|
|
|
|
|
|
Muscular dystrophy |
|
|
|
Spina biida |
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
Cerebral palsy |
|
Head/brain injury |
|
|
|
Orthopedic impairment |
|
|
Spinal cord injury |
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
Major mental illness |
|
|
|
|
|
|
||||||||||||||||
|
|
Cystic ibrosis |
|
|
|
Speech/language impairment |
|
|
|
|
|
||||||||||||||||||
OVER |
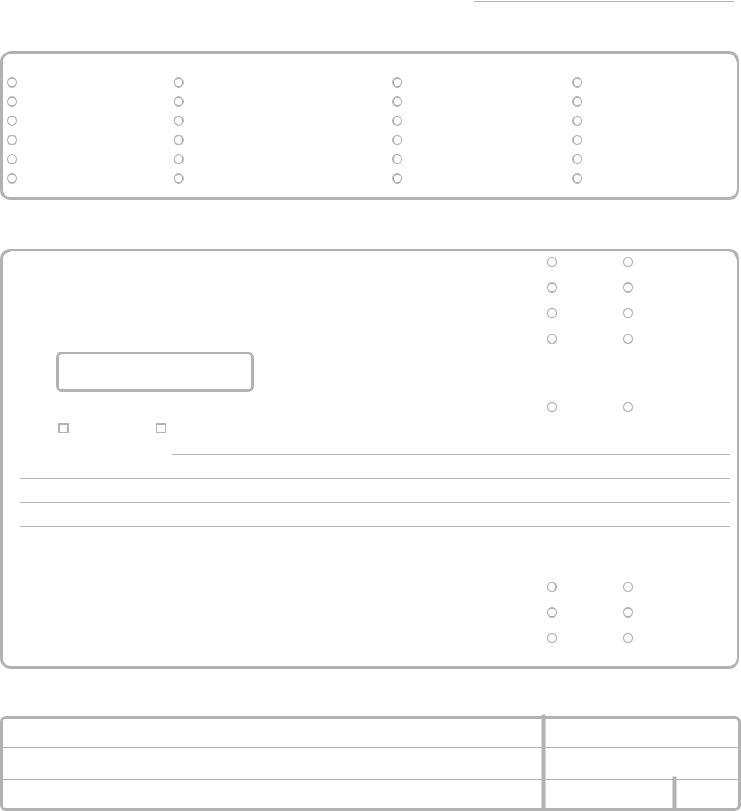
Name of member/applicant
Community services recommended
Check all that apply. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Skilled nursing |
|
|
|
|
|
|
HCBS waiver |
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Rest home |
Homemaker |
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Physical therapy |
Elderly housing |
||||||||||||||||||||||||||||
|
|
|
|
|
|
Personal emergency response system |
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
Meals |
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
Occupational therapy |
|||||||||||||||||||||||||||||
|
|
|
|
Adult foster care |
|
|
|
Adult day health |
|
|
|
Transportation |
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
Speech therapy |
|
|
|
|
|
|
Group adult foster care |
|
|
PACE |
|
|
|
Chore service |
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
Mental health services |
Home health aide |
Grocery shopping/delivery |
|||||||||||||||||||||||||||
|
|
Assisted living |
||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
Social worker services |
|||||||||||||||||||||||||||||
|
|
|
Congregate housing |
|||||||||||||||||||||||||||
|
|
|
|
|
|
Personal care/homemaker |
||||||||||||||||||||||||
|
|
|
|
|
|
|
Other: |
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Additional information
1. Is the home or apartment available for the member or applicant? |
|
|
|
|
yes |
|
no |
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
yes |
|
no |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
2. |
Is there a caregiver to assist the member in the community? |
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
yes |
|
no |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
3. |
Has the member or applicant experienced unexplained weight gain in the last 30 days? |
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
yes |
|
no |
||||
4. |
Does the member or applicant receive personal care/homemaker services? |
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
If yes: |
days per week |
|
|
hours per week |
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
yes |
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
no |
||||||||||||
5. |
Has the member or applicant experienced a signiicant change in condition in the last 30 days? |
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
If yes: |
|
|
|
|
improvement |
|
|
|
|
|
deterioration |
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Indicate the changes below.
For nursing facility requests only
1.Does the nursing facility member/applicant express an interest to remain in or return to the community?
2.Is the nursing facility stay expected to be
3.Is the nursing facility stay expected to be
Referral source Name of registered nurse completing this form
Signature |
|
|
Print name |
|
|
|
|
|
|
|
|
yes |
no |
yes |
no |
yes |
no |
Title
Name of organization
Telephone
Address
City
Zip
For community providers:
For nursing facility providers:
Attach the
Attach the most recent comprehensive MDS, current quarterly MDS, and current physician orders.